Tuberous sclerosis is the most common neurocutaneous syndrome after neurofibromatosis. Dermatologic manifestations may be the only clues the family physician has to the diagnosis of the disorder, which is also marked by childhood seizures and mental retardation. Characteristic signs of tuberous sclerosis vary widely in severity and can include hypopigmented "ash-leaf spots," fibrous plaques on the forehead, angiofibromas on the face (adenoma sebaceum), a shagreen patch on the lower back and fibromas of the nails. Computed tomographic scanning or magnetic resonance imaging reveal subependymal nodules or cortical "tubers" in the brain. Associated cardiac, retinal, renal and pulmonary pathology can increase morbidity and mortality. Genetic counseling is helpful but has limited use because of the variation in genetic expression and the frequency of new gene mutations that cause this disorder. (Am Fam Physician 2000;61:703-8,710.)
The term "tuberous sclerosis" was first used in 1880 to describe a syndrome consisting of seizures, mental retardation and facial rash in a young girl. However, this complex disorder was initially identified in 1862, and an association between seizures, mental retardation and facial angiofibromas (adenoma sebaceum), referred to as "Vogt's triad," was established in 1908.1 With recent advances in genetic research and imaging modalities, more mysteries about this fascinating disorder have been solved.
Epidemiology and Genetics
Tuberous sclerosis is an autosomal dominant disorder with almost complete penetrance but a wide range of clinical severity. The name "tuberous sclerosis" comes from "tubers" (swellings or protuberances) and areas of "sclerosis" (hardening) in the cerebral gyri that calcify with age.
The disorder affects about one in 10,000 persons in the general population and has an estimated incidence of one case per 6,000 live births.2 Thus, it is the second most common neurocutaneous syndrome after neurofibromatosis.3 Tuberous sclerosis has no predilection for gender or race.4 Affected members of the same family may be of normal intelligence, or they may be severely mentally retarded with seizures that are difficult to control.2
Genetic research has identified two tuberous sclerosis genes. One is located on chromosome 9 and the other on chromosome 16. About 68 percent of cases occur as a result of new gene mutations.2 Because of the genetic transmission and new mutations, antenatal diagnosis is difficult.
Careful examination of the parents of an affected child may differentiate between the inherited disorder and a new mutation. Thus, before it is decided that a child has a new mutation, a complete history should be obtained from the child's parents and, if possible, other relatives. Family members should also undergo a physical examination, including a full dermatologic evaluation, with ultraviolet light used to accentuate "ash-leaf spots" (so named because of their resemblance to the leaves of the European mountain ash) and dilated funduscopy used to delineate retinal phakomas (astrocytomas).
Antenatal counseling may help to reduce the transmission of tuberous sclerosis. When multiple persons in the same family have this neurocutaneous syndrome, as many as 50 percent of the offspring of affected family members will also have the disorder.5
Illustrative Case
An eight-month-old boy was brought to an emergency department because of new-onset seizures that were lasting about five minutes. The mother reported that the infant was unable to sit without support and had not attempted to crawl.
The infant's history was remarkable for delayed immunizations. The mother had missed several clinic appointments because she was busy with her other child, a two-year-old boy who was being evaluated for developmental delay. That child had been identified as having delayed speech and language ability.
The physical examination showed a sleepy, afebrile infant in no acute distress and weighing 9.1 kg (20 lb; 50th to 75th percentile). The infant was unable to sit up or hold a sitting position. Of note, an oval depigmented area about 2 cm in greatest diameter with irregular borders was present on the skin over the infant's left lateral trunk. The appearance of this area was consistent with an ash-leaf spot (Figure 1).
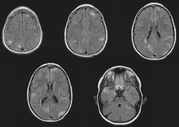
Computed tomographic (CT) scanning of the head, performed in the emergency department, demonstrated multiple calcific subependymal nodules in the infant's brain (Figure 2). A kidney sonogram, an echocardiogram and a chest radiograph were all normal. The infant was admitted to the hospital and placed on phenobarbital to control his seizures.
On further investigation, the infant's brother was found to have a superficial, oblong, hypomelanotic macule on his back. The lesion resembled the one on the infant's trunk.
The parents' histories were taken, and physical examinations were performed. The mother was of normal intelligence and had a normal physical examination. The 22-year-old father of both children had a history of childhood seizures that had been controlled with phenobarbital. He denied having any seizure activity after eight years of age. His appearance was that of a normal male. However, he had acne- like lesions along the bridge of his nose and in his nasolabial folds (Figure 3). A CT scan of the father's brain showed subependymal nodules. Further detailed physical examination revealed a flesh-colored papule in the nail bed of the third toe of the left foot, consistent with an ungual fibroma (Figure 4). He was also found to have an orange- peel-textured lesion (shagreen patch) on his lower back (Figure 5).
Neuropathology
Tuberous sclerosis is a complex of hamartomatous changes involving the brain and skin. Frequently, the disorder also involves the heart, lungs, kidneys and other organs.
Cortical tubers, or benign potato-like growths, appear along the gyri and sulci in the brain. Most easily found on magnetic resonance imaging,6 these growths are associated with seizures.7 Occasionally, a tuber blocks the foramen of Monro and causes hydrocephalus. Subependymal nodules lining the ventricles frequently calcify. The nodules sometimes can be seen on plain-film radiographs, but they are best demonstrated on CT scans.6 A radiologically confirmed cortical tuber or calcified subependymal nodule is highly suggestive of tuberous sclerosis.8
Malignant brain tumors rarely occur in patients with tuberous sclerosis. However, up to 8 percent of patients with the disorder develop subependymal giant cell astrocytomas, typically near the foramen of Monro.9 The astrocytomas may originate from a subependymal nodule.10 These well-circumscribed lesions should not be confused with the giant cell variant of glioblastoma multiforme, a malignant astrocytoma.
Rarely, the giant cell astrocytomas undergo malignant transformation.11 Characteristically, these tumors are avascular without necrosis. They contain a homogeneous population of well-differentiated astrocytes. Progression to malignancy is associated with the appearance of mitotic figures and a necrotic zone.
Clinical Syndrome
Persons with the mild form of tuberous sclerosis can lead full lives without any loss of function. In others, disabilities can be severe, with seizures, infections, tumors, renal involvement or pulmonary complications causing significant mortality. The classic clinical triad of seizures, mental retardation and facial angiofibromas is present only in persons with more severe tuberous sclerosis.
The diagnostic criteria for tuberous sclerosis were recently revised at a consensus conference. Major and minor features are listed in Table 1.12 The diagnosis of the disorder requires the presence of either two major features or one major feature and two minor features. Patients with one major feature plus one minor feature probably have tuberous sclerosis. Tuberous sclerosis should be suspected in patients who have one major feature or two or more minor features.
seizures
Tuberous sclerosis may present at birth with flexion or salaam's seizures.13 The seizures usually continue throughout life, although they transform into adult-type partial complex or tonic-clonic seizures.2
At some point, seizures affect 80 percent of patients with tuberous sclerosis.9 The seizures usually start occurring before two years of age. Intelligence is normal in one fourth of patients with seizures, but nearly all mentally retarded patients have seizures. Seizures can usually be controlled with antiepileptic medications.
dermatologic manifestations
Patients with tuberous sclerosis have several typical dermatologic findings. Facial angiofibromas are found in 75 percent of affected patients.8 These lesions appear after four years of age4 and may be mistaken for acne. Facial angiofibromas may require repeated dermal abrasion for cosmesis.
The ash-leaf spot is the earliest skin lesion in patients with tuberous sclerosis. This hypomelanotic macule is most easily visualized with a Wood's light.4 Ash-leaf spots are found at birth or in early infancy in 87 percent of patients with the disorder. By themselves, these hypomelanotic macules are not diagnostic of tuberous sclerosis because they are also relatively common in the general population.8
The shagreen patch, a thickened orange-peel-textured area of connective tissue hamartoma, is most often found on the mid to lower back. This lesion develops in 21 percent of patients with tuberous sclerosis.2 Shagreen patches may develop between two and six years of age.
Ungual fibromas are flesh-colored papules that may displace and distort the nail bed. These lesions are found in 19 percent of patients with tuberous sclerosis.2 Ungual fibromas are more prominent in adolescents and adults, and they are fairly specific to tuberous sclerosis. Patients can also have sublingual or perilingual fibromas.
cardiac manifestations
Cardiac rhabdomyomas occur in 50 percent of patients with tuberous sclerosis.14 These lesions can be detected by echocardiography. Although the rhabdomyomas are frequently asymptomatic, they may cause heart failure in infants because of outflow obstruction of one or both ventricles.11 Rhabdomyomas decrease in size with age.
ophthalmologic manifestations
Retinal phakoma, often called "mulberry lesions," are astrocytomas of the retina. The physician may first note these lesions as the absence of the normal "red reflex" in the newborn. The presence of two or more retinal phakomas is highly suggestive of tuberous sclerosis.11 The lesions occur in about 50 to 75 percent of patients with the disorder.11
A retinal phakoma may have a characteristic appearance of a large, whitish, mulberry-like multinodular lesion. The lesion can easily be mistaken for a retinoblastoma. Therefore, a diligent search for other signs of tuberous sclerosis should be made before inappropriate, unnecessary enucleation is performed.11
Patients can also have plaque-like hematomas and achromic patches on the retina. Most lesions do not cause visual changes.15
renal manifestations
Renal cysts may develop in children with tuberous sclerosis, and renal angiomyolipomas may occur in adults. Renal failure or bleeding angiomyolipomas may cause death. Pain is the most frequent clinical feature of these lesions.
An angiomyolipoma greater than 3.5 to 4 cm in diameter should be evaluated angiographically and considered for treatment. If an angiomyolipoma is smaller than 3.5 to 4 cm but is causing symptoms, the lesion should also be studied angiographically.
Given the significant morbidity of hypovolemic shock from hemorrhagic angiomyolipomas, patients with tuberous sclerosis should undergo ultrasound examination at diagnosis and serial sonography every one to three years. If an angiomyolipoma grows or becomes symptomatic, renal arterial embolization or renal-sparing surgery (i.e., enucleation or partial nephrectomy) should be considered.15
Some experts recommend CT scanning or ultrasonography every six months for asymptomatic lesions more than 3.5 to 4 cm in diameter. Annual CT scanning or ultrasonography has also been recommended for asymptomatic lesions less than 3.5 to 4 cm in diameter.16
A slightly increased incidence of renal cell carcinomas has been noted in patients with tuberous sclerosis. In a study conducted at a Mayo Clinic,2 renal cell carcinoma was present in two of 11 patients with this disorder who died of renal disease.
pulmonary manifestations
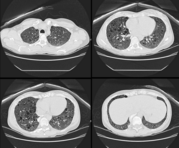
Lymphangiomyomatosis occurs in 1 to 6 percent of almost exclusively female patients with tuberous sclerosis.8 Morphologic analysis of the lungs shows multiple cyst-type lesions measuring a few millimeters in diameter.
Because lymphangiomyomatosis is often fatal and is thought to respond to progesterone and/or oophorectomy, chest radiographs should be obtained at regular intervals in all patients with tuberous sclerosis.2 Serial pulmonary function testing is also advised. Lung transplantation may be considered in patients with end-stage disease.
Final Comment
The dermatologic manifestations of tuberous sclerosis are helpful in diagnosing this disorder. Unfortunately, no specific prenatal laboratory test is available. Genetic counseling should be offered to families with affected members, even though accurate counseling remains difficult because of the variability of gene expression. When tuberous sclerosis has been inherited in the autosomal dominant form, dermatologic signs are almost universally present in one of the patient's parents.
Physicians and affected families seeking more information can contact the National Tuberous Sclerosis Association (8181 Professional Place, Suite 110, Landover, MD 20785-2226; telephone: 800-225-6872 or 301-459- 9888; fax: 301-459-0394; Web site: http:// www.ntsa.org).
REFERENCES
1. Griffiths PD, Martland TR. Tuberous sclerosis complex: the role of neuroradiology. Neuropediatrics 1997;28:244-52.
2. Stefansson K. Tuberous sclerosis [Editorial]. Mayo Clin Proc 1991;66:868-72.
3. Gutowski NJ, Murphy RP. Late onset epilepsy in undiagnosed tuberous sclerosis. Postgrad Med J 1992;68(806):970-1.
4. Thomas FB, Eisen AZ, Wolff K, Freedberg IM, Austen KF. Neurocutaneous diseases. In: Fitzpatrick TB, ed. Dermatology in general medicine. 4th ed. New York: McGraw-Hill, 1993:2255-9.
5. Simonoff E. Genetic counseling in autism and pervasive developmental disorders. J Autism Dev Disord 1998;28:447-56.
6. Roach ES. Neurocutaneous syndromes. Pediatr Clin North Am 1992;39:591-620.
7. Shepherd CW, Stephenson JB. Seizures and intellectual disability associated with tuberous sclerosis complex in the west of Scotland. Dev Med Child Neurol 1992;34:766-74.
8. Kwiatkowski DJ, Short MP. Tuberous sclerosis. Arch Dermatol 1994;130:348-54.
9. Katogal P. Epilepsy in the setting of neurocutaneous syndromes. In: Wyllie E. The treatment of epilepsy: principles and practice. 2d ed. Baltimore: Williams & Wilkins, 1996:646-53.
10. Houser OW, McLeod RA. Roentgenographic experience at the Mayo Clinic. In: Gomez MR, ed. Tuberous sclerosis. New York: Raven, 1979:27- 53.
11. Osborne JP. Diagnosis of tuberous sclerosis. Arch Dis Child 1988;63:1423-5.
12. Roach ES, Gomez MR, Northrup H. Tuberous sclerosis complex consensus conference: revised clinical diagnostic criteria. J Child Neurol 1998;13:624-8.
13. Adams RD, Victor M. Developmental diseases of the nervous system. In: Principles of neurology. 5th ed. New York: McGraw-Hill, 1993:1027- 30.
14. Haslam RH. Neurocutaneous syndromes. In: Nelson WE, Behrman RE, Kliegman RM, Arvin AM, eds. Nelson Textbook of pediatrics. 15th ed. Philadelphia: Saunders, 1996:1707.
15. Weiner DM, Ewalt DH, Roach ES, Hensle TW. The tuberous sclerosis complex: a comprehensive review. J Am Coll Surg 1998;187:548-61.
16. Oesterling JE, Fishman EK, Goldman SM, Marshall FF. The management of renal angiomyolipoma. J Urol 1986;135:1121-4.
Tuberous Sclerosis and Your Baby
What is tuberous sclerosis?
Tuberous sclerosis causes growths in the brain, eyes, heart, kidney, skin or lungs. These growths are usually benign (not cancer). The first signs may be seizures and spots on the skin. People in the same family who have tuberous sclerosis may have no learning problems or mild learning problems, or they may have serious learning problems, with seizures that are hard to control.
Tuberous sclerosis isn't common, but it isn't rare either. Up to 40,000 people in the United States have it. The disorder occurs in both sexes and in people of all races and ethnic groups.
How did my child get this disorder?
About half the time, tuberous sclerosis is passed from a parent to a child, or inherited. If one parent has tuberous sclerosis, every child born to that parent has a 50 percent chance of inheriting it.
However, in about half the children who have tuberous sclerosis, the mother and father have no signs of it. It seems that sometimes a normal gene changes (mutates) to the abnormal form that causes tuberous sclerosis.
Doctors have no test to identify a person who has the tuberous sclerosis gene if that person has no signs of it.
If parents who have one child with tuberous sclerosis want to have another child, they need to talk with their family doctor first. The family doctor can refer them to a genetic counselor or medical geneticist who can help them decide what to do.
What are the signs of tuberous sclerosis?
Your doctor may suspect tuberous sclerosis if your baby has a condition called cardiac rhabdomyomas (benign heart tumors) at birth or starts to have seizures, especially a kind of seizure called infantile spasms.
However, your doctor may not be able to tell that your child has tuberous sclerosis until these signs show up:
* White spots on the skin (called hypopigmented macules) that glow under a special lamp
* A rash on the face (called facial angiofibromas)
* A mental disability
Where can I get more information?
For support and information, you can contact this organization:
National Tuberous Sclerosis Association
8181 Professional Place, Suite 110
Landover, MD 20785-2226
Telephone numbers: 1-800-225-6872
Fax number: 1-301-459-0394
E-mail address: ntsa@ntsa.org
Web site: http://www.ntsa.org
COPYRIGHT 2000 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group