The development of effective antiviral drugs is an important biomedical scientific achievement of the late 20th century. Highly potent drugs are now available against herpes viruses, HIV, hepatitis B virus, and influenza virus. This list will extend to papillomaviruses, respiratory viruses, enteroviruses, and hepatitis C virus over the next 5-10 years. Viruses that maintain latency (the herpes viruses) or persistence (HIV and hepatitis B virus) are not specifically cleared from the body by these drugs, but their replication can be effectively suppressed. Currently, 18 specific antiviral drugs (excluding interferons) are licensed in the United Kingdom, with many more in phase 3 clinical trials or available on expanded access. For the common viral infections, prescribing will shift into primary care, as has already occurred for shingles and herpes simplex infections.
Against this exciting background comes the news of drug resistance. Virally encoded drug resistance has been documented against nearly all compounds with antiviral activity, and the genetic basis of resistance is now known.
Biological basis of resistance
Drug resistance is defined as a reduced susceptibility to a drug in a laboratory culture system and is expressed as an altered [IC.sub.50] or [IC.sub.90] (drug concentration required to inhibit viral growth by 50% or 90% respectively). This is termed the phenotype. This phenotype is determined by specific mutations in the viral genome (the genotype), which leads to alterations in the viral target protein (for example, HIV reverse transcriptase) or the viral drug activator (for example, herpes simplex thymidine kinase). The high rate of replication of some viruses determines that many of these genetic variants will already exist in untreated infected people. This is consequent on an inherent error rate of viral polymerases, especially for RNA viruses such as HIV[1] and influenza, which replicate the viral genome. A wide range of viral variants, including those with mutations associated with drug resistance, will therefore be present. This collection of variants in one person is termed the viral quasispecies, with the "fittest" virus representing the majority population. The use of an antiviral drug will provide a selective pressure for the preferential growth of variants with a reduced susceptibility to drugs in accordance with Darwinian evolutionary principles. The emergent drug resistant virus will be the fittest in the presence of drug. Some drug resistant viruses, however, seem not to replicate as well as wild type virus (in the absence of drug)[2] In some cases, multiple mutations are required for the development of high level resistance, and insufficient suppression of viral replication by antiviral drugs will predispose to their sequential acquisition.
Laboratory tests for resistant virus comprise phenotypic or genotypic assays.[3] Phenotypic assays are generally regarded as the standard but are time consuming and depend on the ability to propagate the virus--for example, hepatitis B and C viruses cannot routinely be grown in the laboratory. Genotypic assays are easier to undertake, but they are unable to detect mutations associated with drug resistance that occur in a small proportion of the viral population. Furthermore, the relation between results obtained by genotypic and phenotypic assays may be variable. Currently, these assays are available only in specialised laboratories, and there is little consensus on how they might best be used for clinical benefit.
Clinical relevance of resistance
HIV
Resistance to drugs against HIV has developed against antiretroviral drugs of all classes--namely, the nucleoside analogue reverse transcriptase inhibitors, the nonnucleoside reverse transcriptase inhibitors, and the protease inhibitors. As more drugs against HIV have become available, treatment with combinations of three and four drugs has superseded treatment with one and two drugs, with associated clinical and virological benefits.[4] Thus, the total cost of antiretroviral drugs in the United Kingdom increased from 10m [pounds sterling] in 1996 to an estimated 60m [pounds sterling] in 1998.[5] The risk of resistance emerging is reduced by more potent suppression of viral replication (gauged by suppression of plasma HIV RNA quantity--viral load) (figure).[6] Nevertheless, in clinical practice drug failure remains common.[7]
[Figure ILLUSTRATION OMITTED]
The primary reasons why treatment fails are many and include poor drug compliance, pharmacological factors, and drug resistance, but in many cases failure occurs with resistant virus. Adherence to treatment regimens that may entail 30 or more tablets daily is less than ideal, and simplified strategies, such as once daily dosing and reducing the number of pills, are required. The drug resistant viruses present when treatment fails may have reduced susceptibilities to other drugs in the same class, or even multidrug resistance,[8] and this limits the success of second line salvage treatment. The clinical usefulness of drug resistance assays in guiding effective salvage treatments requires urgent investigation.[9]
Viruses with mutations associated with resistance in reverse transcriptase and protease genes have been isolated from patients with primary HIV infection and at first diagnosis before treatment.[10-12] This provides strong epidemiological evidence for the transmission of drug resistant viruses. In a recent case a multiply resistant virus that had been sexually transmitted was inadequately suppressed by combination treatment in the recipient.[13] The spread of resistant viruses in the community is therefore worrying. By implication, resistance testing may be required to guide effective first line treatment in communities in which drug resistant viruses have been transmitted.
Hepatitis, viruses
As trials of nucleoside and nucleotide analogues against hepatitis B virus reach an advanced stage[14] some remarkable similarities between drug resistance to HIV and hepatitis B virus have emerged.[15] Some drugs, such as lamivudine and adefovir, have activity against both viruses. Furthermore, the genetic basis of lamivudine resistance in both HIV and hepatitis B virus is similar since the viral polymerase catalytic site targeted by the drug is homologous in the two viruses. Currently, specific antiviral drugs are unlikely to eradicate hepatitis B virus from the infected person, but long term suppression of viral replication is a reasonable goal. In this respect, the development of protocols for the treatment of hepatitis B with these new classes of drugs must be guided by the current principles of HIV treatment, such as the use of combination regimes. Hepatitis B virus is compact, and the genes coding for the polymerase and surface antigen overlap. Thus, drug resistance mutations in polymerase can also alter the structure of surface antigen,[15] with implications for vaccine efficacy (hepatitis B virus vaccines generate humoral antibody responses against epitopes in the surface antigen). Careful monitoring of drug resistant variants of hepatitis B virus is therefore required as the use of these drugs increases.
Hepatitis C virus is another persistent virus, and the health costs of caring for carriers who have liver disease are likely to escalate. Promising results of interferon with or without tribavirin treatment have been reported in selected patients. However, the pharmaceutical industry is currently investing substantial resources in the development of more specific inhibitors of hepatitis C virus, targeting especially the viral protease and helicase enzymes.[16] Compounds will probably enter clinical trials within 5-10 years, and, if successful, will be widely used. The inherent variability of the hepatitis C virus genome suggests that drug resistance will readily emerge to such compounds.
Herpes viruses
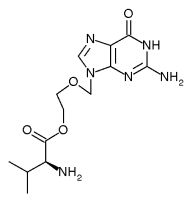
Drugs such as aciclovir, valaciclovir, and famciclovir are widely used to treat infections with herpes simplex and varicella zoster. In general, drug resistance is limited to patients who are immunocompromised; the estimated prevalence of herpes simplex resistant to aciclovir is 5-10% in patients with AIDS and recipients of bone marrow transplants.[17 18] Long term ganciclovir treatment of cytomegalovirus infections in this group of patients can also lead to resistance.[19] Second line treatments are of proved efficacy,[20 21] and drug susceptibility assays shoed be performed in immunocompromised patients with unresponsive herpes simplex infections to distinguish true antiviral resistance from other causes of clinical non-responsiveness such as poor drug absorption. Although drug resistance of herpes simplex is exceedingly rare in patients whose immune system is not compromised (estimated prevalence is 0.5% in genitourinary medicine clinics in the United States),[17] vigilance is required as the use of these drugs increases in primary care and over the counter preparations become available. Only one case of transmission of aciclovir resistant herpes has been documented to date.[22] Current understanding of the latent state of herpes simplex suggests that resistant virus shed at epithelial surfaces will revert to the wild type on subsequent reactivations, and this may limit the spread of resistant virus to others.
Influenza viruses
The unpredictability of epidemic influenza and the possibility that new, highly pathogenic influenza strains may emerge and cause severe illness in humans--for example, H5N1 in Hong Kong in 1997--make influenza a highly desirable target for antiviral drugs. Amantadine and its structural homologue rimantadine are currently the only drugs available to treat influenza A infection; on the basis of their prophylactic and therapeutic efficacy they are an acceptable alternative to vaccine. Amantadine resistant viruses occur frequently[23] and can be transmitted to others, without apparent loss of pathogenicity.[24] For this reason, care must be taken when the drug is given both for treatment of disease and as prophylaxis (as might occur in nursing ,homes during an epidemic or endemic). A new class of drug, the neuraminidase inhibitors, will soon be available,[25 26] and this may stimulate prescribing in primary care. Inappropriate use of these drugs may increase the risk of resistance developing and will be wasteful of resources if used for non-influenza symptoms.
Conclusions
The emergence of viral resistance against any specific and potent drug is virtually inevitable. Drug resistance is costly to the health service, to the patient who fails to gain maximum therapeutic benefit, and for the community in which resistant viruses may be spread. For persistent infections, resistance will develop more rapidly in the face of suboptimal virus suppression, and every attempt must be made to implement appropriate therapeutic regimens. Clear diagnostic and therapeutic guidelines are required on using antiviral agents in primary care against, for example, shingles and influenza. Finally, there is an urgent need to clarify the most effective use of antiviral resistance assays in clinical practice.
Conflict of interest: The Public Health Laboratory Service obtains funding for antiviral research from GlaxoWellcome and Roche Pharmaceuticals.
[1] Coflin JM. Population dynamics of HIV drug resistance. In: Richman DD, ed. Antiviral drug resistance. London: Wiley, 1996:267-304
[2] Back NKT, Nijhuis M, Keulen W, Boucher CAB, Essink BBO, van Kuilenburg ABP, et al. Reduced replication of 3TC-resistant HIV-1 variants in primary cells due to a processivity defect of the reverse transcriptase enzyme. EMBO J 1996;15:4040-9.
[3] Pillay D. Emergence and control of resistance to antiviral drugs in resistance in herpes viruses, hepatitis B virus, and HIV. Commun Dis Public Health 1998;1(1):5-13.
[4] Centers for Disease Control and Prevention. Report of the NIH panel to define principles of therapy of HIV infection and guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents. MMWR 1998;47:1-91.
[5] Hospital Pharmacy Audit, Medicine Audits. Monthly sales data. Sittingbourne: HPA.
[6] Havlir DV, Richman DD. Viral dynamics of HIV: implications for drug development and therapeutic strategies. Ann Intern Med 1996;124: 984-94.
[7] Ashcroft ME, Skidmore SJ, Olowokure B, Pillay D. Audit of HIV RNA quantitation measurements in the West Midlands: a preliminary report. Int J STD AIDS 1998;9:361-5.
[8] Van Vaerenbergh K, van Laethem K, Albert J, Boucher C, Clotet B, Floridia M, et al. Prevalence of multinucleoside drug resistance among European HIV-1-infected patients' receiving various combinations of nucleoside analogues. Second international workshop on HIV drug resistance and treatment strategies, Lake Maggiore, June 1998. (Abstract 69.)
[9] Hirsch MS, Conway B, D'Aquilla RT, Johnson VA, Brun-Vezinet F, Clotet B, et al. Antiretroviral drug resistance testing in adults with HIV infection. JAMA 1998;279:1984-91.
[10] Imrie A, Beveridge A, Genn W, Vizzard J, Cooper DA. Transmission of human immunodeficiency virus type 1 resistant to nevirapine and zidovudine: Sydney Primary HIV Infection Study Group. J Infect Dis 1997; 175:1502-6.
[11] Veenstra J, Schuurman R, Cornelissen M, Van't Wout AB, Boucher CAB, Schuitemaker H, et al. Transmission of zidovudine-resistant human immunodeficiency virus type 1 variants following deliberate injection of blood from a patient with AIDS: characteristics and natural history of the virus. Clin Infect Dis 1995;21:556-60.
[12] Kozal M, Leahy N, Hanrahan J, Swack N, Stapleton J. Genotypic analysis of HIV-1 pol genes from drug-naive patients presenting to clinic between 1993-1998 and drug-experienced patients failing antiretroviral combination therapy with reverse transcriptase inhibitors and protease inhibitors. Second international workshop on HIV drug resistance and treatment strategies, Lake Maggiore, June 1998. (Abstract 114.)
[13] Hecht FM, Grant RM, Petropoulos CJ, Dillon B, Chesney MA, Tian H, et al. Sexual transmission of an HIV-1 variant resistant to multiple reverse transcriptase and protease inhibitors. N Engl J Med 1998;339:307-11.
[14] Lai CL, Chien RN, Leung NWY, Chang TT, Guan R, Tai D-I, et al. A one-year trial of lamivudine for chronic hepatitis B. N Engl J Med 1998;339:61-8.
[15] Bartholmeusz A, Locarnini S. Mutations in the hepatitis B virus polymerase that are associated with resistance to famciclovir and lamivudine. Int Antiviral News 1997;5:123-4.
[16] Bartenschlager R. Molecular targets in inhibition of hepatitis C virus replication. Antiviral Chem Chemother 1997;8:281-301.
[17] Reyes M, Graber JM, Weatherall N, Hodges-Savola C, Reeves WC. Acyclovir-resistant herpes simplex virus: primary results from a national surveillance system. Eleventh international conference on antiviral research, San Diego, April, 1998. (Abstract 16.)
[18] Pottage JC, Kersler HA. Herpes simplex virus resistance to aciclovir: clinical relevance, Infect Agents Dis 1995;4:115-24.
[19] Bowen EF, Emery VC, Wilson P, Johnson M, Davey CC, Sabin CA, et al. Cyclomegalovirus polymerase chain reaction viraemia in patients receiving ganciclovir maintenance therapy for retinitis. AIDS 1998;12:605-11.
[20] Safrin S, Crumpacker C, Chatis 0P, Davis R, Hafner R, Rush J, et al. A controlled trial comparing foscarnet with vidarabine for acyclovir-resistant mucocutaneous herpes simplex in the acquired immunodeficiency syndrome. N Engl J Med 1991;325:551-5.
[21] Lalezari J, Schacker T, Feinberg J, Gathe J, Lee S, Cheung T, et al. A randomized, double-blind, placebo-controlled trial of cidofovir gel for the treatment of acydovir-unresponsive mucocutaneous herpes simplex virus infection in patients with AIDS. J Infect Dis 1997; 176:892-8.
[22] Kost RG, Hill EL, Tigges M, Straus SE. Brief report: recurrent acyclovir-resistant genital herpes in an immunocompetent patient. N Engl J Med 1993;329:1777-82.
[23] Belshe RB, Hall Smith M, Hall CB, Betts R, Hay AJ. Genetic basis of resistance to rimantadine emerging during treatment of influenza virus infection. J Virol 1988;62:1508-12.
[24] Hayden FG, Belshe RB, Clover RD, Hay AJ, Oates MG, Soo W, et al. Emergence and apparent transmission of rimantadine-resistant influenza A virus in families. N Engl J Med 1989;321:1696-702.
[25] Hayden FG, Osterhaus ADME, Treanor JJ, Fleming DM, Aoki FY, Nicholson G, et al. Efficacy and safety of the neuraminidase inhibitor zanamivir in the treatment of influenzavirus infections. N Engl J Med 1997;337:874-80.
[26] Mendel DB, Tai CY, Escare PA, Li W, Sidwell RW, Huffman JH, et al. Oral administration of a prodrug of the influenza virus neuraminidase inhibitor GS 4071 protects mice and ferrets against influenza infection. Antimicrob Agents Chemother 1998;42:640-6.
RELATED ARTICLE: Summary points
Resistance has developed to nearly all specific and effective antiviral agents
Resistance has developed to all drugs against HIV, and treating hepatitis B with nucleoside analogue monotherapy gives rise to drug resistant variants
Resistance develops rapidly when viral replication is not making maximally suppressed
Drug resistant viruses may be transmitted
Assays to measure drug resistance are available in specialised laboratories
Public Health Laboratory Service Antiviral Susceptibility Reference Unit, Division of Immunity and Infection, University of Birmingham Medical School, Birmingham B15 2TF Deenan Pillay, head of unit
Enteric and Respiratory Virus Laboratory, Central Public Health Laboratory, London NW9 5HT Maria Zambon, consultant medical virologist
Correspondence to: Dr Pillay D. Pillay@bham.ac.uk
BMJ 1998;317:660-2
COPYRIGHT 1998 British Medical Association
COPYRIGHT 2000 Gale Group