Varicella-zoster virus remains latent in the body and can cause several clinical syndromes. Antiviral agents provide a way to treat adults with herpes zoster infection, and a newly licensed live attenuated vaccine is effective in preventing chickenpox.
Cohen and several associates discussed recent advances in treating varicella-zoster virus infection. Although most cases of chickenpox occur in children and are benign, approximately 100 persons die in the United States annually from this infection. The same virus remains latent in the body throughout life and reactivates in 15 percent of persons, causing herpes zoster or shingles.
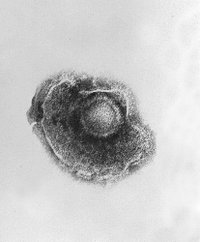
Humans are infected with varicella-zoster virus when the virus comes in contact with the mucosa of the upper respiratory tract or the conjunctiva. Contagion is thought to be greatest immediately before the onset of rash, with respiratory spread being the most important route of transmission. Dissemination through the bloodstream to the skin causes the characteristic varicella rash. The average incubation period is 14 days, with most cases occurring 10 to 20 days after exposure. The virus infects and then becomes latent in the dorsal root and the cranial nerve ganglia.
Clinical features include a generalized vesicular rash and fever, with lesions first appearing on the face and scalp, and subsequently spreading to the trunk and then to the extremities. During a period of a few days, new vesicular lesions appear as old ones develop a crust. The most common complication is secondary bacterial infection. Adults with varicella are generally more ill than children and have a greater incidence of pneumonia and death. Other complications include cerebral ataxia and encephalitis, but they are much less common (about one in 4,000 patients). Varicella in pregnant women during the first half of pregnancy is associated with fetal varicella syndrome, characterized by atrophy and scarring of the skin of the affected limb along with central nervous system damage and eye malformations. Varicella of the newborn, resulting from maternal infection occurring a few days before delivery, can increase newborn morbidity in infants five to 10 days of age. Systemic corticosteroid therapy increases morbidity, especially when administered during the incubation period. Herpes zoster occurs with viral reactivation that results in a unilateral vesicular rash usually confined to one or two adjacent dermatomes. Varicella-zoster infections are more severe in immunocompromised patients because cellular immunity is more important for defense than humoral immunity.
Laboratory confirmation of the diagnosis is unnecessary in most cases of varicella. Cultures are less sensitive in detecting the virus because of its lability. Serologic testing can be used to retrospectively confirm a diagnosis. Treatment with acyclovir shortens viral shedding and new lesion formation, and speeds healing of lesions in both healthy and immunocompromised patients. Although treatment of children may not be necessary because of the benign disease course, adolescents and adults should be treated promptly. Valacyclovir, famciclovir, foscarnet and acyclovir are newer drugs that inhibit the viral DNA polymerase. Intravenous foscarnet can be used to treat patients with advanced AIDS who have varicella that persists or recurs despite treatment with acyclovir.
Treatment of patients with zoster includes early use of an antiviral drug as well as reduction of pain. Steroids may be useful in reducing acute pain in adults older than 50 years of age who have no relative contraindications. Early treatment of postherpetic neuralgia will lessen the later perpetuation of pain. The only licensed treatment is a topical ointment containing capsaicin. Studies have shown that low dosages of tricyclic antidepressants or gabapentin added to the existing regimen are effective in reducing pain. Other treatment regimens include carbamazepine, narcotics, regional nerve blocks and acupuncture, but controlled trials have not been done to verify these impressions.
Prevention using varicella-zoster immune globulin, which must be given within 96 hours of exposure to be effective, is useful in immunocompromised persons, pregnant women and exposed infants. A one-week course of high-dose acyclovir started early can prevent chickenpox. The vaccine marketed in the United States is indicated for use in immunocompetent, nonpregnant patients older than 12 months of age without a history of varicella and is 70 to 90 percent effective in preventing chickenpox or attenuating the symptoms of chickenpox. Two doses of vaccine administered four to eight weeks apart are recommended for patients older than 12 years of age.
RICHARD SADOVSKY, M.D.
Cohen JI, et al. Recent advances in varicella-zoster virus infection. Ann Intern Med June 1, 1999;130:922-32.
COPYRIGHT 1999 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group