SUMMARY
We have developed a cheaper an simple in house indirect ELISA that uses the live attenuated VZV vaccine as a coating antigen.
The alternative ELISA had an agreement of 94% when compared with a commercial VZV ELISA kit. Moreover, our ELISA proved to be more reliable than the kit when assessing true negative samples.
By adding a standard scrum, we were able to produce results in international units per millilitre. Also, the addition of an extra step with 8M urea allowed the assessment of VZV IgG avidity without excessive costs.
The cost per sample to test VZV IgG was 2.7 times cheaper with our ELISA, allowing the testing of many samples without the burden of production of VZV antigen in the laboratory.
KEYWORDS: Varicella; ELISA; Antibody avidity.
INTRODUCTION
Assessment of varicella zoster virus (VZV) antibodies is performed routinely by enzyme immunoassays (ELISA) with commercially available kits. A cheaper and as accurate alternative is the use of "in house" ELISAs. However, that requires the production of VZV antigen in tissue culture and its subsequent extraction from VZV-infected cells. Moreover, most in house ELISAs use a control for nonspecific antibody binding, a similarly prepared extract of uninfected cells14.
Production of VZV antigen is usually performed in cell lines derived from human fibroblasts (e.g., MRC5 cell line), known to be time consuming and very often not so easy to handle21.
The increasing use of a VZV vaccine in different populations has added to the necessity of measuring anti-VZV antibodies as an indicator of prior or recurrent infection, to predict susceptibility to disease, and to evaluate immune response to vaccination3,4,5,10,12,16,17,18,22,23.
We have developed a cheaper and simple alternative indirect ELISA that uses the live attenuated VZV vaccine as a coating antigen. The use of a standard reference serum allowed us to produce results in international units per millilitre (IU/mL). Finally, with the addition of an extra step with 8M urea, we could also assess VZV IgG avidity.
MATERIAL AND METHODS
Serum samples: Two hundred and thirty-nine serum samples were tested: 221 were from healthy adults, 122 (55%) of them who referred having had varicella in the past and 99 (45%) who denied previous clinical VZV infection; the remaining 18 sera were drawn from 12-month-old infants without clinical or serologie evidence of previous VZV infection.
Serum samples were collected to investigate VZV seroprevalence in different populations. all studies were approved by the Ethics Committee of the Federal University of Sao Paulo, in Sao Paulo, Brazil.
VZV ELISA kit: A Hemagen indirect ELISA kit to detect IgG VZV antibodies (Columbia, USA) was used according to the manufacturer's instructions.
High, medium and low callibrators were added together with serum samples diluted 1 in 41, all in duplicates. A standard curve with a corresponding linear regression curve fit equation was obtained and results were calculated by interpolation of mean optical density (OD) values onto the curve fit.
Results were considered positive if they were higher than 20 arbitrary units per millilitre (AU/mL), as suggested by the kit's manufacturer.
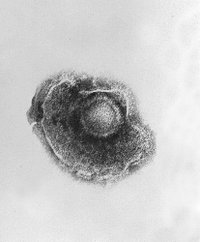
"In House" VZV indirect ELISA: Varicella IgG antibodies were assessed by an "in house" indirect ELISA. Immulon 2 96-well microtiter plates (Dyncx, USA) were coated with varicella vaccine batch VA254A41A, 10(3,3) PFU/mL (Varilrix, SmithKline Beecham, Belgium) diluted 1:100 in O. IM carbonate-bicarbonate buffer, pH 9.6, and incubated overnight at 4 °C. Two-fold serial dilutions of serum samples and of varicella reference serum [in house standard calibrated against "Varicella zoster virus antibody human immunoglobulin- NIBSC reagent (90/690)"] in 0.0IM phosphate buffered saline (PBS), pH 7.2 and 0.05% Tween 20 with 1 % bovine serum albumin (BSA) were added to the plate and incubated for I h at 37 °C. Reference serum was added to 10 wells and serum samples were added to 3 wells, in all twofold dilutions starting at 1:100.
In the next step, alkaline phosphatase conjugated rabbit anti-human IgG, specific for [gamma]-chains (Dako, Denmark) diluted 1:500 in 0.01M PBS, pH 7.2 and 0.05% Tween 20, was incubated for l h at 37 °C. p-nitrophenyl-phosphate disodium (Sigma, USA) in 0.1M diethanolaminc, 0.005M magnesium chloride buffer, pH 9.8, was used as substrate in a concentration of 1 mg/mL. OD was read at 405 nm in an immunoreader ELX-800, using 630 nm as a reference filter (Bio-Tek Instruments, USA).
Between steps, the plate was washed five times in 0.01 M PBS, pH 7.2 and 0.05% Tween 20. all solutions were added in a 100 µL volume to microplate wells. Varicella zoster antibodies were expressed in IU/ mL using the curve comparison method to transform optical density in concentration units. In all plates two blank wells we always present, and mean values were subtracted from all other wells.
IgG antibody avidity: To assess varicella IgG avidity, an extra step was added to the test. An 8M urea solution in PBS was dispensed to half of all wells after serum samples had been washed out. IgG avidity index was calculated by dividing results obtained with urea addition by results without urea and multiplying them by 100. Serum samples with avidity indices below 30% were considered with low avidity.
Protective antibody levels: Because an internationally accepted antibody level that predicts previous contact with wild varicella zoster virus or vaccine is not available, we have established a cutoff based on the following. Nineteen children who had been regularly followed up from birth and did not have evidence of previous varicella infection assessed both by clinical exam and repeated serologie testing during the first year of life were tested for varicella at 12 months of age. Cutoff of 0.2 ILVmL was calculated by adding mean antibody levels (0.04 lU/mL) to 3 standard deviations (3 × 0.04 ILVmL).
Assessment of VZV ELISA specificity: Because cross-reactivity among Herpesvirus antibodies has been described1,2, we have tested 8 serum samples for cytomegalovirus (CMV) IgG (CMV-IgG, Asxym, Immunofluorimetry with microparticles) and Epstein Barr viral capsid antigen (VCA) IgG (Indirect Immunofluorescence, "home made" with H3PR1 cells). Five sera were from adults without history of VZV infection who proved to be seronegative for IgG VZV by our "in house ELISA"; the other 3 sera were from 15 month old infants who had been vaccinated at 12 month of age with VZV vaccine (Varilrix, SmithKline Beecham, Belgium) and were seropositive for IgG by our "in house" VZV EIJSA.
RESULTS
Comparison of "in house" ELISA with commercial ELISA kit: In house ELISA and commercial ELISA kit showed an agreement of 94%. When compared with commercial kit, our in house ELISA showed a sensitivity of 95% and specifily of 87%. Only 13 out of 239 samples tested produced discordant results when assessed by both ELISAs (Table 1).
True positive and true negative samples assessed by "in house" ELISA and commercial ELISA kit: As described in the Materials and Methods session, we sellected among the samples tested by both methods those that were supposedly positive (adults who referred previous clinical VZV infection) and those that were supposedly negative (12-month infants without clinical and laboratory evidence of VZV infection).
While the commercial ELISA kit detected 98% (120 in 122) supposedly positive samples and 89% (16 in 18) supposedly negative samples, our in house ELISA detected 98% (120 in 122) and 100% (18 in 18) of the same serum samples (Table 2).
Assessment of VZV ELISA spccifity: Among the 5 samples from VZV IgG seronegative adults, 4 were positive from CMV IgG and one was negative. all 5 sera were also positive for VCA IgG antibodies.
Among the 3 samples from VZV IgG seropositive children, 2 were seronegative for CMV IgG and one was positive; 2 were seronegative for VCA IgG and one was weakly positive (Table 3).
Cost assessment of "in house" ELISA and commercial ELISA kit: Our in house ELISA proved to be cheaper than the commercial kit, with a cost per sample of US$0.99 and US$2.70, respectively (Table 4).
IgG VZV antibody avidity: By the addition of an extra 8M urea step, we were able to assess IgG VZV antibody avidity using the in house ELISA. As shown on Table 5, individuals with past primary VZV infection had high (above 60%) or intermediate IgG avidity (between 30% and 60%). Those with recent or concurrent infection showed low IgG avidity (below 30%).
DISCUSSION
We have developed a modified indirect ELISA that proved to be simple, cheap and easy to perform. Most "in house" ELISAs that detect antibodies against viruses require the production and extraction of virus antigen6,20. Many laboratories do not have tissue culture facilities, precluding the use of such techniques.
However, previous immunoassays well accepted in the literature have used alternatives for less accessible reagents. In special?, toxoid vaccines have been routinely used in ELISAs to detect tetanus and diphtheria antibodies6,9,15.
Live attenuated vaccines against measles and mumps have also been used as antigens for "in vitro" T cell proliferation assays, with good results11.
Our modified ELISA had a good agreement when compared with a commercial ELISA kit and did not show cross-reactivity with antibodies from other Herpesviruses. Moreover, it proved to be superior than the kit when true negative samples were tested. As suggested by others19, we used sera from 12 month-old infants without evidence of previous VZV infection.
Another advantage of the test we have developed was the use of a reference serum with a known concentration antibodies measured in IU/ mL. As it is well known, that allows the comparison of results obtained in different countries13.
Finally, introducing an extra step allowed the assessment of VZV IgG avidity without excessive costs.
In sum, we have developed a cheap and accurate alternative ELISA to measure VZV antibodies that proved suitable for most laboratories without the cumbersome needs of tissue culture, that produced results in lU/mL and permitted the assess of IgG avidity.
RESUMO
Desenvolvimento de ELISA indircto simples c de baixo custo para detecç o de anticorpos anti-varicela zoster
Desenvolvemos urn ensaio imunoenzimatico (ELISA) indireto simples e econ mico para deteccao de anticorpos contra o vírus da varicela zoster (VVZ) que utiliza a vacina contendo o vírus vivo atenuado como antígeno para recobrir a placa.
Este ELISA mostrou uma concord ncia de 94% quando comparado com um kit de ELISA comercial para anticorpos contra varicela. Além disso, nosso ELISA mostrou ser mais confiavel que o kit quando amostras comprovadamentc negativas foram testadas.
O uso de um soro padr o de refer nda, calibrado em unidades intcrnacionais por mililitro, possibilitou também que os resultados pudessem ser comparados com outros estudos. O acréscimo de uma etapa extra com soluç o de uréia 8M permitiu avaliaç o de avidez de IgG para VVZ scm custos excessives.
O custo por amostra para testar IgG contra VVZ com nosso ELISA foi 2,7 vezes mais barato quando comparado com o kit comercial.
REFERENCES
1. AMERICAN ACADEMY OP PEDIATRICS - Human Herpesvirus 6 (including Roseola) and 7. In: PICKERING, L.K., cd. Red Book: 2003 Report of the Committee on Infectious Diseases. 26. ed. Elk Grove Village, American Academy of Pediatrics, 2003. p. 357-358.
2. AMERICAN ACADEMY OF PEDIATRICS - Varicella-zoster infections. In: PICKERING, L.K., ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26. cd. Elk Grove Village, American Academy of Pediatrics, 2003. p. 672-686.
3. AMPOEO, K.; SAlMAN, E.; EARUSSA, P. et al. - Persistence of immunity to live attenuated varicella vaccine in healthy adults. Clin, infect. Dis., 34: 774-779, 2002.
4. ASANO, Y; SUGA, S.; YOSHIKAWA, T. el ai - Experience and reason: twenty-year follow-up of protective immunity of the Oka strain live varicella vaccine. Pediatrics, 94: 524-526, 1994.
5. BOGGER-GOREN, S.; BABA, K.; HUREEY, P. el at. - Antibody response to varicclla-zoster virus after natural or vaccine-induced infection. J. infect. Dis., 146: 260-265, 1982.
6. DE MORAES-PINTO, M.I.; ORUAMABO, R.S.; IGBAGIRI, P.P. etal. - Neonatal tetanus despite immunization and protective antitoxin antibody. J. infect. Dis., 171: 1076-1077, 1995.
7. DE MORAES-PINTO, M.I.; AEMEIDA, A.C.M.; KENJ, G. el at. - Placental transfer and maternally acquired neonatal IgG immunity in human immunodeficiency virus infection. J. infect. Dis., 173: 1077-1084; 1996.
8. GAEAZKA, A.M. - The immunological basis for immunization series. Module 2: Diphtheria. Geneva, World Health Organization, 1993.
9. GALAZKA, A.M. -The immunological basis for immunization scries. Module 3: Tetanus. Geneva, World Health Organization, 199.3.
10. GAEIL, K.; LEE, B.; STRINP, T. el at. - Outbreak of varicella at a day-care center despite vaccination. New Engl. J. Med., 347: 1909-1915, 2002.
11. GANS, H.; YASUKAWA, L.; RINKI, M. et al. - Immune responses to measles and mumps vaccination of infants at 6, 9 and 12 months. J. infect. Dis., 184: 817-826, 2001.
12. GERSHON, A.A.; STEINBERG, S.P. & GELB, L. - Live attenuated varicella vaccine use in immunocompromised children and adults. Pediatrics, 78: 757-762, 1986.
13. KEMENY, D.M. - Quantitalion. In:_______ A pratical guide to ELISA. Oxford, Pergamon, 1991. p. 57-67.
14. KRAH, D.L. - Assays for antibodies to varicella-zoster virus. Infect. Dis. Clin. N. Amer., 10: 507-527, 1996.
15. KRISTIANSEN, M.; AGGERBECK, H. & HERON, I. - Improved ELISA for determination of anti-diphtheria and/or anti-tetanus antitoxin antibodies in sera. Acta path, microbiol. immunol. scand., 105: 843-853, 1997.
16. KUTER, B.; MAITHEWS, H1; SHINEFIELD, H. el at. - Ten year follow-up of healthy children who received one or two injections of varicella vaccine. Pediat. infect. Dis. J., 23: 132-137, 2004.
17. LEVIN, MJ.; GERSHON, A.A.; WEINBERG, A. el al. - Immunization of HIV-infected children with varicella vaccine. J. Pediat., 139: 305-310, 2001.
18. REIS, A.D.; PANNUTI, C.S. & SOUZA, V.A.U.F. - Preval ncia de anticorpos para o vírus da varicela-zoster em adultos jovens de diferentes regi es climáticas brasileiras. Rev. Soc. bras. Med. trop., 36: 317-320, 2003.
19. ROBERTSON, P. W.; BELL, S.M. & PERSON, MJ. - A method for determining the cutoff value of a varicella-zoster virus IgG enzyme immunoassay for immune status. J. virol. Meth.,26: 115-118, 1989.
20. SHANLEY, J.; MYERS, M.; EDMOND, B. & STEELE, R. - Enzyme-linked immunosorbcnt assay for detection of antibody to varicella-zoster virus. J. clin. Microbiol., 15: 208-211, 1982.
21. SHEHAB1Z. & BRUNELL, P. A. -Enzyme-linked immunosorbent assay for susceptibility to varicella. J. infect. Dis., 148: 472-476, 1983.
22. WATSON, B.; KELLER, P.M.; ELLIS, R.W. & STARR, S.E. - Cell-mediated immune responses after immunization of healthy seronegative children with varicella vaccine: kinetics and specificity. J. infect. Dis., 162: 794-799, 1990.
23. ZERBONI, L.; NADER, S.; AOKI, K. & ARVIN, A.M. - Analysis of the persistence of humoral and cellular immunity in children and adults immunized with varicella vaccine. J. infect. Dis., 177: 1701-1704, 1998.
Received: 5 January 2004
Accepted: 14 May 2004
Erika ONO(1), Manuel Mindlin LAFER(1), Lily Yin WECKX(1), Cclso GRANATO(2,3) & Maria lsabel de MORAES-PINTO(1)
Research supported by FAPESP (Grants: 01/05481-0 and 97/06118-9)
(1) Division of Pediatrie Infectious Diseases, Federal University of S o Paulo.
(2) Division of Adult Infectious Diseases, Federal University of S o Paulo
(3) Immunology Department, FIeury Laboratory, S o Paulo
Correspondence to: Maria Isabel de Moraes-Pinto, Division of Pediatrie Infectious Diseases, Federal University of S o Paulo (UNIFESP-EPM). Rua Pedro de Toledo 781, 9. andar, Vila Clementine, 04039-032 S o Paulo, SP, Brasil. Tel/Fax: +55-11-5574-6471. E-mail:m.isabelmp@uol.com.br
Copyright Instituto de Medicina Tropical de Sao Paulo May/Jun 2004
Provided by ProQuest Information and Learning Company. All rights Reserved