Hot flashes are the most common and troublesome symptoms reported by women during and after perimenopause. For more than 80 percent of these women, hot f lashes persist for more than a year; 9 percent of women older than 70 years report experiencing hot f lashes. For some women, f lashes are inconvenient but not troublesome; however, about 25 percent of these women report severe symptoms that interfere with sleep and daily function. Use of the most effective therapy for hot f lashes, estrogen, has dramatically decreased since publication of the Women's Health Initiative study, which linked hormone use to increased risk of breast cancer and thromboembolic events. Many suggested alternative therapies are based on modulation of the serotonergic and noradrenergic pathways. Venlafaxine (Effexor) inhibits both pathways and has been used to treat hot flashes in women who have a history of or are at high risk of breast cancer. Evans and colleagues studied a long-acting form of venlafaxine in a general population of women experiencing hot f lashes.
The 80 participants were recruited through media advertising and information distributed by clinics. All participants were postmenopausal and reported that they experienced more than 14 hot flashes per week. Women were excluded if they were taking reproductive hormones or antidepressant medications, or if they had any contraindications to antidepressant medications. All participants completed an interview and questionnaire that included mood symptoms. The women also scored the impact of hot flashes on daily activities using a rating scale. During the 12-week study, participants completed a daily diary of hot flashes (occurrence and severity) plus any perceived adverse effects of treatment. The study participants were randomly assigned to receive placebo or extended-release venlafaxine. Participants were asked to take one tablet (placebo or 37.5 mg venlafaxine) daily for one week, then two tablets daily for 11 weeks.
The two groups were comparable in all major variables, but the treatment group reported more frequent and more severe hot flashes, as well as more frequent alcohol use. Eleven women in the treatment group withdrew from the study because of problems with sleeping, anxiety, nausea, or decreased libido. Eight women withdrew from the placebo group because of lack of impact on symptoms. By the end of the first month of the study, patient scores of the effect of hot flashes on daily activities had declined substantially in both groups. In the venlafaxine group, these scores continued to decline until week 12; the scores of the women in the placebo group reverted to baseline. The mean treatment group score fell from 72.4 to 35.3, whereas that of the placebo group returned to around 62. The reduction of 51 percent in the venlafaxine group was significantly greater than the 15 percent recorded in the placebo group. Data from patient diaries showed a reduction in hot flash severity in both groups with a greater, but not significant, improvement in the treatment group. Dry mouth, decreased appetite, and sleeplessness were more common in the venlafaxine group; however, dizziness, tremors, anxiety, diarrhea, and rash were more common in the placebo group. Almost all (93 percent) of the patients treated with venlafaxine chose to continue this medication after the study had ended.
The authors conclude that in this study extended-release venlafaxine significantly modulated the impact of hot flashes on daily activities, but it did not dramatically reduce the apparent frequency or severity of hot flash episodes. They suggest that these results indicate mood elevation or increased coping ability in women with menopause.
ANNE D. WALLING, M.D.
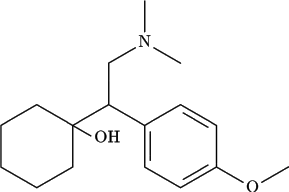
Evans ML, et al. Management of postmenopausal hot flushes with venlafaxine hydrochloride: a randomized, controlled trial. Obstet Gynecol January 2005;105:161-6.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group