Ventricular septal defect (VSD) is considered one of the most common congenital heart diseases in patients with Down's syndrome. it is well known that some VSDs show a tendency to diminish in size and to close. To our knowledge, in patients with Down's syndrome spontaneous closure of a perimembranous inlet VSD has not been decribed before. The pervalence of some cardiac malformations and the rarity of others have been reported in patients with Down's syndrome. Left ventricular outflow tract obstruction rarely occurs in patients with Down's syndrome. A case of Down's syndrome with coarctation of the aorta, patent ductus arteriousus, and perimembranous inlet VSD that spontaneously closed by formation of aneurysm of the membranous septum is reported.
Ventricular septal defect (VSD) is considered one of the most frequent congenital heart diseases in Down's syndrome.[1-3] The prevalence of perimembranous subaortic defect followed in rate by perimembranous inlet defect and the rarity of muscular VSD already have been reported.[3] Left ventricular outflow tract obstruction and mitral stenosis are very rare in patients with VSD and Down's syndrome.[3-4]
Usually, perimenbranous septal defects show a tendency to diminish in size and to close,[5,6] but spontaneous closure is very unusual in patients with Down's syndrome.[6]
We report a patient with Down's syndrome with coarctation of the aorta, patent ductus arteriosus, and perimembranous inlet VSD spontaneously closed by aneurysm of the membranous septum after coarctation repair. The association of coarctation of the aorta and the spontaneous closure of perimembranous inlet VSD in a patient with Down's syndrome make this case unusual.
CASE REPORT
An infant, delivered at 33 weeks of gestation, weighed 1.9 kg and was 44 cm long. The baby was referred to us because of a heart murmur and Down's syndrome. He was admitted to our hospital at 1 month of age, weighing 2.2 kg and in congestive heart failure.
Physical examination showed a very sick patient with Down's syndrome phenotype, failure to thrive, absent femoral and pedal pulses, and moderate hepatomegaly. A grade 3/6 systolic heart murmur was evident in the fourth intercostal space on the left sternal border which irradiated to the back. Upper body blood pressure was 110/60 mm Hg versus 60/35 mm Hg in the legs, pulse rate was 170 beats per minute and respiratory rate was 37 breaths per minute.
The chest x-ray film showed cardiac enlargement and pulmonary venous congestion. The electrocardiogram showed normal sinus rhythm, a P-R interval of 0.14 s, a QRS width of 0.08 s, a QRS complex mean frontal axis of + 120[degrees], and a tall R wave in [V.sub.4]R, [V.sub.1], [V.sub.2].
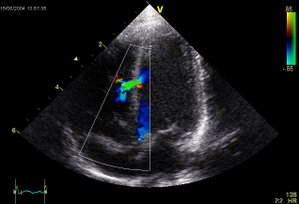
At two-dimensional echocardiography, the diagnosis of a large inlet VSD (Fig 1), aortic coactation, and a small patient ductus arterious was made. Using continuous wave Doppler across aortic coarctation, we measured a peak pressure gradient of 50 mm Hg. The diagnosis of Down's syndrome was confirmed by karyotipe analysis.
Four days after admission, the patient underwent coarctation repair with patch angioplasty and ductus arteriousus ligation. The postoperative period was uncomplicated, and he was discharged ten days after surgery without medication.
During the following period he had regular growth and no sings of heart failure. The two-dimensional ecnocardiogram confirmed the diagnosis of inlet VSD and showed a large aneurysm of the interventricular septum. No significant pressure gradient on the aortic isthmus was evidenced by continuous wave Doppler.
Magnetic resonance imaging, cardiac catheterization, and angiography, performed when the patient was eight months of age, demonstrated complete spontaneous closure of the VSD with a large aneurysm of the interventricular septum (Fig 2) and the good results of the coarctation repair, with a 10 mm Hg pressure gradient across the aortic isthmus.
DISCUSSION
In patients with Down's syndrome, the prevalence is well known of some cardiac malformations like atrioventricular septal defect, VSD, tetralogy of Fallot, patient ductus arteriosus, and the rarity of other forms like truncus arteriosus, transposition of the great arteries, hypoplastic left heart syndrome, and anomalies of the atrial situs or ventricular looping.[1-2] Further more, the prevalence of the complete form of atrioventricular septal defect vs the partial form in Down's syndrome has been described.[1,2] Recent reports have described in patients with Down's syndrome the prevalence of inlet VSD with a cleft of the mitral valve, the rarity of muscular VSD, left outflow tract obstruction, and mitral valve stenosis as opposed to findings in patients without Down's syndrome.[1-4]
Our ptient presented with a perimembranous inlet VSD, typical for Down's syndrome, and aortic coarctation; this is considered a rare association. The mitral valve was normal.
It is accepted that perimembranous defects show a spontaneous tndency to diminish in size and to close.[5,6] An aneurysm of the membranous septum has been considered as the mechanism for this closure by some authors.[6] On the other hand, other authors have considered reduplication of tricuspid valve tissue, adhesion of tricuspid valve leaflets, and prolapse of an aortic valve leaflet,[5] as the most frequent mechanism respondible for this.
Spontaneous closure of perimembranous defects is unusual in patients with Down's syndrome.[6]
Our patient and in neonatal age a perimembranous inlet VSD without any evidence of aneurysm of the membranous septum.
At three months of age, a large aneurysm of the membranous septum was observed on the two-dimensional echocardiography and confirmed at cardiac catheterization and magnetic resonaance imaging that showed, at eight months of age, the evidence of complete closure of perimembranous
To our knowledge, spontaneous closure of perimembranous inlet VSD has not been described before in a patient with Down's syndrome and associated aortic coarctation.
REFERENCE
[1] Laursen HB. Congenital heart disease in Down's syndrome. Br Heart J 1976; 38:32-38
[2] Park SG, Mathews RA, Zuberbuhler JR, Rowe RD, Nekes WH, Lenox CC. Down syndrome with congenital heart malformation. Am J Dis Child 1977; 131:29-33
[3] Marino B, Papa M, Guccione P, Corno A, Marasini M, Calabro R. Ventricular septal defect in Down syndrome. Am J Dis Child 1990; 144:544-45
[4] De Biase L, Di Ciommo V, Ballerini L, Bevilacqua M, Marcelletti C, Marino B. Prevalence of left-sided obstructive lesions in patients with atrioventricular canal without Down's syndrome. J Thorac Cardiovasc Surg 1986; 91:467-69
[5] Anderson RH, Lenox CC, Zuberbuhler JR. Mechanism of closure of perimembranous ventricular septal defect. Am J Cardiol 1983; 52:341-45
[6] Ramaciotti C, Keren A, Silverman NH. Importance of (perimembranous) ventricular septal aneurysm in the natural history of isolated perimembranous ventricular septal defect. Am J Cardiol 1986; 57:268-72
COPYRIGHT 1993 American College of Chest Physicians
COPYRIGHT 2004 Gale Group