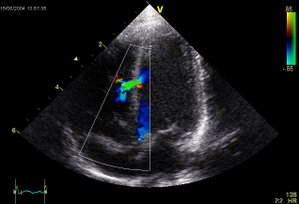
Ventricular septal defect
A ventricular septal defect (or VSD) is a defect in the ventricular septum (the wall dividing the left and right ventricles of the heart). more...
The ventricular septum consists of a muscular (inferior) and membranous portion (superior). The membranous portion (which is close to the atrioventricular node) is most commonly affected.
Congential VSDs are collectively the most common congenital heart defect.
Diagnosis
VSDs can be detected by cardiac auscultation, as they typically cause systolic murmurs. Confirmation of findings from cardiac auscultation can be obtained with a cardiac ultrasound (echocardiography) (less invasive) and cardiac catheterization (more invasive).
Auscultation is generally considered sufficient for ruling-out a significant VSD, if done by a pediatric cardiologist. This holds true as long as the pressures on the right side of the heart is low.
Pathophysiology
Large VSDs result in a significant left-to-right shunt and increase load on the right ventricle. If untreated, they result in hypertrophy of the right ventricle, which ultimately leads to right heart failure and death.
Treatment
Treatment is either surgical (open or percutaneous endovascular) or conservative. Smaller congenital VSDs often close on their own (as the heart grows) and are thus treated conservatively. Open surgical procedures require a heart-lung machine and are done with a median sternotomy. Percutaneous endovascular procedures are less invasive and can be done on a beating heart, but are only suitable for certain patients. Repair of most VSDs is complicated by the fact that the conducting system of the heart is in the immediate vicinity.
Epidemiology
VSDs are the most common congenital cardiac anomaly. It is found in 30% of all newborns with a congenital heart defect, or about 2-3 per 1000 births.
Congential VSDs are frequently associated with other congential conditions, such as Down syndrome.
A VSD can form a few days after a myocardial infarction (heart attack) due to mechanical tearing of the septal wall, before scar tissue forms, when macrophages start remodeling the dead (heart) tissue.
Read more at Wikipedia.org