ECG changes during exercise stress testing, such as false-positive ST-segment depression and disappearance of the delta wave, are reported in patients with the Wolff-Parkinson-White (WPW) pattern. We present a ease of exercise testing in a 53-year-old man with WPW syndrome with ischemic-appearing ECG changes and normal nuclear stress perfusion study findings who was thought to be at clinically low risk for having significant coronary disease. A literature review is discussed. Although ST-segment depression typical for isehemia occurs in half of the patients in whom WPW syndrome is reported, exercise testing is still an important tool in their evaluation. Data other than ECG response can be interpreted in the context of clinical history and physical examination findings to stratify the risk of coronary disease. Complete and sudden disappearance of the delta wave has been seen during exercise in 20% of patients with WPW syndrome and can identify those who are at low risk for sudden arrhythmic death.
Key words: exercise test; preexcitation syndromes; Wolff-Parkinson-White syndrome
Abbreviations: EP = electrophysiology; WPW = Wolff-Parkinson-White
**********
ECG changes during exercise testing, including ST-segment depression and loss of the delta wave, occur in patients with Wolff-Parkinson-White (WPW) syndrome. (1,2) Since Lamba first reported a case of a false-positive exercise test result in 1959, knowledge of ECG changes in the setting of WPW syndrome has been limited to several studies with small numbers of patients. The following case illustrates typical false-positive ECG changes and the disappearance of the delta wave that are elicited during treadmill testing in a patient with WPW syndrome. We review the literature to determine the frequency and clinical implications of these ECG changes, and discuss clinical situations in which exercise testing may be of value.
CASE REPORT
A 53-year-old man was sent for exercise testing prior to rotator cuff surgery. He was noted to have the WPW pattern on the ECG during his preoperative evaluation. The patient complained of occasional mild, atypical, nonpredictable chest discomfort. His medical history was unremarkable with no risk factors for coronary artery disease. On physical examination, he was normotensive with unremarkable cardiovascular examination findings. His baseline heart rate was 60 beats/Min, and his baseline BP was 118/68 mm Hg. He exercised for 12 min and 24 s, reaching 13 metabolic equivalents with a maximum heart rate of 162 beats/ min and a BP of 154/84 mm Hg. The test was stopped because of fatigue. He had no chest pain.
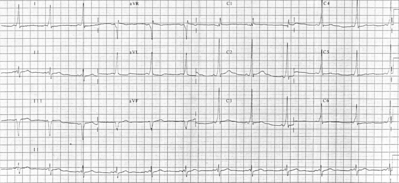
His ECG during testing demonstrated the WPW pattern at baseline, which is consistent with a posteroseptal accessory tract. ST segments were normal at rest (Fig 1, top left, a). An ST-segment depression of 1 mm began at 2 min and 50 s (Fig 1, left top middle, b), reaching a maximum of 2 mm in leads [V.SUB.4] to [V.SUB.6] at 8 Min and 50 s (Fig 1, left bottom middle, c). The delta wave suddenly and completely disappeared, and the PR interval lengthened at 9 min and 15 s (Fig 1, left bottom, d) at a heart rate of 151 beats/min with immediate normalization of ST segments extending through maximum exercise (Fig 1, right top, e). In recovery, ST segments remained normal until a heart rate of 90 beats/min occurred, at which time the delta wave reappeared with a recurrence of 1-mm ST-segment depressions (Fig 1, right top middle, f, and right bottom middle, g). At 5 min into recovery, the ECG had returned to baseline (Fig 1, right bottom, h), demonstrating resolution of the ST-segment depression with the normalization of the depolarization abnormality.
[FIGURE 1 OMITTED]
A nuclear exercise perfusion study was subsequently performed. The same ECG changes were demonstrated. Myocardial perfusion imaging was normal with no evidence of infarction or ischemia. Given his atypical symptoms, lack of risk factors, excellent exercise capacity without ischemic symptoms during exercise testing, and normal nuclear perfusion imaging findings, the patient was thought to be at low risk for having significant coronary artery disease. As concluded in several reports (1,2,4) describing otherwise low-risk patients with exercise-induced ST changes in the setting of WPW syndrome, our patient was thought to have had a false-positive exercise test result. He completed noneardiac surgery without complication.
DISCUSSION
WPW is a conduction disturbance in which atrial impulses are transmitted to the ventricle by an accessory pathway in addition to normal atrioventricular conduction. The result of these multiple fronts of depolarization is the delta wave, as well as a short PR interval and a widened QRS complex. (5) During exercise, increases in sympathetic tone and vagolysis, and subsequent changes in the automaticity of conductive tissues may result in several ECG changes. ST-segment depression typical for ischemia has been reported. (1,2) Accordingly, the current guidelines classify exercise testing in patients with WPW syndrome as a IIb indication (ie, usefulness/efficacy is less well established by evidence/opinion). (6)
ST-Segment Changes
The ischemic-appearing ST segment has been reported during exercise with depressions of up to 8 mm having been described. (2) We identified 176 patients who underwent exercise testing in eight studies (1,2,4,7-11) as having preexcitation, with ischemic-appearing changes occurring in 86 patients (49%) [Table 1]. Although the majority of these patients did not undergo angiography, most were thought to be at low clinical risk for significant coronary artery disease. Therefore, these ST changes were thought to be false-positive results. (2)
In the case of a complete block of the accessory pathway resulting in the disappearance of the delta wave, the ST segments typically normalize, representing ventricular activation and repolarization via the His-Purkinje system alone. However, the ischemic-appearing ST segments may persist despite disappearance of the delta wave. In a population thought to be experiencing false-positive exercise tests, Poyatos et al (2) demonstrated the normalization of ST segments on the ECGs of 20 of 28 patients whose delta waves had disappeared, with 8 patients continuing to display ST-segment depression on their ECGs. A proposed mechanism for this phenomenon is the concept of "cardiac memory" with persistence of abnormal repolarization, as can be seen with the cessation of pacing or the resolution of a bundle branch block. (12)
To improve diagnostic accuracy, nuclear perfusion imaging has been evaluated. However, several studies (2,7-10) have demonstrated a high frequency of perfusion abnormalities. In a review of false-positive thallium studies, Paquet et al (7) identified 47 patients in the literature with WPW syndrome who underwent stress myocardial perfusion imaging. Only 24 patients (51%) were reported as having normal study findings, with the majority of abnormal study findings being false-positive findings. The mechanism of perfusion abnormalities in patients with WPW syndrome has been compared to that seen in those with left bundle branch block. (8) Ventricular asynchrony leading to regional differences in perfusion has been described. Dipyridamole perfusion imaging (7) and exercise radionuclide ventriculography (11) have been proposed as alternative methods to better diagnose ischemia in patients with WPW syndrome.
Delta-Wave Changes
The disappearance of the delta wave has been reported in several studies, and has been used to stratify those patients who are at risk for developing rapid tachyarrhythmias and sudden death. We identified 238 patients in seven studies (2,4,10,13-16) in whom the behavior of the delta wave was described (Table 2). The complete disappearance of the delta wave is described in 98 patients (41%). Of these, 43 patients (18%) exhibited sudden complete disappearance and 44 patients (18%) exhibited gradual disappearance. Nineteen patients (8%) demonstrated incomplete disappearance.
The current consensus opinion is that the gradual disappearance of the delta wave represents facilitated and preferential conduction through the atrioventricular node over the accessory pathway as sympathetic tone increases. (4) However, the sudden disappearance of the delta wave from one beat to the next suggests a complete block of conduction in the accessory pathway, therefore identifying pathways with a long anterograde effective refractory period. (13,14)
Attempts have been made to stratify patients who are at risk of sudden death by using this classification system. Patients with short accessory pathway-refractory periods are able to sustain the fastest heart rates during atrial fibrillation, which can lead to ventricular fibrillation. (14) Patients with the shortest interval between consecutive preexcited beats (ie, the shortest RR interval) of [less than or equal to] 250 ms duration during atrial fibrillation induced in an electro-physiology (EP) study (17) had the shortest accessory pathway-refractory periods and are thought to be at the highest risk for sudden death. Sharma et al (13) studied 56 patients with both an EP study and exercise testing. Thirty-four patients who did not experience the disappearance of the delta wave had a mean ([+ or -] SD) shortest RR interval of 236 [+ or -] 64 ms. In nine patients who had a gradual loss of the delta wave, the mean shortest RR interval was 242 [+ or -] 37 ms. The sudden loss of the delta wave occurred in 13 patients and was associated with a mean shortest RR interval of 410 [+ or -] 148 ms. The authors suggested that the sudden loss of the delta wave during exercise therefore identified patients who were at low risk for the development of ventricular fibrillation.
In further support of this, Gaita et al (16) studied 65 patients without significant organic heart disease with an EP study, 8 of whom had sudden complete disappearance of the delta wave. Seven of these eight patients had a shortest RR interval of > 250 ms and were thought to be at low risk for sudden death. The authors concluded that the exercise test had a high negative predictive value in the setting of sudden, complete disappearance of the delta wave. In contrast, the gradual or incomplete loss of the delta wave during exercise did not reliably predict high-risk patients. Pappone et al (18) have proposed the routine use of EP testing to stratify the risk of young asymptomatic patients for sudden death. If such a screening strategy were employed, exercise testing prior to an EP study would potentially eliminate the need for invasive risk stratification in approximately 20% of asymptomatic patients with sudden, complete disappearance of the delta wave.
CONCLUSIONS
False-positive ST segments are common during exercise testing in WPW syndrome patients, occurring in 49% of cases, regardless of the persistence or absence of the delta wave. Nuclear exercise myocardial perfusion imaging is also associated with a high frequency of false-positive study results. However, exercise testing still is an important diagnostic tool in the evaluation of patients with WPW and should not be categorically avoided. Data such as exercise capacity, symptom reproduction, heart rate, and BP response to exercise, arrhythmia, and prognostic score indexes (19) can be interpreted in the context of the clinical history and physical examination findings to stratify the risk of coronary disease. Nuclear myocardial perfusion imaging findings, when normal, can be reassuring. Conversely, in patients who are thought to be at a higher risk for having significant atheroselerosis, a definitive evaluation with coronary angiography should be considered. Finally, the sudden and complete disappearance of the delta wave can be used to identify patients with WPW syndrome who are at low risk for sudden death, and may be a useful noninvasive adjunct to the evaluation of otherwise asymptomatic individuals with structurally normal hearts.
REFERENCES
(1) Gazes PC. False positive exercise test in the presence of the Wolff-Parkinson-White syndrome. Am J Cardiol 1969; 78: 13-15
(2) Poyatos ME, Suarez L, Lerman J, et al. Exercise testing and thallium-201 myocardial perfusion scintigraphy in the clinical evaluation of patients with Wolff Parkinson White syndrome. J Electrocardiol 1986; 19:319-326
(3) Lamb LE. Multiple variations of Wolff Parkinson White conduction in one subject: intermittent normal conduction and a false positive exercise test. Am J Cardiol 1959; 4:346
(4) Strasberg B, Ashley WW, Wyndham CRC, et al. Treadmill exercise testing in the Wolff-Parkinson-White syndrome. Am J Cardiol 1980; 45:742-747
(5) Wolff L, Parkinson J, White P. Bundle branch block with short PR interval in healthy young people prone to paroxysmal tachycardia. Am Heart J 1930; 5:685-704
(6) Gibbons J, Balady GJ, Bricker JT, et al. ACC/AHA 2002 Guideline Update for Exercise Testing: Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation 2002; 106:1883-1892
(7) Paquet N, Verreault J, Lepage S, et al. False-positive [sup.201]thallium study in Wolff-Parkinson-White syndrome. Can J Cardiol 1996; 12:499-502
(8) Archer S, Gornick C, Grund F, et al. Exercise thallium testing in ventricular preexcitation. Am J Cardiol 1987; 59:1103-1106
(9) Tawarahara K, Kurata C, Tagnchi T, et al. Exercise testing and thallium-201 emission computed tomographic in patients with intraventricular conduction disturbances. Am J Cardiol 1992; 69:97-102
(10) Pattoneri P, Astorri E, Calbiani B, et al. Thallium-201 myocardial scintigraphy inpatients with Wolff-Parkinson-White syndrome. Minerva Cardioangiol 2003; 51:87-93
(11) Greenland P, Kauffman R, Weir KE. Profound exercise-induced ST segment depression in patients with Wolff-Parkinson-White syndrome and normal coronary arteriograms. Thorax 1980; 35:559-.560
(12) Rosenbanm MB, Blanco H, Elizari MV, et al. Electrotonic modulation of the T wave and cardiac' memory. Am J Cardiol 1982; 50:213
(13) Sharma AD, Yee R, Guirandon G, et al. Sensitivity and specificity of invasive and noninvasive testing for risk of sudden death in Wolff-Parkinson-White syndrome. J Am Coll Cardiol 1987; 10:373-381
(14) Daubert C, Ollitrault J, Descaves C, et al. Failure of the exercise test to predict the anterograde refractory period of the accessory pathway in Wolff Parkinson White Syndrome. Pacing Clin Electrophysiol 1988; 11:1130-1138
(15) Levy S, Broustet JP. Exercise testing in the Wolff-Parkinson-White syndrome [letter]. Am J Cardiol 1981; 48:976
(16) Gaita F, Ginstetto C, Riccardi B, et al. Stress and pharmacologic tests as methods to identify patients with Wolff-Parkinson-White syndrome at risk of sudden death. Am J Cardiol 1989; 64:487-490
(17) Klein GJ, Bashore TM, Sellers TD, et al. Ventricular fibrillation in the Wolff-Parkinson-White syndrome. N Engl J Med 1979; 301:1980-1985
(18) Pappone C, Santinelli V, Rosanio S, et al. Usefulness of invasive electrophysiologic testing to stratify the risk of arrhythmic events in asymptomatic patients with Wolff-Parkinson-White pattern. J Am Coll Cardiol 2003; 41:239-244
(19) Froelicher V, Shelter K, Ashley E. Better decisions through science: exercise testing scores. Prog Cardiovasc Dis 2002; 44:395-414
* From the Cardiology Service, Walter Reed Army Medical Center, Washington, DC.
Manuscript received September 29, 2004; accepted September 30, 2004.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Matthew R. Jezior, MD, Captain, US Army Medical Corps, Cardiology Service, Walter Reed Arvny Medical Center, Washington, DC 20307; e-mail: matthewjezior@na.amedd. army.mil
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group