Study objectives: To evaluate the effects of spontaneous breathing at ambient airway pressure (Paw) and during airway pressure release ventilation (APRV) on respiratory work and respiratory muscle blood flow (RMBF) in experimental lung injury.
Design: Prospective experimental study.
Setting: Research laboratory of a university hospital.
Subjects: Twelve hemodynamically stable, analgosedated, and tracheotomized domestic pigs. Measurements: Respiratory work was estimated by the inspiratory pressure time product (PTPinsp) of esophageal pressure, and RMBF was measured with colored microspheres. Lung injury was induced with IV boll of oleic acid. The first set of measurements was performed before induction of lung injury while pigs were breathing spontaneously at ambient Paw, the second after induction of lung injury while breathing spontaneously at ambient Paw, and the third with lung injury and spontaneous breathing with APRV.
Results: After induction of lung injury PTPinsp increased from 138 [+ or -] 14 to 214 [+ or -] 32 cm [H.sub.2]O s/min when pigs breathed spontaneously at ambient Paw (p < 0.05) and returned to 128 [+ or -] 27 cm [H.sub.2]O s/min during APRV. While systemic hemodynamics and blood flow to the psoatic and intercostal muscles did not change, diaphragmatic blood flow increased from 0.34 [+ or -] 0.05 before to 0.54 [+ or -] 0.08 mL/g/min after induction of lung injury and spontaneous breathing at ambient Paw (p < 0.05) and returned to 0.32 [+ or -] 0.05 mL/g/min during APRV (p < 0.05 vs spontaneous breathing at ambient Paw [lung injury]).
Conclusion: Respiratory work and RMBF are increased in acute lung injury when subjects breathe spontaneously at ambient Paw. Supporting spontaneous breathing with APRV decreases respiratory work and RMBF to physiologic values.
Key words: airway pressure release ventilation; respiratory muscle blood flow; spontaneous breathing; work of breathing
Abbreviations: APRV = airway pressure release ventilation; CPAP = continuous positive airway pressure; FI[O.sub.2] = inspiratory fraction of oxygen; Paw = airway pressure; Pes = esophageal pressure; PTPinsp = inspiratory pressure time product., RMBF = respiratory muscle blood flow; Sa[O.sub.2] = arterial oxygen saturation; VE = minute ventilation; VT = tidal volume
**********
Improvement in ventilation-perfusion matching has been considered an advantage of partial ventilatory support using airway pressure release ventilation (APRV) compared to controlled mechanical ventilation (1,2) because diaphragmatic contraction by spontaneous breathing presumably augments distribution of ventilation to dependent lung regions. (3,4) Spontaneous breathing is possible throughout the ventilatory cycle during APRV, which ventilates by time-cycled switching between two levels of continuous positive airway pressure (CPAP). (5) Although spontaneous breathing with APRV has been shown to result in increased oxygen delivery in the absence of a rise in oxygen consumption, (6,7) increased oxygen demand of the respiratory muscles during partial ventilatory support has remained a concern in acute lung injury. Previous studies (8-10) in animals with either acute lung injury or hemodynamic shock have demonstrated that unassisted spontaneous breathing may result in a substantial increase in respiratory muscle blood flow (RMBF). However, these results may not be applicable to spontaneous breathing with APRV since these studies (8-10) compared controlled mechanical ventilation with spontaneous breathing at ambient airway pressure (Paw) without any ventilatory assistance. In contrast, APRV provides a constant degree of mechanical assistance, as it combines mechanical ventilation with spontaneous breathing and therefore should decrease the workload on the respiratory muscles. Because respiratory work and RMBF are closely related, (8) APRV should also decrease RMBF as compared to spontaneous breathing at ambient Paw in lung injury.
We hypothesized that the respiratory work and RMBF would be reduced during spontaneous breathing with APRV as compared to spontaneous breathing at ambient Paw in lung injury. To test this hypothesis, pigs were subjected to oleic acid-induced lung injury. Respiratory work was estimated by the inspiratory pressure time product of the esophageal pressure (PTPinsp), and RMBF was measured with the colored microspheres technique. (11)
MATERIALS AND METHODS
Instrumentation
The principles of laboratory animal care (revised National Institutes of Health guidelines, 1985) were followed, and the study was approved by the local Laboratory Animal Care and Use Committee. Twelve pigs, mixed German country breed, weighing 10 to 19 kg (15.2 [+ or -] 0.8 kg [mean [+ or -] SEM]) were fasted for 24 h while having free access to water. Prior to instrumentation, animals were premedicated with IM ketamine (10 mg/kg), xylazine hydrochloride (2 mg/kg), and glyopyrronium bromide (15 [micro]g/kg) and placed supine on a heating pad to maintain core temperature at 38[degrees]C. Anesthesia was induced with 1V sodium pentobarbital (10 mg/kg) and maintained with sodium pentobarbital (2 mg/kg/h) and ketamine (2 mg/kg/h). To ensure adequate hydration, 500 mL of Ringer solution was infused rapidly followed by an infusion rate of 5 mlJkg/h throughout the study. The animals were tracheotomized, intubated with a 7.5-mm internal diameter cuffed tracheal tube (Mallinkrodt; Argyle, NY), and breathed room air spontaneously at ambient Paw throughout instrumentation.
A 7F, three-lumen central venous catheter (OW-14703-E; Arrow International; Reading, PA) was inserted through the right jugular vein. The left carotid artery was cannulated, and a 4F pigtail catheter (Duct-Occlud 147420; PFM; Cologne, Germany) was inserted under pressure control into the left ventricle for injection of microspheres. A 7F, three-lumen catheter (OW-14703-E) was placed in the abdominal aorta via the right femoral artery for pressure monitoring and blood sampling, and a 4F, thermistor-tipped fiberoptic catheter (Pulsiocath PV2024L; Pulsion Medical Systems; Munich, Germany) was advanced through the left femoral artery into the descending thoracic aorta. A balloon catheter (International Medical; Zutphen, the Netherlands) was placed in the juxtacardlac portion of the esophagus. At the end of each experiment, the correct position of all catheters was verified by autopsy.
Ventilatory Measurements
Gas flow was measured at the proximal end of the tracheal tube with a heated pneumotachograph (No. 2; Fleisch; Lausanne, Switzerland), connected to a differential pressure transducer (SMT; Munich, Germany). Mrway pressure was measured at the proximal end of the tracheal tube with another differential gas-pressure transducer (SMT). To monitor esophageal pressure (Pes), the esophageal balloon catheter was also connected to a differential pressure transducer (SMT). The validity of the esophageal balloon measurements was tested with an occlusion method. (12) All signals were sampled with an analog/digital converter board (PCM-DAS16S/12; Computer Boards; Mansfield, MA) installed in a personal computer. Digitized signals were plotted in real-time on the computer screen and stored on magnetic media for off-line analysis.
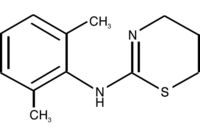
Tidal volume (VT) and minute ventilation (VE) were derived from the integrated gas flow signal. VT was indexed for body weight. Respiratory rate was determined from the gas flow signal. Mean Paw was determined for each respiratory cycle. The PTPinsp was determined from Pes as the area under the Pes/time curve, which was only considered if Pes was below a baseline value defined at end-expiration to ensure that the pressure change resulted from spontaneous breathing activity. (13) Cardiac artifacts were present on the esophageal pressure tracings, but small enough not to invalidate the calculations of the pressure/ time product (Fig 1). Spontaneous breaths during APRV may occur on the high or low CPAP levels, as well as during airway pressure release or restoration. Therefore, this Pes baseline was calculated separately for each of the four phases of the mechanical ventilatory cycle (ie, high CPAP level, low CPAP level, airway pressure release, and restoration of high CPAP level) to compensate for changes in Pes due to changes in Paw during APRV. Breaths resulting from restoration of the high CPAP alone, ie, without detectable deflection in Pes indicating lack of spontaneous breathing activity, were defined as mechanical breaths. Spontaneous breaths were defined as breaths on both CPAP levels during which no step change in Paw occurred. Assisted breaths were defined as spontaneous breaths during which also a step change in Paw occurred. In an additional analysis, ventilatory variables for these pure mechanical and spontaneous breaths were calculated separately. All ventilatory variables were averaged over a period of 10 min.
[FIGURE 1 OMITTED]
Cardiovascular Measurements
Heart rate was obtained from the ECG. Mean arterial BP and central venous pressure were transduced (Combitrans; Braun AG; Melsungen, Germany), recorded (CS/3; Datex-Engstrom; Helsinki, Finland), and stored on a personal computer at sampling intervals of 5 s (Datex AS/3 Data Collection Software; Datex-Engstrom). A horizontal plane through the midpoint of the dorsoventral thoracic diameter was taken as zero reference point for pressure measurements. The transpulmonary double-indicator dilution method was used to estimate cardiac output and intrathoracic blood volume as described previously. (14,15) Three measurements were performed at random moments during the ventilatory cycle and averaged. Standard formulas were used to calculate systemic vascular resistance and oxygen delivery. Transmural central venous pressure was derived by subtracting averaged Pes from central venous pressure. Values were indexed for body weight where appropriate.
Blood Gas Analysis
Arterial blood gases and pH were determined immediately after sampling in duplicate with standard blood gas electrodes (ABL 510; Radiometer; Copenhagen, Denmark). In each sample, hemoglobin and arterial oxygen saturation (Sa[O.sub.2]) were analyzed using spectrophotometry (OSM 3; Radiometer).
Tissue Blood Flow Measurements
Colored microspheres (Dye Trak; Triton Technology; San Diego, CA) were used to determine tissue blood flow as described previously.11 The polystyrene microspheres are coated with a single colored dye and are 15 [+ or -] 0.3 [micro]m SD in diameter. Red-, yellow-, blue-, violet-, or white-colored microspheres were used. Depending on the different absorbance characteristics of each color, 6 to 15 million microspheres suspended in 2 to 5 mL of 0.9% saline solution containing 0.02% Tween 80 were used for each blood flow measurement. Prior to injection into the left ventricle through the pigtail catheter, the suspension of microspheres was thoroughly sonicated and vortexed. The sequence of the color of microspheres was randomly assigned, and microspheres were injected slowly and continuously so that systemic hemodynamics remained unchanged during injection at all time points. After injection, the catheter was flushed with 10 mL of saline solution. Starting 10 s before the injection of microspheres and continuing for 120 s after the injection was completed, two reference blood samples were withdrawn simultaneously from different lumina of the aortic catheter at a rate of 5 mL/min with a precision pump (AH 55-2226; Harvard Apparatus GmbH; March-Hugstetten, Germany). At the end of the experiments, the animals were killed using sodium pentobarbital and potassium chloride. The crural and costal portions of the diaphragm, intercostal, and psoas major muscles and adrenal glands were removed bilaterally. The tissues were carefully dissected free of adherent fat or connective tissue. While adrenal glands were analyzed as a whole, muscle tissue samples were cut into small pieces weighing approximately 2.5 mg (BP 310 S; Sartorius; Gottingen; Germany). The trapped colored microspheres in each tissue and reference blood samples were quantified by their dye content. After digestion of the tissue and blood samples with 4 mmol/L potassium hydroxide for at least 24 h at 70[degrees]C, the microspheres were harvested on a polyester filter (pore size, 8 [micro]m; diameter, 25 mm; Nucleopore; Costar; Bodenheim, Germany). The microspheres were washed with 2% Tween 80 and then with ethanol. The dye was recovered from the microspheres by adding 200 [micro]L of dimethylformamide. Then, the dye solution was separated from the microspheres by centrifugation at 3,000g for 10 min. Spectrophotometric analysis of mixed dye solutions was performed (spectrophotometer DU64; Beckmann; Dusseldoff, Germany; wave length range, 300 to 820 nm, with 1 nm optical band width). The complex spectra were transferred to a personal computer using software (Data-Leader; Beckmann; Dusseldoff, Germany), and the composite spectrum of each dye solution was resolved into spectra of single constituents using a matrix inversion software package (Dye-Trak; Triton Technologies; San Diego, CA). From the spectrophotometric data, tissue blood flow was calculated using the following equation (11):
tissue blood flow (mL/g/min) = As x Vref/Aref/Ws
where As is the absorbance of the tissue sample, Vref is the reference blood flow (milliliters per minute), Aref is the mean absorbance of both reference blood samples, and Ws is the weight of the tissue sample. For each organ, the respective median blood flow of all samples was calculated.
Experimental Protocol
After instrumentation, pigs were allowed to stabilize for 90 min while breathing room air at ambient Paw. Measurements were performed during three periods of 30 min in duration. During the first period, the animals were left breathing spontaneously at ambient Paw (spontaneous breathing, normal lung) [Fig 1, left, A]. Then, lung injury was induced by injection of 0.1 mL/kg purified oleic acid through the central venous line over 30 min. An additional 0.2 mL were administered every 30 min until Pa[O.sub.2] was < 50 mm Hg while breathing room air at ambient Paw. The fraction of inspired oxygen (FI[O.sub.2]) was then increased to avoid acute hypoxia and was not changed thereafter. After lung injury was allowed to stabilize for another 90 min, the second set of measurements was performed (spontaneous breathing, lung injury) [Fig 1, center, B]. For the third period of measurements (APRV, lung injury), APRV was provided with a demand valve CPAP circuit of a standard ventilator (Evita; Drager; Lubeck, Germany) [Fig 1, right, C]. The low CPAP level was set at 5 cm H20, and the inspiratory to expiratory ratio was set at 1:1. Then the animals were transiently paralyzed with boli of 1 mg/kg IV succinylcholine, and the high CPAP level was adjusted to produce a VT of approximately 6 mL/kg body weight. After recovery of spontaneous breathing, the rate of mechanical ventilation was set to maintain PaC[O.sub.2] from 45 to 65 mm Hg and pH > 7.30.
Statistical Analysis
Primary variables for a power analysis were PTPinsp and regional blood flow. To detect differences between the three treatment settings with a probability of 81% ([beta] = 0.19) at a significance level of 5% ([alpha] = 0.05), based on an estimated SD of 0.67 between the treatment levels with a SD of 1.0 within the treatment levels, at least 12 animals had to be studied. To detect a difference between two levels using the Tukey honestly significant difference test with a probability of 79% ([beta] = 0.21) at a significance level of 5% ([alpha] = 0.05) with 12 animals, the contrast has to be 1.33 with a SD of 1.0 within the levels.
Results are expressed as mean [+ or -] SE. Data were evaluated for normal distribution with. Shapiro-Wilks W test. A Levene test was used to test for homogeneity of variances. To verify adequate mixing of microspheres in the blood circulation and even distribution of blood flow to the various organs after injection into the left ventricle, correlations were calculated between the number of microspheres trapped in the two reference blood samples as well as between blood flows to the right and left adrenal glands by using general linear regression. Data obtained during the different ventilatory modes were compared using the one-way analysis of variance test followed by the Tukey honestly significant difference test. Differences were considered to be statistically significant if p < 0.05.
RESULTS
For validation of the microspheres technique, adequate mixing of injected microspheres and even distribution of blood flow to the various organs were indicated by highly significant correlations between the number of microspheres trapped in the two reference blood samples (5,030 [+ or -] 619 microspheres per sample vs 4,848 [+ or -] 556 microspheres per sample, r = 0.95) and the blood flows to the right and left adrenal glands (1.99 [+ or -] 0.22 mL/g/min vs 1.91 [+ or -] 0.25 mL/g/min, r = 0.94) [p < 0.0001, respectively].
Ventilatory and lung mechanic variables are shown in Table 1, and systemic hemodynamics and gas exchange variables are shown in Table 2. Induction of lung injury resulted in a decrease in Pa[O.sub.2]/FI[O.sub.2] and Sa[O.sub.2] (p < 0.001, respectively), an increase in respiratory rate and VE (p < 0.05), and a decrease in VT when the animals breathed spontaneously at ambient Paw. Even though the PTPinsp of single spontaneous breaths was not different between the ventilatory modalities, PTPinsp per minute increased (p < 0.05) after the induction of lung injury as a result of the increase in respiratory rate at ambient Paw. With the institution of APRV, the rate of unassisted spontaneous breaths decreased (p < 0.01), effecting 55% of total VE, and PTPinsp per minute returned to baseline levels; during APRV, VE, Pa[O.sub.2]/FI[O.sub.2], and Sa[O.sub.2] returned to baseline levels. Despite the increase in VE during spontaneous breathing at ambient Paw after induction of lung injury, there was an increase in PaC[O.sub.2] and a decrease in pH (p < 0.01). Deterioration of gas exchange during spontaneous breathing at ambient Paw was associated with an increase in arterial lactate concentration (p < 0.05). While the arterial lactate concentration returned to baseline values with the institution of APRV, PaC[O.sub.2] remained significantly increased (p < 0.05) and pH (p < 0.001) was significantly reduced as compared to spontaneous breathing at normal lung conditions. There was no difference in heart rate, mean arterial pressure, transmural central venous pressure, intrathoracic blood volume, cardiac output, and systemic vascular resistance. Although the hemoglobin level was increased after induction of lung injury when animals breathed spontaneously at ambient Paw, oxygen delivery was lowest during that period.
Regional blood flow data are presented in Table 3. While regional blood flow to psoatic and intercostal muscles remained unchanged throughout the study, diaphragmatic blood flow markedly increased during spontaneous breathing at ambient Paw under the conditions of lung injury. However, when APRV was applied, diaphragmatic blood flow returned to the values observed in animals without lung injury breathing spontaneously at ambient Paw. After induction of lung injury, adrenal blood flow increased from 1.35 [+ or -] 0.16 to 2.71 [+ or -] 0.39 mL/g/min (p < 0.01) and returned to baseline values with APRV (2.02 [+ or -] 0.37 mL/g/min).
DISCUSSION
The aim of our study was to investigate the effects of spontaneous breathing on respiratory work and RMBF in a pig model with oleic acid-induced lung injury. We found that PTPinsp and diaphragmatic blood flow markedly increased when animals with lung injury were breathing spontaneously at ambient Paw, and that ventilatory support with APRV resulted in a reduction of PTPinsp and diaphragmatic blood flow to normal physiologic values not different from those obtained in animals with normal lungs breathing spontaneously at ambient Paw.
Direct measurement of RMBF is, for obvious reasons, not possible in critically ill patients. Therefore, the colored microspheres technique was used to determine RMBF in pigs. The validity of using microspheres to study regional blood flow distribution is based on adequate mixing of injected microspheres and even distribution to the various parts of the body. This was demonstrated in our study by the close correlation between the numbers of microspheres trapped in the reference blood samples from different sites in the aorta and nearly identical blood flows to the right and left adrenal glands. In our study, lung mechanics, gas exchange, and cardiovascular variables of the anesthetized pigs breathing spontaneously at ambient Paw without lung injury were similar to normal physiologic values being reported for conscious pigs.16 Therefore, instrumentation and anesthesia should have had no major effects on the validity of our results.
Partial ventilatory support is commonly used not only to separate patients from mechanical ventilation but also to provide stable ventilatory assistance of a desired degree. (6,7,17) APRV provides a constant degree of ventilator/support by time-cycled switching between two CPAP levels, allowing spontaneous breathing in any phase of the mechanical ventilator cycle. (18,19) When spontaneous breathing is abolished, APRV is not different from pressure-controlled ventilation. (18,19) Unlike pressure-support ventilation, which augments each spontaneous breath, spontaneous breathing during APRV is uncoupled from the cyclic changes of CPAP levels. (5) Therefore, during APRV, spontaneous breaths, except those occurring during the change from the lower to the upper CPAP level, are completely unassisted. (5) Acute lung injury commonly is associated with alveolar collapse resulting in a decrease in lung volume and hence lung compliance, thereby increasing the inspiratory workload of the respiratory muscles. (20) Under normal conditions, a small transpulmonary pressure change allows normal tidal breathing from the end-expiratory lung volume along the steep slope of the pressure/volume relationship. Hence, elastic work of spontaneous breathing should be minimal as indicated by the low PTPinsp observed in our animals with normal lungs. However, induction of lung injury most likely decreased lung volume and compliance. Therefore, an increased transpulmonary pressure change would have been required to generate the same VT. Thus, inspiratory work reflected by the PTPinsp increased in our pigs following induction of lung injury; as a result, VT decreased and respiratory rate increased. In agreement with previous findings,s the increase in respiratory work was associated with a marked rise in diaphragmatic blood flow. The observation that the increase in intercostal muscle blood flow was not significant confirms earlier results8 demonstrating that oleic acid-induced lung injury mainly affects blood flow to inspiratory muscles and that the diaphragm performs the majority of the inspiratory workload. Despite the higher respiratory rate effecting an increase in VE, carbon dioxide elimination decreased, indicating a lower alveolar ventilation and a failing of the respiratory muscles. In a clinical situation, acute respiratory failure would have been the indication to start ventilatory support. In accordance with previous findings, (21) the decrease in oxygen delivery was compensated for by an increase of hemoglobin levels and sympathetic stimulation, which was indicated by the increase in adrenal perfusion. However, the marked decrease in oxygen delivery and concomitant increase in arterial lactate concentration revealed that oxygen supply to the tissues was insufficient without ventilatory support after the induction of lung injury despite activation of these compensatory mechanisms. Partial ventilatory support using APRV restored arterial oxygenation, oxygen delivery, and arterial lactate concentration to values not different from those at spontaneous breathing at ambient Paw in the absence of lung injury. While systemic hemodynamics remained unchanged, adrenal and diaphragmatic blood flow and PTPinsp also returned to baseline values after the institution of APRV.
Although mechanical ventilatory support is commonly used to decrease work of breathing, an increase in lung volume and compliance may also efficiently decrease work of spontaneous breathing. (22) The application of CPAP, recruiting initially atelectatic lung areas, will increase lung volume and allow spontaneous breathing on a portion of the pressure/volume curve, where a small transpulmonary pressure change is required to produce VT. Therefore, CPAP titrated individually to increase lung compliance has been shown to reduce the work of spontaneous breathing in patients with acute lung injury. (22) In contrast, in our animals the low CPAP level was Fixed to 5 cm [H.sub.2]O, as we knew from pilot studies that spontaneous breathing in pigs is (unlike in humans) suppressed using higher Paw limits. The high CPAP level was adjusted to produce a VT of approximately 6 mL/kg. As both VT and PTPinsp of each unassisted spontaneous breath did not differ in our animals with lung injury between spontaneous breathing at ambient Paw or with APRV, it is unlikely that the decrease in PTPinsp and RMBF during APRV resulted only from alveolar recruitment. Approximately one half of VE was generated from unassisted spontaneous breaths and the other half from mechanical cycles and assisted spontaneous breaths. Therefore, the lower number of unassisted spontaneous breaths accounted for the difference in PTPinsp as compared to spontaneous breathing at ambient Paw and lung injury.
In an attempt to estimate maximal blood flow to the diaphragm being independent of respiratory workload, Johnson and Reid (23) eliminated autoregulation of the diaphragmatic vasculature by infusing adenosine and nitroprusside. Vascular conductance then can be described as a linear function of aortic BP and the maximal diaphragmatic blood flow: 0.000778 x mean arterial pressure + 0.000145 x mean arterial pressure squared. (23) Using this equation, values of maximal diaphragmatic blood flow in our animals could be estimated as 1.72 [+ or -] 0.01 mL/g/min during spontaneous breathing at ambient Paw without lung injury, 1.58 [+ or -] 0.11 mL/g/min during spontaneous breathing at ambient Paw with lung injury, and 1.46 [+ or -] 0.12 mL/g/min during spontaneous breathing with APRV and lung injury. Thus, the absolute diaphragmatic blood flow measured during spontaneous breathing at ambient Paw with normal lungs represented 21 [+ or -] 3% of maximal diaphragmatic blood flow. Induction of lung injury increased diaphragmatic blood flow to 35 [+ or -] 6% of maximal diaphragmatic blood flow during spontaneous breathing at ambient Paw and to 24 [+ or -] 4% during spontaneous breathing with APRV. These data indicate that partial ventilatory support with APRV was sufficient to counteract the marked increase in diaphragmatic blood flow observed during unassisted spontaneous breathing in our experimental animals. These findings are in agreement with previous studies8 in animals with either acute lung injury or hemodynamic shock demonstrating a marked increase in RMBF during unsupported spontaneous breathing resulting in a reduction of the perfusion of vital organs. Our observation that diaphragmatic blood flow does not significantly increase during spontaneous breathing with APRV is in agreement with previous clinical and experimental findings (24,25) indicating better renal and splanchnic perfusion with spontaneous breathing during APRV in acute lung injury.
Diaphragmatic blood flow never exceeded the maximum possible value in the present study. However, since our animals were well resuscitated and hemodynamically stable, these data may not be applicable to hemodynamically unstable subjects where respiratory blood flow demands caused by spontaneous breathing even during partial ventilatory support might exceed the maximal possible supply causing anaerobic energy production.
Controlled mechanical ventilation and resting of respiratory muscles may cause difficulties in resuming spontaneous breathing and weaning from the ventilator. (26) Even short periods of 48 h of disuse during full ventilatory support have been demonstrated to affect morphometric and contractile properties and ultrastrnctural morphology of respiratory muscles that is associated with a decreased efficiency of mitochondrial oxidative phosphorylation. (27) Therefore, partial ventilatory support using APRV allowing spontaneous breathing throughout the ventilatory cycle from the very beginning of ventilatory support might be advantageous as compared to controlled mechanical ventilation. Since respiratory work and muscle blood flow during APRV was not different from spontaneous breathing at physiologic conditions, problems arising from atrophic respiratory muscles should be less severe as compared to full ventilatory support. However, further studies including longer periods of ventilatory support are necessary to study the effects of maintaining spontaneous breathing during APRV on the metabolism of respiratory muscles and weaning from the ventilator.
In conclusion, our results add further information to previous findings that during acute lung injury respiratory work and RMBF can be essentially influenced by the choice of the ventilatory support modality. We demonstrated in hemodynamically stable animals with lung injury that maintaining spontaneous breathing during partial ventilatory support using APRV is possible without an essential increase in respiratory work and RMBF as compared to spontaneous breathing with healthy lungs at ambient Paw. Further research is warranted to elucidate whether these results are applicable to other modes of partial ventilator/support and to hemodynamically unstable subjects with lung injury.
Manuscript received December 22, 2004; revision accepted April 19, 2005.
REFERENCES
(1) Putensen C, Rasanen J, Lopez FA, et al. Effect of interfacing between spontaneous breathing and mechanical cycles on the ventilation-perfusion distribution in canine lung injury. Anesthesiology 1994; 81:921-930
(2) Putensen C, Mutz NJ, Putensen-Himmer G, et al. Spontaneous breathing during ventilatory support improves ventilation-perfusion distributions in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 1999; 159: 1241-1248
(3) Froese AB, Bryan AC. Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology 1974; 41: 242-255
(4) Wrigge H, Zinserling J, Neumann P, et al. Spontaneous breathing improves lung aeration in oleic acid-induced lung injury; Anesthesiology 2003; 99:376-384
(5) Hormann C, Baum M, Putensen C, et al. Biphasic positive airway pressure (BIPAP): a new mode of ventilatory support. Eur J Anaesthesiol 1994; 11:37-42
(6) Sydow M, Burchardi H, Ephraim E, et al. Long-term effects of two different ventilatory modes on oxygenation in acute lung injury: comparison of airway pressure release ventilation and volume-controlled inverse ratio ventilation. Am J Respir Crit Care Med 1994; 149:1550-1556
(7) Putensen C, Zech S, Wrigge H, et al. Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med 2001; 164:43-49
(8) Magder S, Erian R, Roussos C. Respiratory muscle blood flow in oleic acid-induced pulmonary edema. J Appl Physiol 1986; 60:1849-1856
(9) Hussain SN, Roussos C. Distribution of respiratory muscle and organ blood flow during endotoxic shock in dogs. J Appl Physiol 1985; 59:1802-1808
(10) Viires N, Sillye G, Aubier M, et al. Regional blood flow distribution in dog during induced hypotension and low cardiac output: spontaneous breathing versus artificial ventilation. J Clin Invest 1983; 72:935-947
(11) Kowallik P, Schulz R, Guth BD, et al. Measurement of regional myocardial blood flow with multiple colored microspheres. Circulation 1991; 83:974-982
(12) Brunner JX, Wolff G. Pulmonary function indices in critical care patients. Berlin, Germany: Springer Verlag, 1988; 118-121
(13) Chapman FW, Dziuban SW, Newell JC. Patient-ventilator partitioning of the work of breathing during weaning. Ann Biomed Eng 1989; 17:279-287
(14) Hoeft A. Transpulmonary indicator dilution: an alternative approach for hemodynamic monitoring. In: Vincent JL, ed. Yearbook of intensive care and emergency medicine. Berlin, Germany: Springer, 1995; 593-605
(15) Godje O, Peyerl M, Seebauer T, et al. Reproducibility of double indicator dilution measurements of intrathoracic blood volume compartments, extravascular lung water, and liver function. Chest 1998; 113:1070-1077
(16) Hannon JP, Bossone CA, Wade CE. Normal physiological values for conscious pigs used in biomedical research. Lab Anim Sci 1990; 40:293-298
(17) ARDS network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000; 342:1301-1308
(18) Baum M, Benzer H, Putensen C, et al. Biphasic positive airway pressure (BIPAP): a new form of augmented ventilation. Anaesthesist 1989; 38:452-458
(19) Stock MC, Downs JB, Frolicher DA. Airway pressure release ventilation. Crit Care Med 1987; 15:462-466
(20) Gattinoni L, Pesenti A, Bombino M, et al. Relationships between lung computed tomographic density, gas exchange, and PEEP in acute respiratory failure. Anesthesiology 1988; 69:824-832
(21) Ramirez J, Totapally BR, Hon E, et al. Oxygen-carrying capacity during 10 hours of hypercapnia in ventilated dogs. Crit Care Med 2000; 28:1918-1923
(22) Katz JA, Marks JD. Inspiratory work with and without continuous positive airway pressure in patients with acute respiratory failure. Anesthesiology 1985; 63:598-607
(23) Johnson RL Jr, Reid M. Limits of oxygen transport to the diaphragm. Am Rev Respir Dis 1979; 119:113-114
(24) Hering R, Peters D, Zinserling J, et al. Effects of spontaneous breathing during airway pressure release ventilation on renal perfusion and function in patients with acute lung injury. Intensive Care Med 2002; 28:1426-1433
(25) Hering R, Viehofer A, Zinserling J, et al. Effects of spontaneous breathing during airway pressure release ventilation on intestinal blood flow in experimental lung injury. Anesthesiology 2003; 99:1137-1144
(26) MacIntyre NR. Ventilatory muscles and mechanical ventilatory support. Crit Care Med 1997; 25:1106-1107
(27) Bernard N, Matecki S, Py G, et al. Effects of prolonged mechanical ventilation on respiratory muscle ultrastructure and mitochondrial respiration in rabbits. Intensive Care Med 2003; 29:111-118
Rudolf Hering, MD; Jorg Zinserling, MSc; Hermann Wrigge, MD; Dirk Varelmann, MD; Andreas Berg; Stefan Kreyer; and Christian Putensen, MD
* From the Department of Anesthesiology and Intensive Care Medicine, Rheinische-Friedrich-Wilhelms University, Bonn, Germany.
Supported by departmental funding.
Corresponctence to: Rudolf Hering, MD, Department of Anesthesiology and Intensive Care Medicine, Kreiskrankenhaus Mechernich GmbH, St.-Elisabeth-Str. 2-6, 53894 Mechernich, Germany; e-mail: Rudolf.Hering@ukb.uni-bonn.de
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group