Bell's palsy affects about one in 60 persons and has an annual incidence of around 20 per 100,000 persons. Overall, the condition is most common in persons 15 to 45 years of age, but the incidence is particularly high in pregnant women (45 per 100,000). Holland and Weiner outlined recent developments concerning the management of Bell's palsy.
Although still somewhat controversial, evidence is accumulating that reactivated herpes viruses (simplex type 1 or zoster) in cranial nerve ganglia are the most common cause of Bell's palsy. Conditions caused by the herpes zoster virus may be more severe than those caused by herpes simplex virus type 1.
Patients usually are alarmed by the sudden onset of Bell's palsy symptoms, which include facial weakness accompanied by change in taste sensation, hyperacusis, and decreased lacrimation. Some patients report ear pain or fullness before the paralysis. Severe pain is more typical of herpes zoster infections. Examination of a patient with Bell's palsy shows impaired facial and platysma muscles causing drooping of the mouth and brow plus difficulty closing the eye or mouth. The patient should be examined for evidence of other causes of lower facial weakness such as intracranial or parotid lesions or Lyme disease. Laboratory tests are not helpful in diagnosis except to exclude other potential causes of facial weakness.
Approximately 75 percent of patients recover fully from Bell's palsy, and 10 percent have minor sequelae. About one sixth of patients have residual moderate to severe weakness, contracture, spasm, or synkinesis. In patients who do not receive treatment, most improvement occurs within three weeks. Additional improvement is delayed for the four to six months required for nerve regeneration. Although prognosis cannot be predicted accurately, factors associated with poor outcome have been identified in the accompanying table.
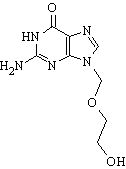
The goals of treatment are to accelerate recovery and prevent or minimize complications. Patients may require considerable reassurance and support during this illness. The eye should be protected from drying by hourly use of lubricating drops while awake and eye ointment at night. Massage, facial exercises, and biofeedback can contribute to improvement but have not been studied extensively. Steroids have been shown to increase the proportion of patients with good outcome by 17 percent if used within seven days of symptom onset. Antiviral agents, such as acyclovir (Zovirax), are increasingly recommended in combination with steroids because of the accumulating evidence of a viral etiology of Bell's palsy. Because acyclovir has low bioavailability, studies are focusing on valacyclovir (Valtrex) and famciclovir (Famvir). One prospective controlled study showed enhanced recovery when valacyclovir was combined with prednisone. The effect was particularly noticeable in older patients. Ideally, patients should begin treatment within 72 hours of symptom onset. Surgical decompression is reserved for rare cases because of danger of adverse effects.
The authors conclude that patients with Bell's palsy should begin treatment immediately and be referred to a subspecialist. Patients with significant sequelae should be referred for multidisciplinary management that could include injections of botulinum toxin, facial reanimation, and cosmetic surgery.
Holland NJ, Weiner GM. Recent developments in Bell's palsy. BMJ September 4, 2004;329:553-7.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group