As a chronic illness, both insulin-dependent diabetes mellitus (IDDM) and non-insulin-dependent diabetes mellitus (NIDDM) can develop into long-term disabling conditions by causing significant complications in major bodily systems that can result in nerve damage, foot ulcers, and circulation, vision, kidney, and heart problems (Hamburg & Inoff, 1983; Johnson, 1995). At the same time, diabetes poses more frequently occurring crises such as potentially life-threatening insulin reactions. Also called hypoglycemia or low blood sugar, insulin reactions are a "frequent and feared complication of insulin treatment" (Wredling, Theorell, Roll, Lins, & Adamson, 1992, p. 518). For people with diabetes, adaptation to disability, therefore, requires coping with immediate situational stressors such as insulin reactions, as well as with the long-term complications of the condition (Livneh & Antonak, 1997). Hence, the purpose of this study is to determine whether a relationship exists between modes of adaptation to an immediate, short-term consequence of diabetes (i.e., insulin reactions) and the long-term reality of living with diabetes.
What are insulin reactions?
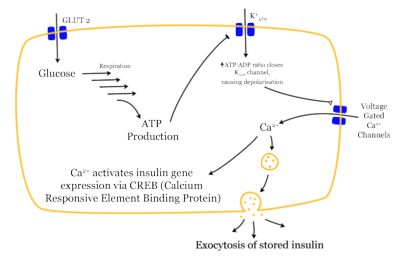
Though the brain absorbs glucose without the assistance of insulin (a hormone), all of the other cells of the body need insulin to stimulate the cellular absorption of glucose (Fogiel, 1990). An insulin reaction occurs when there is too much insulin in the bloodstream. The first symptoms of an insulin reaction can be difficulty in speaking, confusion, drowsiness, dizziness, inability to concentrate, headache, lack of coordination, and double or blurred vision, due to lowered glucose levels in the brain (neuroglycopenia) (Gold, MacLeod, Frier, & Deary, 1995). Other systemic symptoms of insulin reaction are autonomic and can include shakiness, sweating, a pounding heart, nervousness, weakness, or hunger (National Diabetes Information Clearinghouse, 1989). Insulin shock is a more severe condition of an insulin reaction that occurs when blood-sugar levels rapidly decrease and are not countered by some form of glucose. Symptoms of insulin shock can include convulsions, collapse, and possibly death, due to the lack of blood-glucose and glycogen (stored glucose) available to the brain (National Diabetes Information Clearinghouse, 1989).
Diabetes is managed by the external administration of insulin, the internal stimulation of insulin production by oral medications, or a combination of both. Diabetes management entails a minimization of constantly fluctuating blood-sugar levels. Yet, the attempt to match non-diabetic blood-sugar levels (i.e., "tight control" by multiple injections of insulin each day) is often accompanied by a higher risk for insulin reactions. Several studies indicate that recurrent insulin reactions can cause permanent cognitive impairments in individuals with insulin-dependent diabetes (Langan, Deary, Hepburn, & Frier, 1991; Wredling, Levander, Adamson, & Lins, 1990), because brain cells die when deprived of glucose. Therefore, knowledge, awareness, and action concerning insulin reactions are vital for individuals with diabetes.
Adaptation to Insulin Reactions and Diabetes
Most available diabetes research has focused on the medical aspects of diabetes or has elaborated on the overall pattern of psychological responses to diabetes (Hamburg & Inoff, 1983; Jacobson et al., 1986; Johnson, 1995). Research has not investigated the range of psychological reactions to insulin reactions, other than examining the specific fear of hypoglycemia (Cox, Irvine, Gonder-Frederick, Nowacek, & Butterfield, 1987; Green, Wysocki, & Reineck, 1990; Irvine, Cox, & Gonder-Frederick, 1994).
Two research projects studied mood states during an artificially induced hypoglycemia in a laboratory setting (Gold, MacLeod, Frier, & Deary, 1995; Merbis, Snoek, Kanc, & Heine, 1996). Both observed alterations in moods with the onset of hypoglycemia (low blood-sugar). Merbis et al. (1996) concluded that "there is an overall negative changing of mood during a gradual decline to severe hypoglycemia" (p. 120), indicating that there is a physiological basis for mood changes during hypoglycemia. Research is needed to distinguish between physiologically-induced mood changes and negative appraisals of the situation, in addition to research on psychological reactions due to hypoglycemia that was not artificially induced in a laboratory.
Powerful psychological reactions may occur during insulin reactions, as exemplified by the research reported on the use of insulin shock as a psychiatric therapy in the 20th century (e.g., as a treatment for schizophrenia). Over half a century ago, Freeman (1949, p. 183) observed that investigators, who had administered insulin-shock therapy, noted that patients viewed the experience as highly fearful and "akin to death." While the latter point is not used here as a commentary on the ethics of insulin-shock therapy, these clinical observations reflect how insulin shock, as an unresolved insulin reaction, can trigger strong psychological reactions that may include a fear of death. Emotional reactions reported during insulin shock therapy may be stronger than those experienced during insulin reactions, due to contextual, psychological, and biological factors. Yet, Gold, MacLeod, Frier, and Deary (1995) noted that individuals with diabetes often reported feeling miserable or tearful during or after an insulin reaction. In both cases of insulin reaction and insulin shock, the biological problems caused by depriving the brain of glucose can cause difficulties in cognitive-processing abilities during hypoglycemia, which can further complicate the individual's responses to insulin reaction and shock.
Irvine et al. (1994) reviewed research on the "Fear of Hypoglycemia Scale," created to examine fear of hypoglycemia or insulin reactions among individuals with diabetes. They noted that "further research is needed to verify the role of adaptive and maladaptive responses to hypoglycemia." (p. 152). In accordance with the above concerns, the present research adopted two models, a comprehensive stress/coping model (Moos & Swindle, 1990; Swindle & Moos, 1992) and a non-linear, multidimensional measure of psychosocial adaptation to chronic illness and disability (Antonak & Livneh, 1991; Livneh, 2001; Livneh & Antonak, 1990, 1991, 1997) to examine whether parallel responses occur between individuals' psychological responses to hypoglycemia, as an indicator of an acute, stressful event, and diabetes, as a long-term medical condition.
A Stress-Coping Perspective on Reactions to Diabetes and Hypoglycemia
The multiple risk-factor stress and coping model (Moos & Swindle, 1990; Swindle & Moos, 1992) is a multidimensional, bi-directional model explaining variations in life outcomes such as well-being, health, and performance in the face of stressful situations. Specifically, the model illustrates how life outcomes are a function of the way individuals appraise and cope with specific stressful events (e.g., insulin reactions), the nature of ongoing life-stressors and social resources, and the psychological characteristics of the person (e.g., internalized adaptative modes to disability, Livneh & Antonak, 1997). The stress-coping model is pertinent to this investigation because it sequentially links stressful events and the person's appraisal of and coping with those events to health outcomes. Consistent with Lazarus (1999) and others (Hobfoll, Schwarzer, Koo Chon, 1998), Moos and Swindle describe how the appraisal/coping response to a situational stressor (e.g., an insulin reaction) is influenced by personal dispositions (i.e., beliefs about self and world) or, in this case, adaptation-oriented beliefs about diabetes as a long-term disability.
Moreover, in the Moos and Swindle (1990) model, health/life outcomes (the final phase of the model) establish a baseline of health and well-being (or lack thereof) that feeds back to affect initial phases of the model, specifically the individual's personal disposition and environment. Moos and Swindle (1990) stress the reciprocal nature of their stress-coping model. This "bi-directionality" is the rationale for proposing a relationship between appraisal and coping with situational stressors and long-term adaptation to disability. In other words, a parallel relationship may exist between the appraisal of and coping with a dangerous physiological stressor related to diabetes (insulin reaction) and the person's long-term adaptation to diabetes as a potentially disabling condition. In this study, dispositional adaptation to diabetes was conceptualized in terms of a multidimensional model of psychosocial adaptation to chronic illness and disability.
The Multidimensional Adaptation Model
Livneh and Antonak have proposed (Antonak & Livneh, 1991; Livneh, 2001; Livneh & Antonak, 1990, 1991, 1997) that psychosocial adaptation to chronic illness or disability is characterized by early, intermediate, and late reactions that encompass both non-adaptive and adaptive strategies. They propose that four groups of variables influence the process of psychosocial adaptation. These factors are composed of three groups of intrapersonal variables: disability and illness-related variables, sociodemographic variables, personality variables, and one group of interpersonal variables that includes environmental and social systems variables. Livneh and Antonak (1997) and Livneh's (2001) hypothesized predictors of adaptation to chronic illness and disability, consisting of these four groups of intrapersonal and interpersonal variables, are similar to the four factors (i.e., the environmental system, personal system, event-related factors/life-crisis, and coping/appraisal) in Moos and Swindle's (1990) model that influence a fifth factor consisting of the outcomes of health and well-being.
Livneh and Antonak (1997) and Livneh's (2001) non-linear, hierarchical, multidimensional model clarifies both the types of adaptation that a person reaches with respect to chronic illness and disability and the outcomes of those states, such as differential levels of self-esteem, self-efficacy and personal mastery. Empirical research (Antonak & Livneh, 1991; Livneh & Antonak, 1990, 1991) indicates that adaptation to chronic illness and disability includes the following phase-like reactions: shock, anxiety, denial, depression, internalized anger, externalized hostility, acknowledgment, and adjustment. Their model is adopted in this research in view of the limitations of most adaptation models as unidimensional, linear, and developmental (see Livneh & Antonak, 1997, for overview). The present study seeks to investigate if similar reactions are present in long-term psychosocial adaptation, such as to diabetes, and responses to an acute, specific stressor, such as to insulin reactions.
The Research Hypotheses
The general research question for this study was: "Are time-limited appraisal and coping reactions to a particular stressful event, specifically an insulin reaction, related to extended or long-term adaptation to the condition of diabetes itself?" More specifically, the following hypotheses were formulated in order to examine the parallelism of constructs related to short-term responses to insulin reactions and long-term adaptation to diabetes:
1) RIRS' negative affectivity factor (see Instruments section) will be (a) positively associated with RIDI's second-order, psychosocial distress (i.e., non-adaptive reactions) factor, (b) independent of RIDI's Denial scale, and (c) negatively correlated with RIDI's second-order adaptive factor.
2) RIRS' resistance/avoidance factor (see Instruments section) will be (a) independent of RIDI's adaptive and psychosocial distress factors, but (b) positively correlated with RIDI's Denial scale.
3) RIRS' acceptance factor (see Instruments section) will be (a) positively linked to RIDI's adaptive factor, (b) independent of RIDI's Denial scale, and (c) negatively correlated with RIDI's psychosocial distress factor.
Method
Participants
Individuals (N=41) with either IDDM (n=16), NIDDM (n=18), or individuals who did not indicate their type of diabetes (n=7) completed a questionnaire packet at the Diabetic Health Fair in Northwest Arkansas. In this sample, 54% were females and 44% were males (and one unidentified respondent), with 68% being Caucasian, 7% American Indian, and 24% who did not indicate their ethnicity. The mean age was 52 years (SD=16.6 years). The primary marital status reported was 56% married, followed by 19% single, 12% widowed, and 5% divorced.
Secondary disabilities were reported by 24% of the participants (e.g., poor eyesight, neuropathy, heart problems, seizures, hypothyroidism, retinopathy, depression, glaucoma). The reported duration of disability was: less than one year 29%, one to four years 18%, five to nine years 18%, ten to fourteen years 15%, and fifteen or more years 21%. The employment status reported was: full-time 41%, part-time 12%, volunteer 5%, and not working 37%. Most individuals (n=28) reported needing an average of 40 minutes (M=39.68, SD=36.3) to recover their energy after experiencing an insulin reaction (three outliers were dropped from this analysis, due to their reporting of needing more than 24 hours to recover from an insulin reaction).
Instruments
Participants completed the "Reactions to Impairment and Disability Inventory" (RIDI; Livneh & Antonak, 1990), the "Responses to Insulin Reactions Scale" (RIRS; Martz, 2000), and demographic questions, including a question concerning the use of oral medication or insulin. If an individual reported using both oral medication and insulin, the individual was regarded as having IDDM, because this dual use indicates an artificial administration of insulin plus a stimulation of insulin production by oral medication.
The RIDI (Livneh & Antonak, 1990) is a 60-item, multidimensional instrument that measures adaptation to disability in terms of 8 subscales: Shock, Anxiety, Denial, Depression, Internalized Anger, Externalized Hostility, Acknowledgment, and Adjustment. Cronbach alpha coefficients have been reported to be the following for the subscales: .75, .73, .69, .78, .74, .79, .77, and .85 respectively (Livneh & Antonak, 1997).
The first author created an experimental scale to measure psychological responses to insulin reactions. Based on a 5-point Likert-type scale, eleven questions pertaining to the circumstances of insulin reactions were written to reflect non-adaptive/adaptive psychosocial responses to insulin reactions viewed from the framework of the phases of adaptation proposed by Livneh and Antonak (1997). Cronbach's coefficient alpha of the RIRS was .76 in this sample. Scores on the Responses to Insulin Reaction Scale (RIRS) were factor-analyzed to investigate their structure and ability to capture psychosocial adaptation to insulin reactions.
Using the three decision rules of eigenvalue greater than unity, Cattell's scree test, and psychological meaningfulness, three factors were retained. These three factors were than rotated both orthogonally (Varimax) as well as obliquely (Direct Oblimin and Promax) to simplify factorial meaningfulness. Factorial structures derived from the three rotations proved rather similar to one another and the Varimax- rotated structure was retained for the purposes of this study because of its ability to achieve an improved simple structure. The first factor (initial eigenvalue of 4.49; 37.4% explained variance), included 7 items and loaded on those reactions typically considered distressing or non-adaptive (e.g., anxiety, anger), suggesting generalized negative affectivity and included such items as: "Do you feel emotional when you are having an insulin reaction?" and "Do you get angry when your body is in the midst of an insulin reaction?" The second factor (eigenvalue of 1.56; 13.0% explained variance) loaded on two items, both reflecting reactions of condition acknowledgement and acceptance, namely "How long do you usually wait after knowing that your blood sugar is low before resolving it by eating or drinking something?" (not waiting at all suggesting acceptance, waiting until an insulin reaction arrives suggesting lack of acceptance or possibly denial) and "How easy is it typically for you to acknowledge to others that you are having an insulin reaction?" The third and final factor (eigenvalue of 1.25; 10.4% variance explained) loaded on 2 items and suggested a more active form of denial, possibly resistance or avoidance of the experience of insulin reactions. It included the items of "How often do you resist resolving an insulin reaction?" and "Which of the following would best describe your choices?" (ranging from 1 = I always let my blood sugars ride high to avoid insulin reactions, to 5 = I never let my blood sugars ride high to avoid insulin reactions). Factorially-derived, Varimax-rotated scores were then created for participants on all three RIRS scales (i.e., negative affectivity, acceptance, and avoidance-resistance).
Procedure
Individuals with diabetes were invited to participate and screened out of the research if they did not report verbally as having experienced an insulin reaction. As a secondary screening device, the questionnaire also included a question that asked participants to circle the physical signs that they experience during an insulin reaction. All participants, including individuals with NIDDM, circled at least one symptom of hypoglycemia, with the majority (n=31) circling two to four symptoms (e.g., light-headed, confusion, sweating, shakiness, thirstiness, or other). For completing the questionnaires, participants received a coupon for a free meal at a local restaurant and a free pen. Participants were assured that all information given would remain anonymous.
Results
Respondents tended to present a profile of positive adaptation to diabetes and insulin reactions (see Table 1). Their scores on the RIDI reflected agreement with questions typical of acknowledgment and adjustment and disagreement with questions related to shock, anxiety, denial, depression, internalized anger, and externalized hostility. In fact they reported somewhat higher scores on the adaptive scales and lower scores on the non-adaptive scales than a sample of individuals with chronic illnesses and disabilities (N = 241) studied by Antonak and Livneh (1991).
To address the main research question posited in this study and to test its first three hypotheses, correlations were first computed between the set of three RIRS-derived factors (i.e., negative affectivity, acceptance, and avoidance-resistance) and the three second-order factors of the RIDI. Prior to adopting the RIDI's three second-order factor solution, review of its eight subscales was undertaken. Examination of measures depicting the existence of outliers and skewness of distribution was first completed. Results of this examination led to the removal of three outliers and also suggested the presence of moderate skewness in most of RIDI's subscales. Two transformations were used in an effort to reduce the skewed subscale scores. A square-root transformation showed only a minimal improvement in normality, whereas a logarithmic transformation resulted in a more normalized distribution but had only a small effect on the resultant correlation matrix as compared to the non-transformed correlation matrix (entries ranged from .005 to .12, after transformation, and none of the signs changed direction). Since transformation often hinders interpretability of results (Tabachnick & Fidell, 2001) and due to space restrictions, only results obtained from the original (i.e., non-transformed) correlation matrix are reported here for both the research questions and for the following exploratory multiple regression analyses.
Since classical second-order factor analysis of the 60 RIDI items was prohibited by the small number of this study's participants, the scores on the eight RIDI scales were submitted to a set of factor analytic extraction and rotation strategies. Both orthogonal and oblique rotations yielded highly similar factorial structure. The Varimax-rotated structure was used for the purposes of this study because of its superior factorial meaningfulness. Results strongly indicated a three-factor solution and supported earlier findings by Antonak and Livneh (1991). The three factors included: (a) a psychosocial distress factor composed of five subscales that include, in order of subscale loading salience: Depression, Anxiety, Shock, Internalized Anger and Externalized Hostility (eigenvalue = 3.37, 42.1% explained variance); (b) an adaptive factor composed of the two subscales of Acknowledgment and Adjustment (eigenvalue = 1.85, 23.1% explained variance); and (c) the Denial subscale as a single factor (eigenvalue = 1.17, 14.60% explained variance). Table 2 portrays the correlations between the two sets of the three factors derived from participants' responses to the RIRS and RIDI measures.
Hypothesis 1
The first hypothesis was only partially supported. Negative affectivity (NA) as indicated by psychosocial experiences of insulin reaction was positively correlated with stressful reactions as depicted by the RIDI's psychosocial distress factor (r = .56, p =.001). NA, however, was not related to scores on the RIDI's Denial subscale (r = .10, NS). Finally, contrary to expectations, NA was independent of scores on RIDI's adaptive factor, as measured by the Acknowledgement and Adjustment subscales (r = .03; NS).
Hypothesis 2
The second hypothesis was also only partially supported. Resistance/avoidance (R/A), as measured by the RIRS, was independent of both of RIDI's adaptive and psychosocial distress factors (r = -.24, NS; r =.07, NS, respectively). It, however, failed to show association with the more extended measure of denial of diabetes, as measured by the RIDI (r = .08, NS).
Hypothesis 3
The third hypothesis received partial support. The acceptance factor as measured by the RIRS was independent of the adaptive factor generated from the RIDI data (r = .11, NS). As expected, acceptance was not associated with RIDI's Denial subscale (r = -.12; NS). Finally, acceptance of insulin reactions as predicted, was negatively linked to scores on RIDI's psychosocial distress factor (r = -.36; p = .03).
Exploratory research questions
Two exploratory multiple regression analyses were conducted. First, scores on the RIRS' negative affectivity factor were regressed on RIDI's five psychosocial distress scales (i.e., Shock, Anxiety, Depression, Internalized Anger, Externalized Hostility) to examine the latter's unique and combined contributions to psychosocial stressful reactions associated with insulin reactions. Second, scores on the RIRS acceptance factor were regressed on RIDI's two adaptive responses scales, namely, acknowledgment and adjustment to examine their respective contributions to successful psychosocial responses (i.e., scores on the acceptance factor) following insulin reactions.
The first exploratory research question sought to examine the unique and combined contributions of RIDI's five psychosocial distress (i.e., non-adaptive) subscales to the RIRS' NA factor. A stepwise multiple regression analysis was conducted in which scores on RIRS' NA factor (outcome) were regressed on RIDI's five subscales (predictors). Collinearity diagnostics were examined in view of the initially high correlation coefficients among the five RIDI's subscales (ranging from .54 to .77). Two multicollinearity statistics were examined. These included the Variance Inflation Factor (VIF) (and its converted value, Tolerance), and zero-order interscale correlations among the independent variables (Pedhazur, 1997; Tabachnick & Fidell, 1997). Neither the Tolerance values (ranging from .35 to .49), nor the magnitude of correlations (all below the recommended .90) among the five RIDI subscales, indicated problematic levels of collinearity. The model explained (adjusted R Squared) 31.2% of the variance inherent in NA. However, only scores on the Anxiety subscale entered the final model (b = .56; t (1, 30) = 3.69; p =.001).
The second exploratory research question examined the contribution of the two RIDI's adaptive subscales, namely, Acknowledgment and Adjustment, to the variance inherent in the RIRS' acceptance factor. Again, collinearity diagnostics were inspected in view of the highly significant correlation between these two predictor variables (r = .79; p < .001). As was evident from the earlier finding of hypothesis 3, the Acknowledgment and Adjustment subscales uniquely and in combination failed to contribute to variance of RIRS' acceptance factor (R = .135; [R.sup.2] = .02; F (2, 35) = .325, NS).
Discussion
The primary intent of this study was to examine the bi-directional aspects of adaptation suggested by Moos and Swindle's (1990) model. According to their model, appraisal and coping responses triggered by situational stressors (i.e., psychosocial responses to insulin reactions, in the present study) manifest an appreciable degree of parallelism to related personal disposition that the individual brings to the situation (i.e., psychosocial adaptation-associated beliefs and experiences about diabetes as a long-term chronic condition). Yet, the findings obtained in this study of 41 individuals with both insulin-dependent and non-insulin-dependent diabetes offered only partial support to the bi-directional component of the stress-coping model. Hence, although insulin reactions are stressful events for people with diabetes, these reactions do not always parallel their more long-term psychosocial adaptation to diabetes as a chronic condition.
More specifically, responses to insulin reactions that typically suggest negative affectivity, such as anxiety, depression, and anger, were indeed strongly associated with more distressing long-term psychosocial reactions to diabetes. Psychologically adaptive responses to insulin reactions, however, were independent of the more long-term psychosocial adaptive responses to diabetes. The latter finding may be reflective of the fact that although general successful adaptation to diabetes may buffer most daily (e.g., environmental, social) stressful life events, it may not exert significant control of the more physiologically-triggered insulin reactions. An additional explanation may be found in Watson's (2000) extensive research on positive and negative affect, in which he asserts that positive and negative affect are not polar opposites but "tend to fluctuate more or less independently of one another" (p. 45). Hence, in this research, negative affectivity toward insulin reactions may vary independently of positive, adaptive attitudes toward diabetes.
The second set of research hypotheses also yielded inconclusive findings. Denial of insulin reaction--as was measured by the two items depicting inattentiveness to, and resistance of resolving, insulin reactions--was independent of all three RIDI's second-order factors. Although this finding was predicted in regard to RIDI's psychosocial distress and adaptive factors, it was anticipated that a positive relationship be observed between RIRS' and RIDI's denial counterparts. Reasons underlying the failure to confirm this hypothesis may include: (a) several of the items depicting denial on the RIDI (e.g., "I believe that nothing is wrong with me") portray more "passive" forms of condition-negation, while the two RIRS items appear to reflect more "active" or "conscious" forms of denial; (b) the Denial scale of the RIDI is the least internally stable of the RIDI eight scales (see, for example, Livneh & Antonak, 1990) and, therefore, its correlations with other measures of denial are inherently constricted; and (c) the RIRS denial factor was represented by two items only, a fact that appreciably compromises its generalizability and stability.
The third set of research hypotheses, again, yielded mixed findings. As predicted, the RIRS' acceptance factor did not correlate with RIDI's denial factor. Although the RIRS' two-item, acceptance factor did correlate negatively, as predicted, with RIDI's psychosocial distress factor, it failed to be associated with its RIDI's counterpart adaptive factor. These unexpected findings may be attributed to the following: (a) the RIRS' 2-item, acceptance factor reflect a more passive type of acknowledgement of insulin-reaction, unlike the RIDI's adaptive second-order factor that includes more active adjustment-related experiences (e.g., "I can cope with almost all problems I face"); (b) in a similar vein, RIRS' acceptance factor may be perceived as tapping a non-denial, reversed-denial, or recognition of a stressful condition (e.g., length of time waited before resolving low blood sugar) rather than the more proactive stance associated with items reflective of RIDI's Adjustment scale; and (c) as in the RIRS' denial factor, the acceptance factor is also comprised of only two items, thus affecting its stability and content generalizability.
The absence of a relationship between the RIRS' acceptance factor and the RIDI's adaptive second-order factor may also be viewed from an alternative conceptual framework. Possibly the feeling of "being out of control" of one's body as a result of an insulin reaction is more often associated with non-adaptive, or at least psychologically distressing, feelings and less often related to the more adaptive states of acknowledgement and adjustment. Indeed, the majority of participants (n = 26) reported that occurrences of insulin reactions were unpredictable to them. While transient and controllable, for the most part, an insulin reaction was an acute and frightening event experienced by all individuals with diabetes regardless of their levels of adaptation.
Diabetes is an invisible disability until complications (e.g., eye or feet problems) or insulin reactions occur. Hence, individuals with diabetes may view exacerbations more as temporary negative events than as permanent disabling features that they need to accept or adapt to during the foreseeable future. Indeed, several researchers have reported that individuals with invisible disabilities respond to the status of being "disabled" differently than do people with visible disabilities (Gordon, Feldman, & Crose, 1998; Stone, 1995). This observation suggests that individuals with diabetes may respond somewhat differently to the RIDI scales than those with physical, visible disabilities.
Finally, it should be noted that most items on the RIRS are biased toward measuring negative affect (e.g., anxiety, depression). Furthermore, items tapping a proactive form of adjustment, as conceptualized by the RIDI, are missing from the RIRS. Empirical efforts to compare responses to both measures are, therefore, hindered by the lack of balance between the two scales.
Implications for Rehabilitation Professionals
The findings of this research have several implications for providing rehabilitation services to people with diabetes. First, due to the potential danger of insulin reactions, rehabilitation professionals should make certain that their clients with diabetes know the early signs of an insulin reaction (which differ slightly among individuals) and know what to do when those signs occur. Rehabilitation counselors should understand that individuals with diabetes often need to rest after an insulin reaction (Gold, MacLeod, Frier, & Deary, 1995). Gold et al. reported that a state of "tense tiredness" existed for at least 30 minutes after the resolution of an artificially-induced insulin reaction, which is similar to the finding in this study that individuals with diabetes reported needing about 40 minutes to recover from an insulin reaction. Thus, flexibility is needed, both in rehabilitation counseling activities and in the choice of work environments, when an individual has experienced an insulin reaction (e.g., a rest break, as a reasonable accommodation, if an insulin reaction should occur on the job). In addition, rehabilitation counselors must help individuals evaluate whether the occurrence of insulin reactions may create a specific situation of potential harm to self or others, in addition to examining other vocational factors that individuals with diabetes should attempt to avoid in general (Falvo, 1999).
This research has several limitations. First, the item content of the Responses to Insulin Reactions Survey (RIRS) is weighted toward asking individuals to respond to the difficulties that they experienced while having an insulin reaction. Insulin reactions are acute, stressful events for most individuals with diabetes and thereby may be associated mostly with negative affect, thus limiting the reporting of more positive reactions. A second limitation concerns threats to external validity of this study, due to the small sample of convenience that consisted of volunteers with diabetes who attended a diabetic health fair. A third limitation stems from the yet unproven psychometric qualities of the RIRS. This scale needs to demonstrate acceptable levels of reliability and validity for the findings to be interpreted with greater confidence. Finally, causality cannot be inferred from these findings, due to the correlational nature of this research. Moreover, parallelism of responses between the two measures, whenever detected, may be due to a third, covert variable (e.g., certain personality attributes not measured in the present study).
Although caution should be taken concluding that a parallel exists between situational responses to insulin reactions and psychosocial reactions to having diabetes, the results of this study do suggest a need of further research, such as on the applicability of the stress-coping model to reactions to hypoglycemia and diabetes. In addition, the relationship between adaptation to a disability and adaptation to a situational exacerbation of it needs to be examined with other episodic, invisible, chronic illnesses or disabilities, such as epilepsy, systemic lupus erythematosis, and multiple sclerosis. Similarly, researchers could examine the nature of this relationship in visible disabilities, such as amputations and spinal cord injury, which present exacerbations like skin ulcers and urinary tract infections. Empirical evidence from longitudinal studies is also needed to clarify the temporal linkage between experiencing acute, stressful events related to disability and manifesting long-term, adaptive responses to one's condition.
Acknowledgments
The authors would like to thank McDonald's Corporation for providing incentives for the participants of this research project.
References
Antonak, R. F., & Livneh, H. (1991). A hierarchy of reactions to disability. International Journal of Rehabilitation Research, 14, 13-24.
Cox, D. J., Irvine, A., Gonder-Frederick, L., Nowacek, G., & Butterfield, J. (1987). Fear of hypoglycemia: Quantification, validation, and utilization. Diabetes Care, 10 (5), 617-621.
Falvo, D. R. (1999). The medical and psychosocial aspects of chronic illness and disability (2nd ed.). Gaithersburg, MD: Aspen.
Fogiel, M. (Ed.). (1990). The biology problem-solver. Piscataway, NJ: Research and Education Association.
Freeman, T. (1949). Some observations on insulin shock therapy. British Journal of Medical Psychology, 22, 183-188.
Gold, A. E., MacLeod, K. M., Frier, B. M., & Deary, I. J. (1995). Changes in mood during acute hypoglycemia in healthy participants. Journal of Personality and Social Psychology, 68 (3), 498-504.
Gordon, P. A., Feldman, D., & Crose, R. (1998). The meaning of disability: How women with chronic illness view their experiences. Journal of Rehabilitation, 64 (3), 5-11.
Green, L. B., Wysocki, T., & Reineck, B. M. (1990). Fear of hypoglycemia in children and adolescents with diabetes. Journal of Pediatric Psychology, 15 (5), 633-641.
Hamburg, B. A., & Inoff, G. E. (1983). Coping with predictable crises of diabetes. Diabetes Care, 6 (4), 409-415.
Hobfoll, S., Schwarzer, R., & Koo Chon, K. (1998). Distinguishing the stress labyrinth: Interpreting the meaning of the term stress as it is studied in health context. Anxiety, Stress, and Coping, 11, 181-212.
Irvine, A., Cox, D., & Gonder-Frederick, L. (1994). The fear of hypoglycaemia scale. In C. Bradley (Ed.), Handbook of psychology and diabetes: A guide to psychological measurement in diabetes research and practice (pp. 133-155). Switzerland: Harwood Academic Publishers.
Jacobson, A. M., Hauser, S. T., Wertlieb, D., Wolfsdorf, J. I., Orleans, J., & Vieyra, M. (1986). Psychological adjustment of children with recently diagnosed diabetes mellitus. Diabetes Care, 9 (4), 323-329.
Johnson, S. B. (1995). Insulin-dependent diabetes in childhood. In M.C. Roberts (Ed.), Handbook of pediatric psychology (2nd ed.). New York: The Guilford Press.
Langan, S. J., Deary, I. J., Hepburn, D. A., & Frier, B. M. (1991). Cumulative cognitive impairment following recurrent severe hypoglycaemia in adult patients with insulin-treated diabetes mellitus. Diabetologia, 34, 337-344.
Lazarus, R. (1999). Stress and emotion: A new synthesis New York: Springer.
Livneh, H. (2001). Psychosocial adaptation to chronic illness and disability. Rehabilitation Counseling Bulletin, 44 (3), 151-160.
Livneh, H., & Antonak, R. F. (1990). Reactions to disability: An empirical investigation of their nature and structure. Journal of Applied Rehabilitation Counseling, 21 (4), 13-21.
Livneh, H., & Antonak, R. (1991). Temporal structure of adaptation to disability. Rehabilitation Counseling Bulletin, 34 (4), 298-318.
Livneh, H., & Antonak, R. (1997). Psychosocial adaptation to chronic illness and disability. Gaithersburg, MD: Aspen Publishers.
Martz, E. (2000). Responses to insulin reactions survey. Unpublished manuscript.
Merbis, M. A., Snoek, F. J., Kanc, K., & Heine, R. J. (1996). Hypoglycaemia induces emotional disruption. Patient Education and Counseling, 29, 117-122.
Moos, R. & Swindle, R. (1990). Stressful life circumstances: Concepts and measures. Stress Medicine, 6, 171-178.
National Diabetes Information Clearinghouse (1989). The diabetes dictionary. Washington, D.C.: U.S. Department of Health and Human Services [NIH Pub. No. 89-3016].
Pedhazur, E. J. (1997). Multiple regression in behavioral research (3rd ed.). Orlando, FL: Harcourt.
Stone, S. D. (1995). The myth of bodily perfection. Disability & Society, 10, 413-424.
Swindle, R. W., & Moos, R. H. (1992). Life domains in stressors, coping, and adjustment. In W. B. Walsh, K. H. Craik, & R. H. Price (Eds.), Person-environment psychology: models and perspectives (pp. 1-33). Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers.
Tabachnick, B., & Fidell, L. S. (2001). Using multivariate statistics (4th ed.) Boston: Allyn and Bacon.
Watson, D. (2000). Mood and temperament. New York: The Guilford Press.
Wredling, R., Levander, S., Adamson, U., & Lins, P. E. (1990). Permanent neuropsychological impairment after recurrent episodes of severe hypoglycaemia in man. Diabetologia, 33, 152-157.
Wredling, R. A., Theorell, P. G., Roll, H. M., Lins, P. E., & Adamson, U. K. (1992). Psychosocial state of patients with IDDM prone to recurrent episodes of severe hypoglycemia. Diabetes Care, 15 (4), 518-521.
Erin Martz, erinmartz@hotmail.com
COPYRIGHT 2002 National Rehabilitation Association
COPYRIGHT 2002 Gale Group