Keywords: Chinese medicine, Chinese herbal medicine, diabetic nephropathy
**********
Chinese medical journals frequently carry reports on clinical trials for the treatment of diabetic nephropathy with internally administered Chinese herbal medicinals. Some of these articles only discuss the administration of Chinese herbal medicinals, while others discuss the combined administration of Chinese medicinals and Western drugs. Most of these reports are two-wing comparison studies comparing Chinese medicine to standard Western medicine. Quantitative blood and urine analysis are the standard methods used in China for determining the efficacy of Chinese medical protocols for the treatment of diabetic nephropathy. Below are two representative clinical trials.
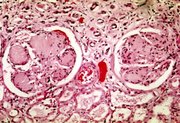
[ILLUSTRATION OMITTED]
RCT 1: Duan Yu-huai et al. published an article titled, "The Treatment of 50 Cases of Diabetic Nephropathy with Jiang Tang Yu Shen Tang (Lower Sugar & Cure the Kidneys Decoction)," in Zhe Jiang Zhong Yi Za Zhi (Zhejiang Journal of Chinese Medicine), #12, 2001, on page 511.
Cohort description: There were 98 patients in total in this study who were divided into two groups. In the treatment group, there were 29 men and 21 women aged 48-72 years, with an average age of 61.5 years. Forty-four of these cases had a disease duration of one half to two years, and the other six had been ill with nephropathy for more than two years. Twelve of these cases had simple albuminuria, 28 had accompanying lower extremity edema, seven had nephrotic syndrome, and three had azotemia. In terms of disease severity and treatment, both groups were basically the same.
Treatment method: The treatment group received the following Chinese medicinals:
Radix Polygoni Multiflori (He Shou Wu)
Radix Dioscoreae (Shan Yao)
Herba Ecliptae (Han Lian Cao)
Fructus Ligustri Lucidi (Nu Zhen Zi)
Semen Euryalis (Qian Shi), 30g each
Fructus Corni (Shan Zhu Yu), 12g
Cordyceps Sinensis (Dong Chong Xia Cao), 6g
Hirudo (Shui Zhi), 10g
Radix Rubrus Paeoniae Lactiflorae (Chi Shao), 20g
Radix Glycyrrhizae (Gan Cao), 5g
If there was simultaneous spleen-kidney yang vacuity, eight grams of Radix Lateralis Praeparatus Aconiti Carmichaeli (Zhi Fu Zi) and three grams of Cortex Cinnamomi (Rou Gui) were added.
If there was lower extremity edema, 30 grams of Rhizoma Imperatae (Bai Mao Gen) were added. One packet of these medicinals was decocted in water and administered per day in divided doses. The comparison group received 25mg of captopril TID plus 10-20mg of nifedipine TID. Both groups also received orally administered gliclazide. In addition, both groups were treated for 1-3 months. If albuminuria disappeared, one month of further treatment was given in order to consolidate the treatment effects.
Study outcomes: Cure was defined as disappearance of the symptoms and albuminuria of less than 0.1 g per day for three months or more, fasting blood glucose returning to normal, and 24 hour urine glucose less than 5g. Marked effect was defined as disappearance of symptoms, albuminuria less than 0.1g per day for three months or more, and FBG and 24 hour urine glucose reduced by 50% or more. Improvement meant that the symptoms partially disappeared, albuminuria was reduced, urine glucose was less than 3g per day, and FBG and 24 hour urine glucose was 30% or more less than before. No effect meant that none of these criteria were met.
Based on these criteria, in the treatment group, 24 cases were considered cured, 16 got a marked effect, five improved, and five got no effect, for a total amelioration rate of 90%. In the comparison group, six patients were cured, eight got a marked effect, 15 improved, and 19 got no effect, for a total amelioration rate of 60.4%. Hence there was a marked statistical difference in effects between these two groups (P + 0.01). On follow-up after one year, of 39 patients in treatment group, three cases had relapsed (7.65%). In the comparison group, eight of 14 patients had relapsed (57.1%). Therefore, the Chinese medical treatment was more effective than the Western medical protocol in terms of immediate treatment efficacy and long-term effect.
RCT 2: In issue #1, 2002 of Xin Zhong Yi (New Chinese Medicine), Gong Wei-xing and Xu Guo-an published an article titled, "A Clinical Audit of Tang Shen Tong Bao Yin (Sugar Kidney Freeing & Treasuring Drink) & Its Effects on Early Stage Diabetic Nephropathy and Improvements in Blood Rheology." This article appeared on pages 30-32 of that journal.
Cohort description: A total of 64 patients, all of whom met WHO criteria for type 2 diabetes mellitus and early stage nephropathy were included in this study. Amongst these, there were 31 males and 33 females aged 45-69 years. In all cases, 24 hour albumin elimination rate (UAE) had been more than 20Fg/min on three occasions, and 24 hour albuminuria was equal to or more than 0.5g. Nineteen patients had stage I diabetic nephropathy, 24 had stage II, and 21 had stage III. In terms of Chinese medical pattern discrimination, all met the criteria for qi and yin dual vacuity mixed with blood stasis. In addition, 26 patients had accompanying hypertension, 35 cases had accompanying retinopathy, two cases had accompanying cerebrovascular disease, and 10 cases had accompanying peripheral neuropathy. These 64 patients were divided in two groups of 32 patients each, and, in terms of sex, age, disease course, and disease severity, there were no marked statistical differences between these two groups (P > 0.05).
Treatment method: The members of the so-called treatment group received the following Chinese medicinals:
* Radix Ginseng (Ren Shen)
* Radix Et Rhizoma Rhei (Da Huang), 10g each
* Radix Puerariae (Ge Gen)
* Radix Salviae Miltiorrhizae (Dan Shen)
* Herba Leonuri (Yi Mu Cao),
* Periostracum Cicadae (Chan Tui)
* Semen Euryalis (Qian Shi), 15g each
* Radix Ligustici Wallichii (Chuan Xiong)
* Fructus Corni (Shan Zhu Yu)
* Fructus Schisandrae (Wu Wei Zi)
* Rhizoma Alismatis (Ze Xie), 12g each
Each day, 150ml of the decocted liquid made from these medicinals were administered orally BID. During the time these patients were taking these Chinese medicinals, they did not increase the doses of any Western hypoglycemic or hypotensive medications.
The 32 patients in the comparison group received 30mg of gliquidone TID and 12.5-25mg of captopril BID. Both groups were treated for four weeks.
Study outcomes: Before and after the treatment period, 24 hour urine glucose (GLU), 24 hour UAE, fasting blood glucose (FBG), creatinine, blood urea nitrogen (BUN), and a number of blood rheology indeces were measured in both groups. In the treatment group, GLU, UAE, creatinine, BUN and part of the blood rheology indeces showed marked improvement (P < 0.05). In addition, there was a marked difference in improvement between the treatment group and the comparison group in a number of the measured indices of both nephropathy and blood rheology (P < 0.05-0.01). Therefore, the conclusion was drawn that this Chinese medicinal protocol was more effective than Western medication alone in the improvement of early stage diabetic nephropathy in patients manifesting a qi and yin dual vacuity with blood stasis pattern.
For more information on the Chinese medical treatment of diabetes and its complications, see Bob Flaws, Lynn Kuchinski & Robert Casanas's The Treatment of Diabetes Mellitus with Chinese Medicine available from Blue Poppy Press. For more information on the Chinese medical treatment of nephropathy, see Wei Li et al.'s Clinical Nephropathy in Chinese Medicine also available from Blue Poppy Press.
abstracted & translated by Bob Flaws, LicAc, Dipl Ac & CH, FNAAOM
Copyright [c] Blue Poppy Press, 2005. All rights reserved.
c/o Blue Poppy Press * 5441 Western Ave. #2 * Boulder, Colorado 80301 USA
www.bluepoppy.com
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group