Facchini FS, Saylor KL. A low-iron-available, polyphenol-enriched, carbohydrate-restricted diet to slow progression of diabetic nephropathy. Diabetes 2003; 52:1204-1209.
* PRACTICE RECOMMENDATIONS
A polyphenol-enriched diet with 50% carbohydrate restriction and low iron availability was superior to a conventional protein-restricted diet in slowing the progression of diabetic nephropathy.
These findings must be confirmed by additional high-quality studies before physicians can routinely recommend a change from the conventional low-protein diet. Current use of this diet is limited, as many nutritionists--even those specializing in diabetes--have no knowledge of it.
* BACKGROUND
Patients with end-stage renal disease are usually encouraged to follow a low-protein diet to slow the progression of their renal disease. This study was conducted to determine whether a carbohydrate-restricted, low-iron/polyphenol-enriched (CR-LIPE) diet was more effective than a conventional protein-restricted diet at slowing the progression of diabetic nephropathy. Foods rich in polyphenols include olive off, green tea, cranberries, grapes, and red wine.
* POPULATION STUDIED
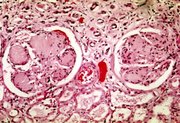
A total of 191 patients with type 2 diabetes--men and women aged 49 to 62 years who were referred to nephrology clinics in California for impending renal failure--were recruited. Subjects had a history of diabetes for 5 to 15 years, with glycosylated hemoglobin (Hb[A.sub.1C]) of 6.0% to 9.3%. Current medications for both hypertension management and glucose control were continued. When there was doubt as to the cause of renal failure, a renal biopsy was performed to confirm the diagnosis of diabetic nephropathy. The ethnicity of the subjects is not mentioned. Results are likely generalizable to a diabetic population with advanced renal disease seen in a nephrology clinic.
* STUDY DESIGN AND VALIDITY
This was a nonblinded, randomized controlled trial, although the method of randomization is not specified. Subjects were assigned with concealed allocation to either the CR-LIPE diet or the control diet, a conventional protein-restricted diet (0.8 g/kg). The main features of the CR-LIPE diet were 50% carbohydrate reduction; iron-enriched meats are replaced with iron-poor meats and foods known to inhibit iron absorption; elimination of all beverages apart from tea, water, and red wine; and the use of olive off for frying and dressings. No attempt was made to assess compliance to either diet.
Analysis was by intention-to-treat; it is unknown whether the outcome assessors were blinded to group assignment. Patients were followed for a mean of 3.9 years (range, 0.7-5.3 years); 21 (11%) were lost to follow-up (9 in the CR-LIPE group, 12 in the control group). Weaknesses included small sample size, unclear method of randomization, lack of information on compliance with the diets, and uncertainty as to whether outcomes were assessed blindly.
* OUTCOMES MEASURED
Disease-oriented outcomes included doubling of serum creatinine and end-stage renal disease as defined by serum creatinine >6.0 mg/dL. Patient-oriented outcomes included the need for renal replacement therapy or transplantation and all-cause mortality.
* RESULTS
No significant difference was seen in the baseline characteristics of the 2 groups. Serum creatinine doubled in 19 (21%) of patients on the CR-LIPE diet vs 31 (39%) control subjects (P<.01). Renal replacement therapy or death occurred in 18 (20%) of patients on the CR-LIPE diet and in 31 (39%) control subjects (P<.01; number needed to treat=5).
These findings were independent of initial serum creatinine, 24-hour protein, blood pressure, Hb[A.sub.1C], and the use of angiotensin-converting enzyme inhibitors.
Anne Mounsey, MD, Department of Family Medicine, University of Virginia, Charlottesville. E-mail: alm2d@virginia.edu.
COPYRIGHT 2003 Dowden Health Media, Inc.
COPYRIGHT 2003 Gale Group