Introduction
The importance of maintenance of tight blood pressure control in people with diabetes has come under the spotlight in the NSF Standards for Diabetes. In this second of two articles on the management of diabetic nephropathy, the role of angiotensin-converting enzyme (ACE) inhibitors and angiotensin-II receptor antagonists (AIIRAs) in the prevention and treatment of diabetic nephropathy is reviewed. This article also looks at new evidence on the impact that aggressive hypertensive management can have on nephropathy in patients with type 2 diabetes.
Diabetes is now the leading cause of renal failure in the UK, accounting for more than one in six people starting renal replacement therapy (DoH, 2003). The role of the renin-angiotensin system in the development of diabetic nephropathy has been clearly demonstrated (Zatz et al, 1986) Angiotensin-converting enzyme (ACE) inhibitors are now the recommended treatment both for normotensive and hypertensive patients with type 2 diabetes and raised albumin excretion rates (AER; DoH, 2003). The renoprotective effects of angiotensin-II receptor antagonists (AIIRAs) have also recently been confirmed and these could be valuable alternatives to ACE inhibitors.
Development of diabetic nephropathy
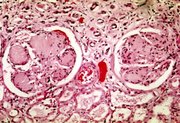
Prolonged exposure to raised blood glucose levels can damage tissues throughout the body. Initially, these changes may be reversible, but over time, raised blood glucose levels can lead to cumulative, irreversible changes. Damage to the walls of small blood vessels leads to the microvascular complications of diabetes. When this occurs in the blood vessels of the kidney, there is a progressive decline in function, which can lead, if untreated, to renal failure in a matter of years.
NSF Standards for Diabetes
The NSF Standards for Diabetes 4 and 10 recommend that all people with diabetes should receive regular surveillance for renal complications (DoH, 2003). There are standard tests that should be carried out to determine renal function (Kenny, 2002). If these tests reveal that a patient with diabetes has microalbuminuria or proteinuria, the new NSF guidelines state that they should be treated with an ACE inhibitor unless contraindicated.
It is important to note that this recommendation is made irrespective of the patient's blood pressure status, as it is now accepted that ACE inhibitors and other agents that intervene in the renin-angiotensin system have beneficial effects on renal function that are independent of their blood pressure lowering properties. It is also important to note that these recommendations apply to patients with type I and type 2 diabetes.
The first studies (Kasiske et al, 1993; Lewis et al, 1993) on the use of ACE inhibitors in patients with diabetes were carried out almost exclusively on those with type I diabetes, and early data in type 2 patients was less convincing. It is now clear that the pathologies of the two types of diabetes are the same with respect to diabetic nephropathy and the benefits of ACE inhibition can be seen in all patients with diabetes.
The role of the renin-angiotensin system
The renin-angiotensin system is a bioenzymatic cascade that results in the formation of the vasoactive peptide angiotensin II. Renin acts on the substrate angiotensinogen to produce angiotensin I, which is then converted by ACE to angiotensin II. ACE also converts bradykinin, substance P and the tachykinins to inactive fragments. However, angiotensin II is also formed in tissue via non-ACE pathways, in which, both angiotensinogen and angiotensin I are converted directly to angiotensin II by enzymes other than ACE.
Angiotensin II acts on two sets of receptors: the [AT.sub.1] receptor which is responsible for the known physiological actions of angiotensin, and the [AT.sub.2] receptor whose function is still unknown. Stimulation of the [AT.sub.1] receptor causes vasoconstriction, stimulation of the sympathetic nervous system and release of aldosterone and anti-diuretic hormone. This increases blood pressure, retention of sodium and water and adversely affects cardiovascular function and structure.
There is compelling evidence that the renin-angiotensin system is involved in the development of diabetic nephropathy, and that inhibition of the renin-angiotensin system slows the progression of diabetic nephropathy by a mechanism that is independent of any antihypertensive effects (Zatz et al, 1986). Studies in diabetic animals have shown that the glomerular efferent arteriolar tone is increased, resulting in increased transcapillary hydraulic pressure (Zatz et al, 1985; Zatz et al, 1986). This may decrease the functional integrity of the glomerular capillary wall.
Inhibition of the renin-angiotensin system and removal of the effects of angiotensin II can improve the glomerular haemodynamics in patients with diabetes. Blockade of the constricting effects of angiotensin II lowers glomerular intracapillary pressure while preserving renal plasma flow. The trophic properties of angiotensin II which promote cellular and glomerular hypertrophy are also diminished, as is the accumulation of mesangial matrix (Berk et al, 1989; Fogo et al, 1990; Remuzzi et al, 1990).
Intervention in the renin-angiotensin system
The beneficial effects of ACE inhibition arise because of the lower circulating levels of angiotensin II and consequent decreased stimulation of the [AT.sub.1] receptor. However, because ACE inhibitors are competitive inhibitors, their blockade can be overcome if the concentration of angiotensin I increases. In addition, ACE inhibitors cannot block the alternative pathways for generating angiotensin II. Accumulation of bradykinin results in increased generation of prostaglandins and nitric oxide. These substances are implicated in the sensitisation of airways and increased membrane permeability, leading to the well-known side effects of ACE inhibitors (cough and angio-oedema).
AIIRAs selectively block [AT.sub.1] receptors, offering a more complete blockade of the actions of angiotensin II without affecting the bradykinin pathway. Recently, a number of studies have reported the beneficial effects of AIIRAs in patients with type 2 diabetes and microalbuminuria or proteinuria.
Prevention of diabetic nephropathy with ACE inhibitors
A number of meta-analyses have confirmed that ACE inhibitors significantly reduce progression to proteinuria and increase the chances of regression to normoalbuminuria in patients with type I diabetes (Kasiske et al, 1993; Kshirsagar et al, 2000; ADNTG, 2001). The ADNTG study showed that 2 years of ACE inhibitor treatment reduced the AER by 50% compared with placebo.
There was a survival advantage in patients with type 2 diabetes and microalbuminuria who were treated with ramipril, as well as a reduction in the progression to overt nephropathy (HOPE study, 2000). In a study of over 400 patients with type I diabetes and proteinuria, treatment with captopril for 3 years led to a 50% reduction in a combined end-point of death, dialysis and transplantation (Lewis et al, 1993).
Prevention of diabetic nephropathy with AIIRAs
Three studies have shown that AIIRAs are effective in slowing the decline of renal function in patients with type 2 diabetes. After the publication of these studies, in June 2002, irbesartan received an extension of its licence to include the treatment of renal disease in patients with hypertension and type 2 diabetes, and at the end of 2002 the licence for losartan was similarly extended to include patients with type 2 diabetes and a history of hypertension.
Studies with irbesartan and losartan
In a study to asssess the effects of irbesartan on the development of diabetic nephropathy, nearly 600 patients with type 2 diabetes, hypertension and microalbuminuria were given either 150 or 300 mg/day of irbesartan, or placebo. The target blood pressure was 135/85 mmHg, which could be achieved with any antihypertensive drug except ACE inhibitors, AIIRAs and dihydropyridine calcium channel blockers in the control group. The study period was 2 years and the primary outcome was the time taken to reach frank proteinuria (>200 [micro]g/min). Secondary outcomes were the change in AER, normalisation of AER and the change in creatinine clearance.
Blood pressure achieved in all three groups was similar but irbesartan delayed the progression to nephropathy (AER>200 [micro]g/min) in a dose-dependent fashion: by 15% in 150mg group, by 10% in the 300mg group and by 5% in the control group. The numbers of patients who reached a normalised AER were 21%, 24% and 49% respectively, giving a 70% risk reduction with the higher dose of irbesartan (Parving et al, 2001).
The magnitude of this effect is similar to that seen in studies of ACE inhibitors in patients with type I diabetes, suggesting that disease progression can be halted by blockade of the renin-angiotensin system at this stage of the disease process. It also suggests the aetiology of the nephropathy associated with type 1 and type 2 diabetes is similar.
Lewis et al (2001) assessed the effects of 300 mg irbesartan and 10 mg amlodipine in 1715 patients with type 2 diabetes, hypertension and proteinuria of at least 0.9 g/day. The control group could use any antihypertensive agent except ACE inhibitors, AIIRAs and calcium channel blockers. Target blood pressure was 135/85 mmHg or a 10 mmHg reduction in systolic pressure if pressure at baseline was >145 mmHg. Primary outcome was a combination of renal events (doubling of serum creatinine, onset of end-stage renal disease) and all-cause mortality. Secondary outcome was a composite of cardiovascular related events and limb amputation above the ankle.
At the study end, blood pressure was significantly lower in the active treatment groups than in the control group. There was a 19% reduction in morbidity with irbesartan and the number of patients reaching the primary endpoint. This effect was not seen in the amlodipine group, implying the effect was not due solely to blood pressure lowering (Lewis et al, 2001).
In a similar study with the same endpoints, but investigating the AIIRA losartan, there was a 16% reduction in the number of patients in the treatment group reaching the primary outcome (Brenner et al, 2001).
The results from these studies demonstrate that irbesartan can slow or reverse the progression of microalbuminuria to proteinuria, and that AIIRAs can delay the progression of diabetic nephropathy in patients with proteinuria and can reduce all-cause mortality. This effect appears to be due to blockade of the renin-angiotensin system, as no significant reduction in the primary outcome was seen with conventional treatment or amlodipine.
ACE inhibitors and AIIRAs in combination
In the candesartan and Iisinopril microalbuminuria study (Morgensen et al, 2000) the effects of dual blockade of the renin-angiotensin system were measured over 12 weeks in nearly 200 patients with type 2 diabetes, microalbuminuria and hypertension. Combination treatment with the two agents produced a greater blood pressure reduction and lower albuminary excretion loss than either treatment alone.
Conclusions
The inhibition of the renin-angiotensin system appears to slow the progression of diabetic nephropathy independently of antihypertensive effects. Indeed, the NSF Standards for Diabetes recommend treating patients with microalbuminuria or proteinuria with an ACE inhibitor, unless contraindicated, irrespective of the patient's blood pressure. Now, recent evidence shows that AIIRAs are effective in slowing the decline of renal function in type 2 diabetes and may present a viable alternative.
Berk BC, Vekshtein V, Gordon HM, Tsuda T (1989). Angiotensin II-stimulated protein synthesis in cultured vascular smooth muscle cells. Hypertension 13:305-14
Brenner BM, Cooper ME, de Zeeuw D et al (2001). Effects of Iosartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. New England Journal of Medicine 345:861-69
Department of Health (2003) National Service Framework for Diabetes: Delivery Strategy (http://www.doh.gov.uk/nsf/diabetes)
Fogo A, Yoshida Y. Yared A, Ichikawa I (1990). Importance of angiogenic action of angiotensin II in the glomerular growth of maturing kidneys. Kidney International 38: 1068-74
Heart Outcomes Prevention Evaluation (HOPE) Study Investigators (2000). Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet 35: 253-59
Kasiske BL, Kalil RSN, Ma JZ et al (1993). Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Annals of Internal Medicine 118:129-38
Kenny C (2002). Preventing nephropathy in patients with type 2 diabetes. Diabetes and Primary Care 4: 69-74
Kshirsagar AV, Joy MS. Hogan SL et al (2000). Effect of ACE inhibitors in diabetic and non-diabetic chronic renal disease: a systematic overview of randomised placebo-controlled trials. American Journal of Kidney Disease 35:695-707
Lewis EJ, Hunsicker LG, Clarke WR et al (2001). Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. New England Journal of Medicine 345: 851-60
Lewis EJ, Hunsicker LG. Bain RP et al (1993). The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy: The Collaborative Study Group. New England Journal of Medicine 329: 1456-62
Mogensen CE. Neldam S, Tikkanen I et al for the CALM study group (2000). Randomised controlled trial of dual blockade of renin-angiotenain system in patients with hypertension. microalbuminuria and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. British Medical Journal 321: 1440-44
Parving HH, Lehnert H, Brochner-Mortensen J et al (2001). The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. New England Journal of Medicine 345: 870-78
Remuzzi A, Puntorieri S, Battaglia C et al (1990). Angiotensin converting enzyme inhibition ameliorates glomerular filtration of macromolecules and water and lessens glomerular injury in the rat. Journal of Clinical Investigation 85: 541-49
The ACE Inhibitors in Diabetic Nephropathy Trials Group (2001). Should all patients with type I diabetes and microalbuminuria receive angiotensin-converting enzyme inhibitors: a meta-analysis of individual patient data. Annals of Internal Medicine 134: 370-79
UK Prospective Diabetes Study Group (1998). Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes. UKPDS 38. British Medical Journal 317: 703-13
Zatz R, Dunn BR, Meyer TW et al (1986). Prevention of diabetic glomerulopathy by pharmacological amelioration of glomerular capillary hypertension. J Clinical Investigation 77:1925-30
Zatz R, Meyer TW. Rennke HG, Brenner BM (1985). Predominance of hemodynamic rather than metabolic factors in the pathogenesis of diabetic glomerulopathy. Proceedings of the National Academy of Science of the United States of America 82: 5963-67
RELATED ARTICLE: ARTICLE POINTS
1 The NSF Standards or Diabetes state that patients with microalbuminuria or proteinuria should be treated with an ACE inhibitor unless contraindicated, irrespective of the patient's blood pressure status.
2 The renin-angiotensin system is involved in the development of diabetic nephropathy.
3 Inhibition of the renin-angiotensin system slows the progression of diabetic nephropathy by a mechanism that is independent of antihypertensive effects.
4 Three recently published studies have demonstrated that AIIRAs are also effective in slowing the decline of renal function in type 2 diabetes.
KEY WORDS
* Diabetic nephropathy
* Type 2 diabetes
* Microalbuminuria
* ACE inhibitors
* AIIRAs
PAGE POINTS
1 Angiotensin II acts on two sets of receptors: the [AT.sub.1] receptor which is responsible for the known physiological actions of angiotensin, and the [AT.sub.2] receptor whose function is still unknown.
2 Inhibition of the renin-angiotensin system and removal of the effects of angiotensin II can improve the glomerular haemodynamics in patients with diabetes.
PAGE POINTS
1 A number of meta-analyses have confirmed that ACE inhibitors significantly reduce progression to proteinuria and increase the chances of regression to normoalbuminuria in patients with type 1 diabetes.
2 The beneficial effects of ACE inhibition arise because of the lower circulating levels of angiotensin II and consequent decreased stimulation of the [AT.sub.1] receptor.
PAGE POINTS
1 Three studies have shown that AIIRAs are effective in slowing the decline of renal function in patients with type 2 diabetes.
2 Irbesartan delayed the progression to nephropathy in a dose-dependent fashion.
3 Irbesartan can slow or reverse the progression of microalbuminuria to proteinuria.
4 AIIRAs can delay the progression of diabetic nephropathy in patients with proteinuria and can reduce all-cause mortality.
PAGE POINTS
1 The inhibition of the renin-angiotensin system appears to slow the progression of diabetic nephropathy independently of antihypertensive effects.
2 Recent evidence shows that AIIRAs are effective in slowing the decline of renal function in type 2 diabetes and may present a viable alternative.
Colin Kenny is a GP in Dromore, Co Down
COPYRIGHT 2003 S.B. Communications
COPYRIGHT 2003 Gale Group