Introduction
The increasing prevalence of end-stage renal failure, its poor prognosis, and the evidence for interventions to prevent the development and progression of renal failure means that we should aim to optimise our practice in this area. Following a literature review, a practice in West Cumbria assessed the feasibility of achieving a target blood pressure of 130/180mmHg in microalbuminuric diabetic hypertensive patients through a 3-month intensive management plan. Results indicate that, due to limited resources, this target may not be feasible, although the plan did have a positive effect on glycaemic control.
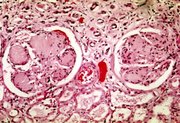
It is now well-established that there is a close link between diabetes (types 1 and 2) and end-stage renal failure (ESRF) (Ritz and Stefanski, 1996).
Over the past 20 years there has been a steady increase in the incidence of ESRF, mainly in people with type 2 diabetes, to the extent that around one-third of the US diabetes population now has coexistent ESRF (Ritx et al, 2002). This may well be explained by the concomitant control of other cardiovascular risk factors, which results in longevity and allows time for ESRF to develop.
What is clear is that once ESRF has developed, the prognosis is very similar to that of metastasised gastrointestinal carcinoma, and this alone warrants the aggressive management of any associated risk factors.
Risk factors for the development of nephropathy
One of the strongest risk factors for the development of nephropathy is family history (US Renal Data System, 1998). A family history of cardiovascular events is also a powerful indicator of risk.
Other risk factors that are more amenable to modification have also been identified, including blood pressure, [HbA.sub.1c] and cholesterol concentrations, smoking and, possibly, high dietary protein intake (Kelter et al, 1996; David et al, 1998).
Practice audit
While carrying out an audit on control of hypertension in type 2 diabetes, it became clear that the group of patients who had coexistent renal disease were very poorly controlled. Indeed, none of 10 patients with type 2 diabetes and hypertension achieved the target blood pressure recommended in the British Cardiac Society guidelines (Wood et al, 1998). However, these guidelines may have been produced with a slant towards the prevention of coronary heart disease rather than renal failure.
Aim
I therefore decided to look at guidelines produced by nephrologists, and then determine whether my group of 10 patients could achieve better blood pressure control with the various methods of intervention available. The point of the exercise was to determine whether these 'trial population' guidelines could be reproduced in a general practice in West Cumbria, or whether, in fact, the targets are unachievable in day-to-day practice.
Target blood pressure
What level of blood pressure should we be aiming for in patients with diabetes and microalbuminuria?
In at least four out of five patients, hypertension or an abnormal circadian variation in blood pressure is found at the time of diagnosis of type 2 diabetes (Kelter et al, 1996). Both features are strongly correlated with the presence of albuminuria, and are powerful predictors of cardiovascular and renal damage. In 1997, evidence was published showing that antihypertensive treatment with [beta]-blockers and angiotensin-converting enzyme (ACE) inhibitors attenuated the progressive loss of renal function in type 2 diabetes (Nielson et al, 1997) on a long-term basis - the first proof that this treatment also delayed the otherwise inevitable decline to renal failure.
What was not clear was the most appropriate blood pressure target, the most appropriate agents to use and the most productive lifestyle interventions.
Evidence from clinical studies
The first question was answered by the Modification of Diet in Renal Disease Study (MDRDS, Peterson et al, 1995), which examined the relationship between proteinuria, prescribed and achieved blood pressure, and decline in glomerular filtration rate. The results supported the concept that proteinuria is an independent risk factor for the progression of renal disease.
Furthermore, recent evidence has shown that not only is urinary protein nephrotoxic, but also that the rate of protein excretion is a powerful predictor of progression (Yokoyama et al, 1997). In addition, a reduction in tubular protein, for example by ACE inhibition, reduces this toxic effect. For this reason, patients are now divided into two groups: those with mild microalbuminuria (urinary excretion < 1 g protein per day) and those with severe microalbuminuria (urinary excretion > 1 g protein per day).
MDRDS advised a target of 125/75 mmHg for those with proteinuria > l g/day, and 130/80 mmHg for those with proteinuria 0.25 g- 1 g/day. The authors also suggested that the extent to which lowering blood pressure reduced proteinuria may be a measure of the effectiveness of this intervention in slowing the progression of renal disease. In response to this, the National Kidney Foundation recommended that the target blood pressure should be 125/75 mmHg in patients with diabetic or non-diabetic renal disease.
On this side of the Atlantic, the UK Prospective Diabetes Study (UKPDS) showed that even moderate lowering of blood pressure leads to a major reduction in renal events (diastolic lowering from 90 to 80 mmHg leading to a 50% reduction).
There has been some concern that lowering blood pressure to 125/75 mmHg may be detrimental, particularly in the elderly, who may suffer postural symptoms or, even worse, ischaemia, although no convincing evidence of this has been found (Ransom and Zanchetti, 1998). It would, however, seem sensible to take care in patients with arteriosclerotic stenotic lesions, particularly of the carotids, and also those with neuropathy who may suffer profound postural hypertension when antihypertensive medication is combined with a diabetic autonomic neuropathy.
In the group of patients for whom I provide care, the majority at any one time, indeed all at the moment, have albuminuria < 1 g/day. It therefore seemed prudent, in light of the above evidence, to set a target blood pressure of 130/80 mmHg for these patients, as suggested by the MDRDS.
Possible interventions
Pharmacological
Patients with diabetes tend to retain sodium, and their hypertension is exquisitely volume-sensitive (Ismail and Becker, 1999). It would therefore seem appropriate to advise a salt-restricted diet, and to administer diuretics: thiazide if there is no evidence of renal failure, or a loop diuretic once the glomerular filtration rate starts to fall. Although diuretics in general tend to worsen glucose intolerance, the benefit from reducing blood pressure far outweighs the deleterious effect. ACE inhibitors have been shown, as discussed above, to slow down renal failure, but one of the most common reasons for their failure as an antihypertensive is sodium loading, and so concomitant administration with a natriuretic makes obvious sense.
Angiotensin II inhibitors have not yet been proven to be renoprotective in people with type 2 diabetes with advanced nephropathy. However, their antiproteinuric effects have been shown to be equivalent to those of ACE inhibitors in patients with diabetic or non-diabetic renal disease.
In general, calcium-channel blockers are less effective than ACE inhibitors in reducing albuminuria. However, the long-acting ones such as amlodipine and diltiazem have been shown to be equally efficacious (Welussi and Badco, 1996).
Despite these theoretical considerations, the underlying protection of nephrons relies on lowering the blood pressure, rather than the agent used (Ransom and Zanchetti, 1998). As in the UKPDS, other agents such as [beta]-blockers have been shown to be of considerable value in achieving this.
Whatever pharmacological methods are chosen, a combination of agents is almost certainly necessary to achieve the targets set (Peterson et al, 1995).
Concordance
Many factors are known to affect the discrepancy between what a doctor writes on a prescription, and what ultimately reaches the patient's target organ. The perceived primary factors have changed over the years; mainly patient factors, e.g. poor compliance, have given way to a less judgmental situation in which it is accepted that the doctor's role is as important, if not more important, in achieving a successful outcome, i.e. concordance (Table I).
Dietary
Trials such as the MDRDS (Petersen et al, 1995) showed not only that reduced dietary protein would directly slow the progression to ESRF, but also that any reduction in salt intake, and any reduction in calorie intake that reduced obesity, would indirectly slow the progression of the disease by reducing blood pressure.
Method
With all these factors in mind, I designed a management plan for my group of 10 patients with diabetes, hypertension and nephropathy.
Over I month, I invited all the patients to attend the diabetes clinic that I run every 2 weeks, to discuss what I intended to do. Along the lines of the DCCT (Diabetes Control and Complications Trial Research Group, 1993), my plan was to provide intensive input into this small group of patients over the following 3 months. This involved many members of the diabetic primary health care team (PHCT), including their GP, the practice nurse, district nurse, dietitian, the community diabetes liaison nurse, the health visitor, and the community pharmacist, as well as my nominated practice receptionist to control the appointments. A practice meeting involving all the above to discuss the proposed plans helped to achieve ownership of the plan.
Therapeutic changes
At lease once a month, blood pressure control was assessed by the GP and therapeutic adjustments were made. In the absence of contraindications or side-effects, patients were given a combination of ACE inhibitors, angiotensin II antagonists, diuretics, calcium-channel blockers, [beta]-blockers and [alpha]-blockers.
The ACE inhibitor used was ramipril, in light of the HOPE data. Candesartan was the angiotensin II antagonist of choice, owing to its dual excretion via kidney and liver.
Bendrofluazide was used for potent natriuresis, unless there was sufficient renal damage to cause elevated creatinine, in which case frusemide was substituted.
The long-acting calcium-channel blocker amlodipine was chosen for the reasons outlined above. Atenolol was used for its trusted safety profile and doxazosin was used as it seems to cause fewer side-effects with regard to postural hypotension compared with other [alpha]-blockers.
Concordance
Polypharmacy breeds lack of concordance particularly when the illness being treated is asymptomatic. Initially, this was assessed by repeat prescription monitoring. Having collected the prescription, cost was not an issue as diabetes treatment, apart from those solely on diet, is free. Access to a pharmacist was also unlikely to be an issue, owing to the location of the practice.
Three potential problem areas were size of tablets and side-effects, confusion due to polypharmacy and lack of understanding, and the value of treatment. To help combat these, I acquired samples of each of the tablets that I prescribe from the local pharmacist, both to show the patient and to see whether they felt they were able to swallow them, and to reduce confusion when discussing changes in medication.
After discussion with a representative from the pharmaceutical industry, I obtained some funding to pay for a supply of plastic pill organisers, so that the daily requirement of tablets could be organised on a weekly basis.
I sat down with all the clinical members of the team, to gain acceptance on the need for education of these patients at each consultation regarding their illness and treatment, and to ensure that we were all giving the same information.
Dietary advice
At the onset and at approximately 16 weeks, the patients were given advice regarding a low-salt diet, and a low-calorie diet if overweight, by the GP, the nurse or the dietitian. Along with this, they were given a handout to take away. For those who were overweight, an appointment was made to join a slimming group run by our health visitor.
Follow-up
As all the patients attend our diabetes clinic, most of the follow-up was provided by myself and the practice nurse. If possible and the patient was in agreement, this was carried out on at least a 2-weekly basis. The following interventions were performed at each visit:
* Check blood pressure twice, preferably 5 minutes apart.
* Check medication - side-effects, concordance, questions
* Weigh
* Discuss diet
* Assess for change in medication - increase if average blood pressure > 130/80mmHg over previous three visits
* Check understanding of the value of treatment and prescription regimen.
If the blood pressure was found to be uncontrolled, then follow-up was arranged weekly, with the appropriate biochemical monitoring when the renin-angiotensin system was modified.
Final interview
At the end of the project, each of the patients involved was interviewed, as was each of the main players of the PHCT, to gain some insight into their feelings regarding the value of all this intervention.
Results
As the 10 patients identified from the control of hypertension in type 2 diabetes audit were receiving regular follow-up in the practice-based diabetes clinic, arranging an initial interview was fairly straight-forward, with only four of them requiring early follow-up in the next 4 weeks.
Eight of the 10 patients agreed to further intervention in an attempt to reach target blood pressure levels after discussion. All received dietary advice; three of four patients with a BMI > 25 agreed to follow-up in our slimming group along with advice regarding weight loss. All eight continued follow-up at least fortnightly.
The modal number of different anti-hypertensive treatments was three at the start of the project, rising to four by the end of the project. The commonest regimen was a combination of ramipril, bendrofluazide, amlodipine and doxazosin. In five of the eight patients, their tablets had all been increased to a maximum strength, as suggested by the BNF; the other three were restricted to only 5 mg amlodipine due to intolerable ankle swelling when the strength was increased further.
According to the written notes, all eight patients received educational input, regarding their illness and their treatment, on at least four occasions.
Three of the patients were over the age of 70, and were very grateful for the suggestion and provision of a pill organiser to aid concordance -- as were their family who had previously, on several occasions, noticed maladministration.
With regard to the resultant control of their hypertension, at the onset of the project, seven of the eight patients were controlled to my previous standard of <I40/80 the other one averaging I52/84mmHg. At the end of the trial period, all were controlled to <140/80mmHg, but only one patient consistently had blood pressures recorded <I30/80mmHg, and one other patient had an average of <I30/80mmHg over the final three visits.
One interesting knock-on effect, perhaps in line with the DCCT findings, was that half these patients had a concomitant improvement in the glycaemic control of at least 0.5% [HbA.sub.1c]
Conclusions and recommendations
From my reading of the relevant literature, it has now become clear that microalbuminuria is a very potent indicator for the development of cardiovascular as well as renal damage, and that the degree of urinary protein excretion is linked in a proportional manner to the associated risk Several trials have shown that a reduction in the degree of proteinuria reduces risk, and that the reduction in blood pressure reduces the degree of proteinuria.
However, the results of my short-term intervention, in a manner that I feel was as intense as is practicable in a general practice, lead me to suggest that the published targets are overambitious. My feeling is that, as suggested by the law of diminishing returns, a target of I40/80mmHg for patients with diabetes, hypertension and microalbuminuria is quite achievable in my working environment, as with the remainder of the diabetes population. However, the gain achieved by further reduction to I30/80mmHg is probably outweighed by the cost of time and money, which may well be better spent elsewhere in other branches of our professional life.
There was, however, the interesting knock-on effect regarding improved glycaemic control. This may well be due to the attention given in general to educating our patients about diabetes, and maybe by some psychological benefit from our acceptance of concordance as an issue, rather than compliance.
The patient's perspective of this project was that, perhaps as expected, they were very grateful for all the time and effort invested in them and their illness; the only downside was that it had to be explained that this level of care was not sustainable with regard to time!
The staff were happy to have been involved in some scientific analysis in the practice, but, again in relation to the time factor, seemed relieved that it had not shown sufficient benefit to warrant continuation!
David M, Brash D et al (1998) Main risk factors for nephropathy in type 2 diabetes mellitus are plasma cholesterol levels, mean blood pressure and hyperglycemia. Archives of Internal Medicine 11:998-1004
Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment on the development and progression of long term complications in insulin dependent diabetes mellitus. New England Journal of Medicine 329:977-986
HOPE (2000) (Heart Outcomes Prevention Evaluation) Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICROHOPE substudy. Lancet 355:235-9
Ismail N, Becker B (1999) Renal disease and hypertension in non-insulin dependent diabetes mellitus. Kidney International 55: I-28
Kelter CG, Bergis KH, Fliser D, Ritz E (1996) Renal findings in patients with short term type 2 diabetes. Journal of the American Society of Nephrology 7: 2627-35
Nielson FS, Lessing, Petal (1997) Long term effect of lisinopril and atenolol on kidney function in hypertensive NIDDM subjects with diabetic nephropathy. Diabetes 46:82-8
Peterson JC, Adler S et al (1995) Blood pressure control, proteinuria, and the progression of renal disease. The Modification of Diet in Renal Disease Study. Archives of Internal Medicine 12:754-62
Ransom L, Zanchetti A (1998) Effect of intensive blood pressure lowering and low-dose aspirin in patients with hypertension -- principal results of the hypertension optimal treatment randomised trial. The Lancet 351:1755-62
Ritx E, Rychlik I et al (2002) End stage renal failure in type 2 diabetes -- a medical catastrophe of worldwide dimensions. American Journal of Kidney Disease. (in press)
Ritz E, Stefanski A (1996) Diabetic nephropathy in type 2 diabetes. American Journal of Kidney Disease 27:67-94
US Renal Data System (1998) Annual Data Report National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, US
Welussi M, Badco E (1996) Effects of cilazapril and amlodipine on kidney function in hypertensive NIDDM patients. Diabetes 45: 216-22
Wood D et al (1998) Joint British recommendations on prevention of coronary heart disease in clinical practice. Heart 80 (suppl 2)
Yakoyama H, Tomosaga O et al (1997) Predictors of the progression of diabetic nephropathy and the beneficial effect of angiotensin-converting enzyme inhibitors in NIDDM patients. Diabetologio 40:405-11
RELATED ARTICLE: ARTICLE POINTS
1 The poor prognosis of end-stage renal failure warrants aggressive management of risk factors.
2 An audit at a practice in West Cumbria found poor blood pressure (BP) control in diabetic hypertensive nephropathy patients.
3 Following literature review, a target BP of 130/80mmHg was suggested for the microalbuminuric subgroup.
4 A 3-month intensive management plan was put into effect for these patients.
5 It was concluded that a target BP of 140/80mmHg is more practicable in everyday practice.
KEY WORDS
* Nephropathy
* Target blood pressure
* Audit
* Intensive management
PAGE POINTS
1 It has been shown that proteinuria is an independent risk factor for the progression of renal disease.
2 Recent evidence has also shown that the rate of protein excretion is a powerful predictor of progression of renal disease.
3 In light of the literature on the subject, we set a target BP of 130/80 mmHg for our diabetic hypertensive microalbuminuric patients.
4 Possible pharmacological interventions include diuretics, ACE inhibitors, [beta]-blockers and angiotensin II inhibitors.
PAGE POINTS
1 Many factors are known to affect the discrepancy between what a doctor writes on a prescription, and what ultimately reaches the patient's target organ.
2 Over 3 months, all 10 diabetic hypertensive microalbuminuric patients at our practice received an intensive management plan.
3 Initially, concordance was assessed by repeat prescription monitoring.
PAGE POINTS
1 Dietary advice covered a low-salt diet, and a low-calorie diet if overweight.
2 Most of the follow-up was provided by the GP and the practice nurse, and took place at least every 2 weeks if possible and the patient agreed.
3 At the end 3 of the project, interviews were carried out with each of the patients involved.
4 Eight of the ten patients agreed to further intervention in an attempt to reach target blood pressures after discussion.
PAGE POINTS
1 At the end of the trial period, all eight patients had a BP below 140/80mrnHg, with only one patient consistently below the set target of 130/80mmHg.
2 Four of the patients had a concomitant improvement in their glycaemic control.
3 It was concluded that the gains achieved by a BP reduction from 140/80 to 130/80 mmHg may be outweighed by the cost in time and money
Richard Tranter is a CP Principal in Whitehaven, Cumbria,
COPYRIGHT 2002 S.B. Communications
COPYRIGHT 2003 Gale Group