We followed eight patients with Duchenne-type muscular dystrophy for an average of 39 months after initiation of noninvasive intermittent ventilatory assistance using body ventilators. After one to three months of nocturnal use averaging 8 h, mean daytime [PaCO.sub.2] fell from 63[+ or -]2 to 45[+ or -]3 mm Hg. At late follow-up, [PaCO.sub.2] remained stable at 47[+ or -]4 mm Hg, but vital capacity fell 33 percent compared with the initial value and the average duration of ventilator use had increased to 18[+ or -]2 h daily. Three patients died and five survived; two continued using negative pressure ventilators and three had tracheostomies placed for administration of positive pressure ventilation. We conclude that noninvasive intermittent ventilatory assistance effectively reverses hypoventilation and symptoms in patients with late-stage Duchenne muscular dystrophy, but pulmonary function continues to deteriorate necessitating longer periods of ventilation, and often tracheostomy, within a few years.
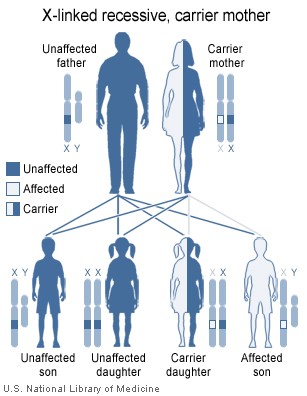
Duchenne and Duchenne-type muscular dystrophies are x-linked recessive hereditary disorders characterized by diffuse skeletal and cardiac muscle involvement.[1,2] They lead inexorably to quadraparesis in the preteen years and death due to respiratory failure at an average age of 20 years or slightly older for the more slowly progressive Duchenne-type dystrophies.[2,3] Although the use of ventilatory support for the treatment of respiratory failure in these patients is controversial,[4,5] noninvasive intermittent ventilatory assistance has been shown to effect sustained stabilization and even reversal of hypoventilation.[6-10] However, the long-term efficacy of intermittent ventilatory assistance in patients with Duchenne-type muscular dystrophy has not been fully evaluated. In this report, we retrospectively examine the clinical course, further decline in pulmonary function, and changing requirements for ventilatory assistance in eight patients with Duchenne-type muscular dystrophy observed for an average of 39 months after the initiation of intermittent ventilatory assistance.
METHODS
Patients were referred for the management of hypercarbia from the Muscular Dystrophy Association Clinic at New England Medical Center. Patients had been diagnosed as having Duchenne or Duchenne-type muscular dystrophy using standard clinical criteria including male sex, elevation of creatine phosphokinase, and a compatible muscle biopsy and clinical picture. All patients were in functional class [9.sup.3] and had severe quadraparesis.
All patients expressed a desire to try intermittent ventilatory assistance and were hospitalized for four to seven days to undergo an initial trial. Baseline studies included pulmonary function studies consisting of spirometry and measurement of lung volumes (P.K. Morgan, Inc.), and room air arterial blood gas values (Radiometer, Inc., Copenhagen) obtained while the patient was seated. The patients were then introduced to a variety of "body" ventilators including negative pressure devices (tank ventilators [iron lung and Portalung] Pneumowrap and chest shell), positive pressure-assisted ventilation administered via a face or nose mask or lip seal, or a Pneumobelt. Devices to be tested were selected based on patient preference and body habitus, as previously described.[11]
Not all patients tried all ventilators, but six of the eight tried both negative and positive pressure devices. Initial settings on the ventilator were selected to augment expired minute ventilation approximately 25 percent over baseline, and fine adjustments were made to optimize patient comfort. The ventilator for long-term use was selected by the patient as long as it was capable of augmenting minute ventilation by at least 25 percent, and patients remained in the hospital for two to three additional nights to familiarize themselves with nocturnal use of the ventilator. To optimize patient acceptance, ventilator use was initiated during the evening for several hours and was gradually extended through the night. Following discharge, a home respiratory care provider checked on the patient frequently until he developed a stabilized routine for ventilator use.
Following discharge, two additional studies were performed. To determine whether alterations in arterial blood gas tensions or respiratory muscle fatigue occurred during the daytime period of spontaneous ventilation, four patients were studied at home within one-half hour of finishing night-time ventilator use, and again on the same day one-half hour before resuming ventilator use. Studies consisted of measurement of spontaneous breathing rate, minute ventilation, vital capacity and maximal voluntary ventilation for 12 s using an Eagle 2 spirometer (Warren E. Collins, Inc., Braintree, MA), and maximal inspiratory and expiratory pressures from FRC using a hand-held manometer (Boehringer Laboratories, Wynnewood, PA). Arterial blood gas values were determined while the patient sat at home breathing room air. Samples were transported on ice to the hospital where gas tensions were measured within 1 h of obtaining them.
To determine whether nocturnal desaturations were occurring in our patients, as has been reported in other patients with neuromuscular disease using negative pressure ventilators,[12] we monitored blood oxygen saturation overnight in three patients using a portable finger oximeter (Ohmeda Biox IVA, Englewood, CO).
For statistical comparisons, we used paired t-tests for comparisons of paired means, and analysis of variance for repeated measures for serial samples. For significant F ratios, we used the Student-Newman-Keuls test for comparisons of individual means.[13] Data are mean[+ or -]SE. Differences were considered significant when p<0.05.
RESULTS
Table 1 shows age at initiation of assisted ventilation, respiratory parameters at initiation of assisted ventilation and at times of early and extended follow-up and clinical outcome in the eight patients comprising our series. Most patients developed respiratory failure at approximately 20 years of age, as is typical for Duchenne muscular dystrophy. Delayed onset in patients 1 and 6 suggests that they may have had a more slowly progressing variety. All patients had severe restriction of their vital capacities and severe hypercarbia at the time that ventilatory assistance was initiated.
All patients had gradually worsening symptoms of chronic hypercarbia including morning headache and loss of energy for several weeks to months prior to initial presentation, but none had symptoms of an acute respiratory illness. Patient 6 complained of cough productive of clear secretions for three weeks prior to presentation. Patients 4 and 6 complained of weakened voice, and only one, patient 2, had dyspnea at initial presentation. The latter patient was also the only one to develop signs of congestive heart failure, including peripheral edema and transudative pleural effusions, during his subsequent course.
Although six of the eight patients tried positive pressure ventilation administered via a face mask, lip seal or nose mask, all six preferred other forms of assisted ventilation; five of the six chose a negative pressure ventilator and one chose a Pneumobelt. Among the negative pressure ventilators, the tank ventilator and Pneumowrap were selected by four and three patients, respectively. The requirement that the Pneumobelt be used in no less than a 45 [degrees] semirecumbent position[11] limits its acceptability for nocturnal ventilation, but the one patient who selected it learned to sleep in the sitting position. Patient 6 used the Pneumobelt in the afternoon in addition to using the Pneumowrap at night. [TABULAR DATA OMITTED]
At the time of discharge from their initial hospitalization, most patients were using their ventilators no more than 3 to 5 h nightly and reversal of daytime hypercarbia was minimal. However, as they gradually extended hours of use and learned to sleep with the ventilator, [PaCO.sub.2] gradually fell to the 40 to 50 range after one to three months of nocturnal ventilator use, as shown in Table 1. Symptoms of morning headache resolved and energy level was improved in all patients and weakened voice and dyspnea were improved in affected patients. The average duration of use at initial follow-up was 8 h. Although only a few measurements of FVC were obtained at early follow-up, no consistent changes were observed.
At extended follow-up, averaging 39 months, the mean number of hours of ventilator use increased to 18 h/24 h, and FVC fell significantly, an average of 33 percent among the five patients in whom follow-up measurements were available. The increase in hours of use of the ventilator was apparently able to compensate for the reduction in pulmonary function because [PaCO.sub.2] remained stable at extended follow-up in comparison with early follow-up. Figure 1 shows these trends in FVC, [PaCO.sub.2] and hours of ventilator use during the follow-up period.
Following initiation of nocturnal ventilatory assistance, five of our eight patients required only one hospitalization for respiratory problems and one patient had no hospitalizations in more than five years. Patient 6 required repeated hospitalizations because of inability to clear secretions and patient 2 had multiple hospitalizations, several related to his severe underlying cardiomyopathy. Three patients died during the extended follow-up period, one of pneumonia when he declined endotracheal intubation. The other two had severe cardiomyopathy and experienced sudden death, one while using the iron lung. Autopsies were not performed. [TABULAR DATA OMITTED]
Figure 2 summarizes the use of ventilators during the extended follow-up period. Patient 4 used the Pneumobelt for gradually increasing periods of time until he developed pneumonia at 26 months. Tracheostomy was performed when he could not tolerate lying in the supine position in a tank ventilator, and he has remained clinically stable subsequently. Among the three patients who began using the Pneumowrap, two switched to the iron lung after three and ten months of nocturnal ventilation, respectively. The iron lung was selected because it provided greater ventilatory assistance and helped in mobilizing secretions. Among the four patients who began using a tank ventilator, one died suddenly, two remained stable while gradually increasing their daily amount of ventilator use and one elected tracheostomy rather than spend up to 20 h in the iron lung every day.
Patients 1, 5 and 7 underwent overnight oximetry monitoring while using their negative pressure ventilators. Mean minimum oxygen saturation during 9[+ or -]1 h of monitoring was 88[+ or -]2 percent, and oxygen saturation was below 90 percent for less than 1 percent of the time.
Table 2 shows respiratory parameters obtained immediately after and immediately before nocturnal ventilator use within the same 24-h period. Among the four patients studied in their homes, there were no significant changes in respiratory rate, minute ventilation, maximal inspiratory and expiratory pressures, vital capacity, MVV or arterial blood gas values during the periods of spontaneous ventilation that averaged 11 h.
DISCUSSION
In our series of eight patients with Duchenne or Duchenne-type muscular dystrophy with respiratory failure, we found, as others have,[6-10] that nocturnal ventilatory assistance using noninvasive ventilators brought about a sustained reversal of hypoventilation and improvement in symptoms of chronic hypercarbia. The clinical course was stabilized in most patients who required infrequent hospitalizations despite minimal pulmonary reserve. Although our patients tried a variety of negative and positive pressure ventilators, they preferred negative pressure ventilators and particularly the tank ventilator because it was effective, comfortable and left the upper airway free. Recently, however, as others have reported,[14,15] we have had success in assisting ventilation in patients with muscular dystrophy and other restrictive lung diseases using positive pressure ventilation administered via a nose mask.
Our patients initiated use of assisted ventilation when they had developed symptomatic hypercarbia prior to the onset of superimposed acute respiratory failure. By beginning assisted ventilation at this phase of their illness, we were able to initiate ventilatory assistance gradually and hypercarbia was reversed very slowly over a period of weeks. Splaingard et al[9] have advocated a similar approach, arguing that a lengthy and expensive hospitalization for an eventual acute deterioration could thereby be avoided.
Although the reversal of hypoventilation in our patients was sustained, we detected a gradual and progressive loss of pulmonary function, amounting to approximately 33 percent of vital capacity over the three and one-quarter year follow-up period. In order to compensate for this loss of function and maintain a stable [PaCO.sub.2], patients gradually increased the duration of ventilatory assistance so that after the extended follow-up period, the duration of daily use was more than double that at the early follow-up period. In addition, patients gradually retreated to more effective and invasive forms of assisted ventilation including the iron lung and positive pressure administered via a permanent tracheostomy.
Lacking a control group in our study, we cannot ascertain whether long-term noninvasive ventilatory assistance was influencing the rate of loss of vital capacity in any way or whether survival was prolonged. No other controlled trials addressing these issues have been reported. However, prior studies on pulmonary function in patients with Duchenne muscular dystrophy not given ventilatory support have rarely detected chronic hypercarbia, even in patients with severe restriction,[16,17] and have considered elevation of [PaCO.sub.2] a preterminal and irreversible event.[3] Rideau et al[2] have described ascending, plateau and descending phases for alterations of vital capacity in Duchenne muscular dystrophy, the onset of the latter phase presaging terminal respiratory insufficiency within several years at an average age of 20 years. A decline in vital capacity to less than 500 ml has been associated with imminent death in untreated patients.[18] Considering these observations on the natural history of respiratory insufficiency in Duchenne muscular dystrophy, it seems highly likely that survival was prolonged in at least some of our patients, particularly in patients 1 and 8, who have lived for more than five years following the onset of hypercarbia. Furthermore, our patients sought treatment for worsening symptoms. Withholding a treatment that has been shown to reliably reverse symptoms and hypercarbia[6-10] when the prognosis without intervention is so poor seems unjustifiable. On the other hand, controlled studies are needed to determine whether or not nocturnal ventilatory assistance initiated prior to the onset of hypercarbia slows deterioration of pulmonary function, as some have suggested.[18]
Others have reported nocturnal arterial oxygen desaturations due to upper airway obstruction in patients with neuromuscular diseases (only one with muscular dystrophy) using negative pressure ventilators.[12] We observed no significant nocturnal oxygen desaturations in our series, although we were able to monitor only three patients. We encountered no difficulty reversing hypoventilation or symptoms, nor were there any indications of upper airway obstruction during hospitalizations in the remaining five patients. Although we may have missed desaturations in these remaining patients, upper airway obstruction during ventilator use did not perceptibly interfere with our patient management. It is possible that patients with Duchenne muscular dystrophy are less susceptible to this problem than those with other neuromuscular diseases.
The lack of change in parameters of pulmonary function and arterial blood gas values during a period of 11 h of spontaneous breathing in four of our patients indicates that our patients remained stable off the ventilator and that blood gas levels obtained at mid-day or late during the period of spontaneous ventilation are representative of the patient's sustained level of ventilation. This stability during the period of spontaneous ventilation also demonstrates that evidence of respiratory muscle fatigue did not occur between intervals of assisted ventilation.
The mechanism by which nocturnal ventilatory assistance reverses hypoventilation is not known with certainty. One theory proposes that intermittent ventilation provides rest for fatigued respiratory muscles, allowing for greater levels of sustained ventilation after resting.[19] A second theory proposes that ventilatory assistance at night prevents the nocturnal hypoventilation that blunts respiratory drive, resulting in a gradual resetting of the respiratory center and increasing ventilatory responsiveness to [CO.sup.2.][20,21] We cannot confirm or disprove either theory based on our study, nor are they mutually exclusive. However, if reversal of hypoventilation is related to reversal of muscle fatigue, one might predict that FVC would improve after a few months of assisted ventialation and that evidence of muscle fatigue would occur after a sustained period of spontaneous ventilation. Although we studied only a small number of patients, we could not confirm these predictions. We cannot exclude the possibility that muscle fatigue develops during longer periods of spontaneous breathing, but nocturnal assisted ventilation had no discernible effect on the parameters of respiratory muscle function that we studied. Prevention of nocturnal hypoventilation, as demonstrated by Goldstein et al,[22] with a gradual downward resetting of the respiratory center, remains a possible explanation for the sustained reversal of hypoventilation in our patients.
In our eight patients with Duchenne or Duchenne-type muscular dystrophy supported with nocturnal ventilatory assistance over an average of 39 months, we observed an early reversal of hypoventilation and stabilization of the clinical course. However, the underlying muscular dystrophy relentlessly progressed necessitating increased periods of ventilatory assistance and changes to more effacacious and invasive ventilators such as the iron lung or positive pressure ventilation via a permanent tracheostomy. Although the clinical course varied considerably between patients after initiation of nocturnal ventilatory assistance, our findings demonstrate that intermittent noninvasive assisted ventilation in Duchenne muscular dystrophy is of temporary benefit, with most patients requiring almost continuous ventilatory support within a few years. These observations should be useful in counseling patients with muscular dystrophy and their families regarding modes of ventilatory assistance.
ADDENDUM
Since acceptance of this manuscript, patient 4 died suddenly 62 months after initiation of ventilation when his ventilator became accidentally detached from his tracheostomy tube. Autopsy revealed a well-healed tracheostomy without stricture, severe dystrophy of skeletal muscle, and moderate fatty infiltration of the myocardium without evidence of cardiac failure.
REFERENCES
[1] Gilroy J, Cahalan JL, Berman R, Newman M. Cardiac and pulmonary complications in Duchenne's progressive muscular dystrophy. Circulation 1963; 27:484-93
[2] Rideau Y, Jankowski LW, Grellet J. Respiratory function in the muscular dystrophies. Muscle Nerve 1981; 4:155-64
[3] Inkley SR, Oldenburg FC, Vignos PJ. Pulmonary function in Duchenne muscular dystrophy related to stage of disease. Am J Med 1974; 56:297-306
[4] Smith PEM, Calverly PMA, Edwards RHT, Evans GA, Campbell EJM. Practical problems in the respiratory care of patients with muscular dystrophy. N Engl J Med 1987; 316:1197-1205
[5] Colbert AP, Schock NC. Respiratory use in progressive neuromuscular diseases. Arch Phys Med Rehabil 1985; 66:760-62
[6] Alexander MA, Johnson EW, Petty J, Stauch D. Mechanical ventilation of patients with late stage Duchenne muscular dystrophy: management in the home. Arch Phys Med Rehabil 1979; 60:289-92
[7] Bach J, Alba A, Pilkington LA, Lee M. Long-term rehabilitation in advanced stage of childhood onset, rapidly progressive muscular dystrophy. Arch Phys Med Rehabil 1981; 62:328-31
[8] Curran FJ. Night ventilation by body respirators for patients in chronic respiratory failure due to late stage Duchenne muscular dystrophy. Arch Phys Med Rehabil 1981; 62:270-74
[9] Splaingard ML, Frates RC, Jefferson LS, Rosen CL, Harrison GM. Home negative pressure ventilation: report of 20 years experience in patients with neuromuscular disease. Arch Phys Med Rehabil 1985; 66:239-42
[10] Bach JR, O'Brien J, Krotenberg R, Alba AS. Management of end stage respiratory failure in Duchenne muscular dystrophy. Muscle Nerve 1987; 10:177-82
[11] Hill NS. Clinical applications of body ventilators. Chest 1986; 90:897-905
[12] Ellis ER, Bye PTP, Bruderer JW, Sullivan CE. Treatment of respiratory failure during sleep in patients with neuromuscular disease. Am Rev Respir Dis 1987; 135:148-52
[13] Steel RCD, Torrie JH. Principles and procedures of statistics. New York: McGraw-Hill, 1960
[14] DiMarco AF, Connors AF, Altose MD. Management of chronic alveolar hypoventilation with nasal positive pressure breathing. Chest 1987; 92:952-54
[15] Kerby GR, Mayer LS, Pingleton SK. Nocturnal positive pressure ventilation via nasal mask. Am Rev Respir Dis 1987; 135:738-40
[16] Hapke FJ, Meek JC, Jacobs J. Pulmonary function in progressive muscular dystrophy. Chest 1972; 61:41-47
[17] Buchsbaum HW, Martin WA, Turino GM, Rowland LP. Chronic alveolar hypoventilation due to muscular dystrophy. Neurology 1968; 18:319-27
[18] Rideau Y. The Duchenne muscular dystrophy child: care of the wheelchair-dependent patient, death prevention. Muscle Nerve 1986; 9(Suppl 5):86
[19] Braun NMT, Faulkner J, Hughes RL, Roussos C, Sahgal V. When should respiratory muscles be exercised? Chest 1983; 84:76-84
[20] Roussos C. Function and fatigue of respiratory muscles. Chest 1985; 88:1245-1325
[21] Ellis ER, Grunstein RR, Chan S, Bye PTP, Sullivan CE. Noninvasive ventilatory support during sleep improves respiratory failure in kyphoscoliosis. Chest 1988; 94:811-15
[22] Goldstein RS, Molotiu N, Skrastins R, Long S, DeRosie J, Contreras M, et al. Reversal of sleep-induced hypoventilation and chronic respiratory failure by nocturnal negative pressure ventilation in patients with restrictive ventilatory impairment. Am Rev Respir Dis 1987; 135:1049-55
COPYRIGHT 1990 American College of Chest Physicians
COPYRIGHT 2004 Gale Group