Abstract
Cervical cancer is the second-most common cancer in young women and is one of the most common causes of cancer deaths among women, particularly in minorities and in impoverished countries. Cervical dysplasia, a premalignant lesion that can progress to cervical cancer, is caused primarily by a sexually transmitted infection with an oncogenic strain of the human papillomavirus (HPV). Not all women with the virus develop cervical dysplasia or cervical cancer. It has been postulated there are multiple host factors that contribute to progression of disease. Many of these factors, such as nutrient deficiencies, can be reversed, which will result in regression of dysplastic lesions. Studies have shown dietary intervention and nutrient supplementation to be effective in preventing cervical cancer. Additionally, local escharotic treatment combined with systemic treatment shows significant potential in reducing dysplasia. Recent advances in vaccination technology demonstrate the effectiveness of an HPV vaccine. The vaccine, however, may have many social and cost-prohibiting limitations, as well as health side effects.
Introduction and Epidemiology
Cervical dysplasia is a premalignant lesion that can progress to cervical cancer, a common epithelial cancer that is the second-most common cancer in women age 20-39 years. (1) It disproportionately affects minority women and women living in underdeveloped countries. (2) Internationally, invasive cervical cancer accounts for 11.6 percent of all cancers. For every case of invasive cancer there are an estimated 50 cases of abnormal cervical smears that require monitoring and follow-up. (3) Current evidence suggests this lesion is primarily caused by a sexually transmitted infection with an oncogenic strain of the human papillomavirus (HPV). However, since this viral genome is found in healthy women as well as in healthy tissue adjacent to neoplastic lesions, factors unique to individual hosts appear to contribute to disease progression and dysplastic transformation.
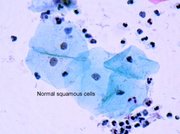
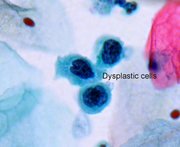
Invasive cervical cancer develops from precursor lesions of the cervix called cervical intraepithelial neoplasia (CIN). Progression from normal tissue to invasive cervical cancer occurs through a series of increasing grades of cervical dysplasia (Figure 1). CIN I represents mild dysplasia and has a high rate of spontaneous remission (60%) and a low rate of progression to carcinoma. In contrast, approximately 38 percent of CIN II and III, moderate to severe dysplasia, will spontaneously regress, and 16-36 percent will progress to invasive cervical cancer. (4) Because reporting for CIN is not mandatory, the exact incidence is unknown. However, it is estimated that 2.5 million women are diagnosed with low-grade cervical abnormalities annually. (5)
[FIGURE 1 OMITTED]
Routine PAP smear screening is widely credited with reducing cervical carcinoma from the first to the eighth leading cause of cancer death in the United States, but the number of deaths attributable to the disease is still high (approximately 4,900 deaths). Additionally, the medical costs of providing PAP screening are considerable and a significant economic burden to health care systems. (6) Millions of ablative procedures (e.g. cryotherapy, electrocautery, cone biopsy) are performed each year as an approach to treatment. Screening is not available to all women, mainly due to lack of insurance or lack of insurance-wellness plans. In countries without screening, cervical cancer is the leading cause of cancer death in women.
Risk Factors
It is undisputed that infection with sexually acquired HPV is the primary risk factor for cervical cancer and plays a critical role in cervical carcinogenesis. (7,8) Several other cofactors have been implicated in the progression of low-grade to high-grade lesions and/or the development of cervical cancer, but these remain controversial in clinical trials. (9) These include early age at first intercourse, history of multiple sexual partners, oral contraceptive use, (10) high parity, low socioeconomic status, poor diet, cigarette smoking, (11) immunosuppression, (12) and promiscuous male sexual partners. (13) In one study, with respect to current use, the risk for cervical dysplasia increased for women who had been using oral contraceptives longer than 10 years. (14) A summary of risk factors is outlined in Table 1.
The correlation between cervical dysplasia and oral contraceptives is based on the premise that steroid hormones, such as estrogen and progesterone, are thought to play a role in the progression of disease. Progesterone has been reported to increase HPV-16 and HPV-18 gene expression at the levels of transcription and mRNA stability. (15,16) Most cases of cervical cancer are in the most estrogen-sensitive region of the cervix known as the transformation zone, (17) an area that displays a high level of conversion of estradiol to 16[alpha]-hydroxyestrone. When HPV-16 DNA immortalizes these cells, this activity increases eightfold. (18) Furthermore, the incidence of HPV DNA in exfoliated cervical cancer cells increases during pregnancy when estrogen levels are highest. (19)
The prevalence of HPV has steadily risen over the past few decades. In the United States, the Centers for Disease Control documented a 459-percent rise in the number of visits to private clinics for condyloma acuminata, a genital lesion caused by HPV, between 1966 and 1981. (20) That number continues to rise. Based on data from a cohort of 22-year-old Finnish women, an estimated 79 percent of Finnish women between the ages of 20 and 79 will contract at least one HPV infection. (21)
Certain HPV types are associated with certain types of disease, although a given HPV type can cause a range of diseases. HPV are double-stranded DNA viruses of approximately 8,000 base pairs. Over 60 types of HPV have been identified. HPV types 6 and 11 are considered low risk and are commonly associated with condyloma acuminata of the lower genital tract and flat cervical condyloma. The medium risk groups, HPV types 33, 35, 39, 40, 43, 45, 51-56, and 58, are associated with low-grade genital dysplasia and carcinomas. The high-risk group of HPV types 16, 18, and 31 are associated with CIN III and malignant neoplasia of the penis, cervix, vulva, and perineum (Table 2). (22)
Although risk for cervical cancer is significantly higher with the presence of HPV infection, HPV infection alone may be insufficient to cause cervical cancer. Approximately 28 percent of women with HPV go on to develop CIN. (23) Current studies indicate HPV exposure is the initiating event. However, for the lesion to be persistent or progress to cervical cancer, other risk factors must be present. Over the past two decades, numerous epidemiological and laboratory studies have suggested nutritional factors may play an important role in the development and progression of CIN and cervical cancer.
Primary Prevention
Because a number of important epidemiological risk factors have been identified as contributing to the development of CIN and cervical cancer, primary prevention should be geared toward risk reduction. Of utmost importance with regard to risk reduction is the elimination of risky sexual behavior that increases exposure to HPV. Such behaviors include early sexual experiences, number of sex partners, and male partner factors such as history of venereal disease and number of sex partners. (24-26) The target population is primarily adolescents and young adults. (27) Women are most susceptible to potential carcinogens such as HPV during this period. (28)
It has been proposed that adolescents are at a greater risk for cervical dysplasia than adult females because of biological changes occurring in the cervix during puberty. (29) A study conducted by Massad and Anoina reported that cervical dysplasia is prevalent in as many as 21 percent of adolescent females. (30) In this population, sexual behaviors are initiated and lifelong patterns are established. Among sexually active adolescents, interventions should include increased condom use, improved communication with partners and peers, and addressing risk behaviors. It is also important for women to understand they can be infected with different strains of HPV with a new partner. Existing infection often lowers host immunity and makes women more susceptible to additional strains of HPV as well as other sexually transmitted diseases. Additionally, risk factors such as smoking need to be addressed at this time. There appears to be a significant correlation between risk of dysplasia and cigarette consumption. One study demonstrates the risk for cervical dysplasia rises with increased number of sex partners, dependent on the number of cigarettes smoked. (31)
Nutritional Intervention
Chemoprevention is an attempt to use natural and synthetic compounds to intervene in early pre-cancerous stages of carcinogenesis before invasive diseases begin. Cervical dysplasia is ideally suited to chemopreventive measures given its well-established pre-invasive state, its multi-step progression toward invasive disease, and the clinical diagnostic ease that allows practitioners to follow the lesion without significant invasive techniques. Nutritional intervention is ideally suited as a means of chemoprevention. Adjusting nutrient deficiencies ill women at risk of disease progression has been shown to prevent cancel from occurring.
Diet
Epidemiological studies suggest increased consumption of fruits and vegetables containing antioxidants is associated with lower risks for malignancies. (32-35) Fruits and vegetables are the primary dietary source of carotenoids, vitamin C, and folate, as well as other anticarcinogenic compounds, which may have synergistic effects. Results from a randomized controlled dietary intervention study of 53 premenopausal women demonstrated that dietary intervention could effectively promote increased fruit and vegetable intake. (36) The intervention improved status for both plasma carotenoids and folate in the target population, as well as a reduction in total plasma homocysteine. Participants were randomly assigned to a control group or a dietary intervention group and were followed for one year. The goal of the diet was to promote consumption of 8-10 servings of vegetables and fruits daily. A food-based nutritional cancer prevention strategy, compared to a single-nutrient intervention study, allows for the additive effect of multiple protective dietary factors and potential synergy of biological interactions that may further enhance protective effects. Although this study did not measure outcomes of disease regression, it set the stage for future studies evaluating dietary intervention and the reduction of cervical cancer.
Another study assessed dietary risk factors for women with invasive and in situ cervical carcinoma in Bangkok, Thailand. (37) Alter administering a food-frequency questionnaire, 50 in situ cases were compared to 125 controls, while a separate group of 134 invasive cases were compared to 384 controls. The study demonstrated that by increasing intake of foods rich in vitamin A, particularly high retinol foods, there may be a reduced risk of in situ disease, and at highest level of intake may inhibit progression to invasive disease. No significant associations were noted among high vitamin C-, folate-, vitamin E-, or beta carotene-foods, or cruciferous vegetables with regard to risk of either in situ or invasive cervical cancer. Currently underway is a randomized trial of 326 women with biopsy proven CIN II to determine if a change in dietary pattern can promote regression of cervical dysplasia. The primary locus of the dietary change is on carotenoids.
Vitamin A
All-trans retinoic acid and 9-cis retinoic acid are metabolites of vitamin A (retinol) in vivo. Interest in retinoic acid as a chemopreventive agent stems from laboratory research that indicates retinoids are potent modulators of epithelial cell growth and differentiation. (38) Additionally, epidemiological studies report retinol intake and serum retinol levels have been found to be 4.5-times lower among women with cervical dysplasia who progress to in situ or invasive disease when compared to those whose disease regresses. (39)
Because of the known teratogenic side effects of high-dose vitamin A, there is limited application of retinoic acid for women of reproductive age. To avoid such a problem, a local topical method of delivery to the cervix was designed. Topical application of all-trans-retinoic acid has been shown to enhance the regression of CIN II in randomized clinical trials. (40) A total of 301 women with histologically confirmed CIN II and III were randomized to treatment groups to receive either 1 mL 0.375-percent retinoic acid or placebo cream for four consecutive days with follow-up and maintenance treatment for two days at months 3 and 6. Cytology and colposcopy were assessed at 9, 12, 15, 21, and 27 months after initial application. The primary histological evaluation was assessed at 15 months. Regression of CIN II lesions occurred in 27 percent of the placebo group and 43 percent of the retinoic acid group. No effect on CIN III lesions was observed.
Since the conclusion of this phase III study, several independent laboratory research endeavors have evaluated retinoic acid as a chemopreventive agent. Studies have shown that retinoic acid is able to regulate differentiation of normal human cetocervical epithelial cells, (41) induce reversible growth inhibition, down-regulate HPV-18 and c-myc mRNA, (42) inhibit immortalization of HPV-16 transfected human keratinocytes, and at physiologic concentrations inhibit expression of HPV-E6 and -E7 proteins. (43) These laboratory findings support clinical evidence that retinoic acid is active in preventing cervical cancer and warrants further clinical trials.
Carotenoids
Although extensive evidence exists for the role of fruits and vegetables in lowering risk of human cancers, the association of carotenoids and cancer is considerably less clear. Carotenoids are obtained from fruits and vegetables, fortified foods, and nutritional supplements. Many experimental studies support a cancer preventive role for these compounds. (44) However, in randomized clinical trials of beta carotene, either no effect (45) or increased cancer incidence among high risk subjects (46,47) has been observed. To date, the vast majority of research has focused on beta carotene and epithelial cell cancers; whereas, relatively few studies have investigated the association of other carotenoids with cancer.
Studies of cervical dysplasia and carotenoids indicate low concentrations of selected serum carotenoids (alpha carotene, beta carotene, lycopene, zeaxanthin, and beta cryptoxanthin) are associated with an increased risk of CIN. (48-51) In a recent study of 241 southwestern American Indian women, 81 with diagnosed CIN II/III were compared to 160 women with normal cervical epithelium. After adjusting for confounding factors, there appeared to be a significant association between decreasing serum carotenoid concentrations and increased risk of GIN, (52) particularly the carotenoids beta cryptoxanthin, lutein, and zeaxanthin.
Although many studies suggest an association between decreased plasma beta carotene and risk for cervical dysplasias, (53) clinical trials examining the efficacy of beta carotene supplementation do not demonstrate a positive effect. In a randomized, nine-month clinical trial of biopsy confirmed dysplasia in 69 women, 39 received 30 mg beta carotene while 30 were given a lactose placebo. (54) Colposcopy and biopsy were performed at baseline and at nine months. Complete regression of disease occurred in 23.1 percent of the carotene group, while there was 46.7-percent complete regression in the placebo group. Partial regression occurred in 23.1 percent of the carotene group, while there was partial regression in only 3.3 percent of the placebo group. Only one case in each group progressed to cervical cancer. Study participants in the placebo and carotene groups were similar in all regards except for the baseline grade of histopathology. Seventy percent of the placebo group had a lesion that was less than CIN II compared with 35.9 percent of the intervention group. Similar negative results have been reported in other clinical trials using 30 mg beta carotene (55,56) as well as studies using a 10 mg dose. (57)
Indole-3-Carbinol
Indole-3-carbinol (I3C) is a phytochemical present in all members of the cruciferous vegetable family including cabbage, broccoli, Brussels sprouts, cauliflower, and kale. Recent studies indicate I3C has the potential to prevent and even treat a number of common cancers, especially those that are estrogen related. (58) Indole-3-carbinol is rapidly converted in the stomach to a variety of condensation products, including diindolylmethane (DIM), indolylcarbazole (ICZ), and 2-(indol-3-ylmethyl)-3,3'-diindolymethane (L-Tr-1) (Figure 2). (59) Plasma from humans and rats fed I3C contains no detectable 13C, but rather large amounts of DIM and other metabolites. (60) Thus, metabolic products of I3C are probably the major compounds initially available to cells after ingestion of I3C. However, laboratory studies suggest I3C can act in several different ways to prevent transformation and/or tumor progression, as well as to kill transformed cells selectively.
[FIGURE 2 OMITTED]
Indole-3-carbinol, through its action on cytochrome P-450, is known to alter the pathway of estrogen metabolism in human males and females in a manner that decreases the risk of certain tumors. (61-63) Metabolism is altered by inducing specific cytochrome P-450 isoforms, via the aryl hydrocarbon receptor, (64) for which DIM is a weak ligand. (65) Metabolic degradation of estradiol by liver cells results primarily in either 2hydroxyestrone or 16[alpha]-hydroxyestrone, and to a lesser extent 4-hydroxyestrone, a potent carcinogen. It is known that 16[alpha]-hydroxyestrone causes proliferation of some breast tumor cell lines, (66) while the alternative metabolite, 2hydroxyestrone, has antiestrogenic and antiproliferative activity. (67) Women with CIN II/ III have lower 2-hydroxyestrone/16[alpha]-hydroxyestrone ratios than women with no abnormal cervical pathology; (68) therefore, the goal is to up-regulate 2-hydroxylation.
While tumor-associated viruses can profoundly affect the 2-hydoxyestrone/16[alpha]-hydroxyestrone ratio, attempts to directly decrease 16[alpha]-hydroxylation have not proved to be effective. However, by up-regulating 2-hydroxylation, estradiol is metabolized to a benign product at the expense of 16[alpha]-hydroxylation. Several compounds have proven to be effective in up-regulating 2-hydroxylation; Niwa et al found I3C to be the most potent. (69) Indole-3-carbinol also appears to suppress 4-hydroxylation activity. (70)
In a double-blind, placebo controlled study, 30 patients with biopsy-confirmed CIN II-III were randomized to receive placebo or 200 or 400 mg oral I3C daily for 12 weeks. (71) Three patients did not complete the study. None of the 10 patients in the placebo group had complete regression of CIN. In contrast, four of eight patients in the 200-mg/day group and four of nine in the 400-mg/day group had complete regression of CIN based on 12-week biopsy. In this study, the highest dose, 400 mg/day, is equivalent to one-third of a head of cabbage. No adverse effects were noted in this or previous studies.
An in vitro study of I3C was performed on human cervical cancer cell lines to determine if I3C and DIM could induce apoptosis. (72) This study concluded both I3C and DIM are able to achieve apoptosis in the cervical epithelium of HPV-16 transgenic mice, suggesting its use as a potential chemotherapeutic agent.
Folate and Homocysteine
Folate deficiency was linked with cervical dysplasia as early as 1966. (73) It has been hypothesized that subclinical folate deficiency, even if transient or localized, allows for incorporation of the HPV genome into host DNA with resultant malignant transformations. (74) The strongest association has been observed between low red blood cell (RBC) folate and HPV-16. However, there is strong evidence that current oral contraceptive use may constitute an independent risk, even with acceptable folate levels. (75)
Whitehead et al demonstrated megaloblastic changes in cervical smears of oral contraceptive users in the absence of general folate deficiency. (76) Oral folate therapy for two weeks led to improvement in cervical cytology despite "normal" blood folate. It has also been reported that taking oral contraceptives leads to increased serum copper (77) and decreased serum folate by interference with intestinal conjugase (an enzyme required for transmembranous folate transport), subsequently leading to elevated homocysteine levels. (78)
Folate metabolism is closely linked with the methylation cycle and DNA biosynthesis, which requires the insertion by 5-formyltetrahydrofolate (folinic acid) and 5,10-methylenetetrahydrofolate, of one-carbon groups into the purine ring and pyrimidine bases. The active folate moiety, 5-methyltetrahydrofolate donates a one-carbon group for remethylation of homocysteine to methionine and subsequent methylation of DNA by S-adenosyl methionine. Thus, folate deficiency not only increases homocysteine concentrations within the cell, it also impairs DNA biosynthesis, (79) which is crucial to cell growth, reproduction, and differentiation. Consequently, low tissue folate causes an increase in the frequency of fragile sites on DNA, (80) the risk of DNA for attack by carcinogens and viruses, (81) and the potential for chromosomal damage and oncogene expression, (82,83) and inhibits DNA repair. (80)
The degree of hypomethylation of cervical tissue was observed in a series of biopsy samples from 41 women. (84) A significant degree of DNA methylation was present in low-grade CIN, while there was a significant decrease in DNA methylation in the cases of high-grade CIN and carcinoma. Additionally, an in vitro study demonstrated methylation selectively down-regulates HPV-18 transcription. (85)
Despite positive laboratory findings supporting a role for folic acid in the cervical cancer continuum, clinical trials have not demonstrated positive results with supplementation. In a trial by Butterworth et al, 235 subjects with CIN I or II were randomly assigned to receive either 10 mg folic acid or placebo (10 mg ascorbic acid) daily for six months. (86) After six months, there was no difference between cases or controls with regard to dysplasia status, biopsy results, or HPV-16 infection. The same author published a case-control study of 726 women in The Journal of the American Medical Association the same year. This study revealed low red blood cell folate levels, below 660 nmol/L, enhance the effects of several risk factors for cervical dysplasia, but particularly HPV-16 infection. (74)
Childers et al also conducted a phase III trial to determine whether high-dose folic acid improves regression of early stage CIN. The effects of treatment with 5 mg folic acid daily or placebo for six months were compared in 331 randomized women. (81) Patient HPV status was not determined. Similarly, this study did not demonstrate significant improvement for the treatment group compared to controls. After three months of treatment, 8.1 percent of the folate intervention group had lesions that improved while only 2.8 percent of the placebo had improvements. However, after six months of follow-up, seven percent of the folate group and six percent of the placebo group showed improvements. Both the Childers and Butterworth trials had a high number of patients with CIN I, a lesion with a high spontaneous regression rate and low rate of progression. It remains unclear if folic acid supplementation would be more effective in preventing progression of moderate and severe dysplasia. Although no research has been conducted to support this theory, it is possible some cases of dysplasia may be a result of inability to properly convert folic acid to one of its more active forms, such as folinic acid or 5-methyltetrahydrofolate. More research is required to determine whether supplementation with one of these forms would provide more benefit in the prevention or treatment of dysplasia.
Antioxidants
Low plasma levels of antioxidants have consistently been linked to increased incidence of cancer and precancerous states. (87,88) Studies have measured the association between various plasma and tissue antioxidant levels and severity of CIN and cervical cancer. In one study, plasma levels of total coenzyme Q10 (CoQ10) and alpha tocopherol were measured by high performance liquid chromatography in patients with biopsy-confirmed CIN (n=55), cervical cancer (n=20), and in controls with normal PAP smears (n=27). Results showed mean plasma levels of CoQ10 and alpha tocopherol were significantly lower in patients with diagnosed CIN and cervical cancer when compared to controls. Levels of CoQ10 from cervicovaginal epithelial cells were measurable and also appeared to be significantly lower in women diagnosed with CIN. (89) These findings suggest low levels of these two antioxidants may play a role in the pathogenesis of cervical cancer. On the other hand, low plasma levels may also reflect increased utilization of antioxidants to counteract oxidative stress, suggesting the body needs supplementation to continue this process efficiently.
Plasma ascorbic acid (AA) levels in smokers are lower in both normal women (90) and women with cervical dysplasias. (91) Sixty-two women with abnormal PAP smears underwent colposcopy and biopsy as well as cervicovaginal lavage to collect exfoliated epithelial cells. (92) Measurements of AA and glutathione (GSH) were evaluated and measured by standardized methods. The study demonstrated that the total number of cells retrieved in lavage specimens of smokers is significantly higher compared to the nonsmoker group, suggesting rapid exfoliation of epithelial cells may be a factor in the pathogenesis of dysplasias. However, AA and GSH levels were not statistically significant among the various groups of women with histopathologically diagnosed cervical dysplasia. The small sample size in each dysplasia group may account for this finding.
Although the role of selenium and cervical cancer has not been studied extensively, studies have found no relationship between serum selenium and invasive cervical cancer. (93,94) To date no studies, either clinically or in vitro, have been performed to assess selenium status in women with precancerous or dysplastic states.
Escharotic Treatment
The use of escharotic or caustic treatments for epithelial cancers is based on a centuries-old observation that select plant and mineral extracts could be used to treat topical skin lesions. Zinc chloride (ZnCl), and Sanguinaria canadensis (bloodroot) are the two agents traditionally used as part of the Mohs chemosurgery fixed-tissue technique. (95) ZnCl was used as a fixative while bloodroot was used as an organic stabilizer. The paste application, fixation, and excision of the tumor were repeated daily until microscopic examination finding was negative for any tumor. (96)
A small study using local escharotic treatment was conducted on seven women with carcinoma in situ of the cervix. (97) Three levels of treatment were employed: local treatment to the cervix, systemic treatment, and constitutional treatment. Local escharotic treatment utilized preparations of ZnCl, bloodroot, bromelain, and Calendula succus. Local treatment was repeated twice weekly for five weeks with treatments 2-3 days apart. Topical vitamin A was applied following each local treatment. Systemic treatment was comprised of ascorbic acid 6-10 g per day, beta carotene 120,000-180,000 IU per day, and selenium 400 meg per day. Patients were also prescribed a vegan diet to eliminate animal fats and two botanical compounds to enhance immune function--Taraxacum officinalis and Arctium lappa. Systemic treatment was continued for not less than three months. Constitutional treatment consisted of a homeopathic remedy prescribed on an individual basis.
All seven patients received one year of follow-up. Four of the women remained disease free after the one-year period. One woman improved to atypia and then reverted to mild dysplasia. One woman had resolution of the cells of the endocervix and not the ectocervix, and one woman had resolution of the cells of the ectocervix and not the endocervix. The latter patients appeared to be non-compliant with regard to diet and lifestyle changes, suggesting the influence of synergistic effects of this multi-modality approach.
A follow-up study was performed by the same group on 43 cases, including cervical atypia (n=7), cervical dysplasia (n=26), and carcinoma in situ (n=10) during the following two years. (98) A similar protocol was used, with the addition of 10 mg folic acid daily. The results of the study were encouraging as 38 of the women had complete regression to normal, while three of the women had partial regression and two had persistent lesions. The two women with persistent lesions had low-grade dysplasia. These studies yield promising results, suggesting the need for a multi-faceted approach to preventing cervical cancer. Table 3 summarizes the escharotic treatment.
HPV Vaccine
Most recently, the HPV vaccine has been introduced to the conventional medical community as a means to prevent cervical cancer. The vaccine has been touted as "the beginning of the end for cervical cancer." (99) Vaccines against HPV, both the strains commonly associated with cervical cancer and those associated with genital warts, are a priority for a number of pharmaceutical and biotechnology firms. In recent years, two companies, Cantab of Cambridge, England and MedImmune of Gaithersburg, Maryland, USA, have conducted human trials of these vaccines. Merck has also produced a vaccine that has been tested successfully in double-blind trials.
Cantab has created TA-HPV, a live recombinant vaccinia virus engineered to express the E6 and E7 genes from HPV type-16 and -18. the principle viruses associated with cervical cancer. (100) MedImmune's prophylactic vaccine is called MEDI-501, which consists of recombinant HPV-11 LI protein. Recombinant LI has the property to self-assemble into virus-like particles (VLPs). VLPs contain no viral DNA and are considered noninfectious. Merck has created the naked plasmid DNA vaccine, which appears to be more cost effective and has the ability to be processed intracellularly, resulting in a more potent cellular immune response. (101)
In November 2002, The New England Journal of Medicine reported on a randomized, multicenter, double-blind study of 2,392 young women, ages 16-23 years, who received three doses of placebo or HPV-16 virus-like particle vaccine (40 [micro]]g per dose), given at day 0, month 2, and month 6. This study was fully funded by Merck. The women were followed a median of 17.4 months. Only 1,533 women were eligible for primary analysis. Forty-one cases of persistent HPV-16 infection occurred in the placebo group and none in the vaccine group. Forty-four cases of preinvasive cervical neoplasia not associated with HPV-16 infection were identified, 22 in each group. (102) A major limitation to this study is that primary analysis was limited to women who were negative for HPV-16 DNA and HPV-16 antibodies both at enrollment and at month 7, suggesting HPV-16 can potentially develop during the course of vaccination, but results were excluded in final assessment.
Although the vaccine was generally well tolerated, a slightly higher percentage of women in the vaccine group than in the placebo group failed to complete the vaccination series or withdrew shortly thereafter, suggesting the vaccine may have been associated with reduced tolerability. The most common side effect reported was pain at the sight of injection, experienced by both placebo and vaccinated groups. Systemic events were reported by 41.6 percent of the vaccinated group and 43.5 percent of the placebo group. The term systemic event was not defined. Serious adverse effects were reported in the vaccine and placebo group, 0.4 and 0.3 percent, respectively, causing discontinuation of the study.
Discussion
Despite potential progress in the medical community, a number of challenges to widespread use of the HPV vaccine can be anticipated. Public health officials will need to address the considerable social implications for what amounts to be an "STD vaccine." Vaccination would begin in early adolescence, making it necessary for parents and doctors to discuss sex with children. In Journal Watch Women's Health, from the publishers of The New England Journal of Medicine, Dr. Andrew Kaunitz brings to light a few important questions: (1) In the United States, where the federal government supports universal vaccination of children, will there be political obstacles to funding a vaccine that makes sex safer? (2) Given that the main beneficiaries of an HPV vaccine will be women, will parents of teenage boys balk at having their sons vaccinated? and (3) In less developed countries where invasive cervical cancer is most prevalent, will cost considerations and the need for three injections limit vaccine use? (103) The vaccine is projected to cost $100 per dose. With three doses of the vaccine required to confer HPV immunity, the cost may be prohibitive in poor nations where cervical cancer kills an estimated 250,000 women a year.
Although numerous epidemiological studies have examined the association between risk of cervical cancer and dietary cofactors, most studies appear to have methodological limitations. A major limitation of many observational studies is reliance on dietary self-report, which has many potential sources of error and bias. Also, many nutritional epidemiological studies were conducted before a reliable test for HPV status was available. (104)
As with many nutritional-based clinical trials, nutrient-based cervical cancer prevention trials have been designed without adequate information or qualitative analysis as to when in the carcinogenesis continuum a particular nutrient is actively effective. Additionally, little light has been shed on the duration of treatment and length of follow-up needed to demonstrate an effect. Current evidence suggests nutritional factors play a role in the progression of normal cervical epithelium to preinvasive cervical lesions and ultimately carcinoma. However, lack of knowledge of biological mechanisms, which determines optimal timing for intervention, is lacking. This ultimately deters the ability to test the effect of a nutrient appropriately in clinical trials. To date, only five phase III nutrient chemoprevention trials have been completed, with only one showing positive effect. Until more intervention studies have been completed, it is reasonable to assume nutrient supplementation may be an effective tool in preventing progression of cervical dysplasia to cervical cancer, especially when serum and plasma markers unequivocally demonstrate specific nutrient deficiencies. More importantly, adequate dosage and duration of treatment need to be further evaluated.
References
(1.) Greenlee RT, Hill-Harmon MB, Murray T, Thun M. Cancer statistics, 2001. CA Cancer J Clin 2001;51 : 15-36.
(2.) Surveillance, Epidemiology, and End Results (SEER) Program Public-Use Data (1973-1998). National Cancer Institute, Division of Cancer Control and Population Sciences, Bethesda, MD, Surveillance Research Program. Cancer Statistics Branch, 2001.
(3.) Franco EL. Understanding the epidemiology of genital infection with oncogenic and nononcogenic human papillomaviruses: a promising lead for primary prevention of cervical cancer. Cancer Epidemiol Biomarkers Prey 1997;6:759-761.
(4.) Mitchell ME Tortolero-Luna G, Wright T, et al. Cervical human papillomavirus infection and intraepithelial neoplasia: a review. J Natl Cancer Inst Monogr 1996;21:17-25.
(5.) Kurman R J, Henson DE, Herbst AL, et al. Interim guidelines for management of abnormal cervical cytology. The 1992 National Cancer Institute Workshop. JAMA 1994;271:1866-1869.
(6.) Landis SH, Murray T, Bolden S, Wingo E Cancer statistics, 1998. CA Cancer J Clin 1998;48:6-29.
(7.) Koutsky LA, Holmes KK, Critchlow CW, et al. A cohort study of the risk of cervical intraepithelial neoplasia grade 2 or 3 in relation to papillomavirus infection. N Engl J Med 1992;327:1272-1278.
(8.) Schiffman MH, Bauer HM, Hoover RN, et al. Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst 1993;85:958-964.
(9.) Tabrizi SN, Fairley CK, Chen S, et al. Epidemiological characteristics of women with high grade CIN who do and do not have human papillomavirus. Br J Obstet Gynaecol 1999;106:252-257.
(10.) No authors listed. Risk of cervical dysplasia in users of oral contraceptives, intrauterine devices or depot-medroxyprogesterone acetate. The New Zealand Contraception and Health Study Group. Contraception 1994;50:431-441.
(11.) Ho GY, Kadish AS, Burk RD. et al. HPV 16 and cigarette smoking as risk factors for high-grade cervical intra-epithelial neoplasia. Int J Cancer 1998;78:281-285.
(12.) Palefsky JM, Holly EA. Molecular virology and epidemiology of human papillomavirus and cervical cancer. Cancer Epidemiol Biomarkers Prev 1995;4:415-428.
(13.) Munoz N, Bosch FX. Epidemiology of cervical cancer. IARC Sci Publ 1989;94:9-39.
(14.) deVet HC, Knipschild PG, Sturmans E The role of sexual factors in the aetiology of cervical dysplasia, Int J Epidemiol 1993:22:798-803.
(15.) Chen YH, Huang LH, Chen TM. Differential effects of progestins and estrogens on long control regions of human papillomavirus types 16 and 18. Biochem Biophys Res Commun 1996;224:651-659.
(16.) Yuan F. Auborn K, James C. Altered growth and viral gene expression in human papillomavirus type 16-containing cancer cell lines treated with progesterone. Cancer Invest 1999;17:19-29.
(17.) Autier R Coibion M, Huet E Grivegnee AR. Transformation zone location and intraepithelial neoplasia of the cervix uteri. Br J Cancer 1996:74:488-490.
(18.) Auborn KJ, Woodworth C, DiPaolo JA, Bradlow HL. The interaction between HPV infection and estrogen metabolism in cervical carcinogenesis. Int J Cancer 1991;49:867-869.
(19.) Rando RF, Lindheim S, Hasty L, et al. Increased frequency of detection of human papillomavirus deoxyribonucleic acid in exfoliated cervical cells during pregnancy. Am J Obstet Gynecol 1989;161:50-55.
(20.) Condyloma acuminatum-US 1966-1981. MMWR 1983;32:306-308.
(21.) Syrjanen K, Hakama M, Saarikoski S, et al. Prevalence, incidence, and estimated life-time risk of cervical human papillomavirus infections in a nonselected Finnish female population. Sex Transm Dis 1990;17:15-19.
(22.) Rock CL, Michael CW, Reynolds RK, Ruffin MT. Prevention of cervix cancer. Crit Rev Oncol Hematol 2000;33:169-185.
(23.) Kiviat NB, Koutsky LA. Specific human papillomavirus types as the casual agents of most cervical intraepithelial neoplasia: implications for current views and treatments. J Natl Cancer Inst 1993;85:934-935.
(24.) Miller AB, Barclay TH, Choi NW, et al. A study of cancer, parity and age at first pregnancy. J Chron Dis 1980;33:595-605.
(25.) Peters RK, Thomas D, Hagen DG, et al. Risk factors tot invasive cervical cancer among Latinas and non-Latinas in Los Angeles County. J Natl Cancer Inst 1986;77:1063-1077.
(26.) Wright VC, Riopelle MA. Age at time of first intercourse v. chronologic age as a basis for Pap smear screening. Can Med Assoc J 1982;127:127-131.
(27.) Arora CD, Schmidt DS, Rader AE, et al. Adolescents with ASCUS: are they a high risk group? Clin Pediatr 2001;40:133-138.
(28.) Herrero R, Potischman N, Brinton LA, et al. A case-control study of nutrient status and invasive cervical cancer. 1. Dietary indicators. Ant J Epidemiol 1991:134:1335-1346.
(29.) Roye CF. Pap smear screening for adolescents: rationale, technique and follow-up. J Pediatr Health Care 1993;7:199-206.
(30.) Massad LS, Anoina D. Colposcopic and cytologic findings among adolescents referred to two urban teaching hospitals. J Pediatr Adolesc Gynecol 1996:9:190-194.
(31.) deVet HC, Sturmans F, Knipschild PG. The role of cigarette smoking in the etiology of cervical dysplasia. Epidemiology 1994;5:631-633.
(32.) Ziegler RG. Vegetables, fruits, carotenoids and the risk of cancer. Am J Clin Nutr 1991;53:251S-259S.
(33.) Byers T, Perry G. Dietary carotenes, vitamin C, and vitamin E as protective antioxidants in human cancers. Annu Rev Nutr 1992;12:139-159.
(34.) Block G, Patterson B, Subar A. Fruit. vegetables and cancer prevention: a review of the epidemiological evidence. Nutr Cancer 1992;18:1-29.
(35.) Steinmetz KA, Potter JD. Vegetables, fruit, and cancer prevention: a review. J Am Diet Assoc 1996;96:1027-1039.
(36.) Rock CL, Moskowitz A, Huizar B, et al. High vegetable and fruit diet intervention in premenopausal women with cervical intraepithelial neoplasia. J Am Diet Assoc 2001;101:1167-1174.
(37.) Shannon J, Thomas DB, Ray RM, et al. Dietary risk factors for invasive and in-situ cervical carcinomas in Bangkok, Thailand. Cancer Causes Control 2002:13:691-699.
(38.) Sporn MB, Roberts AB. Cervical dysplasia regression induced by all-trans-retinoic acid. J Natl Cancer Inst 1994;86:476-477.
(39.) Nagata C, Shimizu H, Higashiiwai H, et al. Serum retinol level and risk of subsequent cervical cancer in cases with cervical dysplasia. Cancer Invest 1999;17:253-258.
(40.) Meyskens FL Jr, Surwit E, Moon TE, et al. Enhancement of regression of cervical intraepithelial neoplasia II (moderate dysplasia) with topically applied all-trans-retinoic acid: a randomized trial. J Natl Cancer Inst 1994;86:539-543.
(41.) Agarwal C, Rorke EA, Irwin JC, Eckert RL. Immortalization by human papillomavirus type 16 alters retinoid regulation of human ectocervical epithelial cell differentiation. Cancer Res 1991;51:3982-3989,
(42.) Bartsch D, Boye B, Baust C, et al. Retinoic acid-mediated repression of human papillomavirus 18 transcription and different ligand regulation of the retinoic acid receptor beta gene in non-tumorigenic and tumorigenic HeLa hybrid cells. EMBO J 1992:11:2283-2291.
(43.) Khan MA, Jenkins GR, Tolleson WH, et al. Retinoic acid inhibition of human papillomavirus type 16-mediated transformation of human keratinocytes. Cancer Res 1993;53:905-909.
(44.) Steinmetz KA, Potter JD. Vegetables, fruit and cancer II. Mechanisms. Cancer Causes Control 1991;2:427-442.
(45.) Hennekens CH, Buring JE, Manson JE, et al. Lack of effect of long-term supplementation with beta carotene on the incidence of malignant neoplasms and cardiovascular disease. N Engl J Med 1996;344:1145-1149.
(46.) Albanes D, Heinonen OR Huttunen JK, et al. Effects of alpha-tocopherol and beta-carotene supplements on cancer incidence in the Alpha-Tocopherol Beta-Carotene Cancer Prevention Study. Am J Clin Nutr 1995;62:1427S-1430S.
(47.) Omenn GS, Goodman GE, Thornquist MD, et al. Risk factors for lung cancer and for intervention effects in CARET, the Beta-Carotene and Retinol Efficacy Trial. J Natl Cancer Inst 1996;88:1550-1559.
(48.) Potischman N, Herrero R, Brinton LA, et al. A case-control study of nutrient status and invasive cervical cancer. II. Serologic indicators. Am J Epidemiol 1991;134:1347-1355.
(49.) Nagata C, Shimizu H, Yoshikawa H, et al. Serum carotenoids and vitamins and risk of cervical dysplasia from a case-control study in Japan. Br J Cancer 1999;81:1234-1237.
(50.) Peng YM, Peng YS, Childers JM, et al. Concentrations of carotenoids, tocopherols, and retinol in paired plasma and cervical tissue of patients with cervical cancer, precancer, and non-cancerous diseases. Cancer Epidemiol Biomarkers Prey 1998;7:347-350.
(51.) VanEenwyk J, Davis FG, Bowen PE. Dietary and serum carotenoids and cervical intraepithelial neoplasia. Int J Cancer 1991;48:34-38.
(52.) Schiff M, Becker TM, Masuk M, et al. Risk factors for cervical intraepithelial neoplasia in Southwestern American Indian women. Am .l Epidemiol 2000;152:716-726.
(53.) Palan PR, Mikhail MS, Goldberg GL, et al. Plasma levels of beta-carotene, lycopene, canthaxanthin, retinol, and alpha- and tau-tocopherol in cervical intraepithelial neoplasia and cancer. Clin Cancer Res 1996;2:181-185.
(54.) Romney SL, Ho GY, Palan PR, et al. Effects of beta carotene and other factors on outcome of cervical dysplasia and human papillomavirus infection. Gynecol Oncol 1997;65:483-492.
(55.) Keefe KA, Schell MJ, Brewer C, et al. A randomized, double blind, Phase III trial using oral beta-carotene supplementation for women with high-grade cervical intraepithelial neoplasia. Cancer Epidemiol Biomarkers Prey 2001:10:1029-1035.
(56.) Mackerras D, Irwig L, Simpson JM, et al. Randomized double-blind trial of beta-carotene and vitamin C in women with minor cervical abnormalities. Br J Cancer 1999:79:1448-1453.
(57.) de Vet HC, Knipschild PG, Willebrand D, et al. The effect of beta-carotene on the regression and progression of cervical dysplasia: a clinical experiment. J Clin Epidemiol 1991;44:273-283.
(58.) Grubbs CJ, Steele VE, Casebolt T, et al. Chemoprevention of chemically-induced mammary carcinogenesis by indole-3-carbinol. Anticancer Res 1995;15:709-716.
(59.) Grose KR, Bjeldanes LF. Oligomerization of indole-3-carbinol in aqueous acid. Chem Res Toxicol 1992;5:188-193.
(60.) Stresser DM, Williams DE, Griffen DA, Bailey GS. Mechanisms of tumor modulation by indole-3-carbinol. Disposition and excretion in male Fischer 344 rats. Drug Metab Dispos 1995:23:966-975.
(61.) Telang NT, Suto A, Wong GY, et al. Induction by estrogen metabolite 16 alpha-hydroxyestrone of genotoxic damage and aberrant proliferation in mouse mammary epithelial cells. J Nail Cancer Inst 1992;84:634-638.
(62.) Stoewsand GS, Anderson JL, Munson L. Protective effect of dietary brussels sprouts against mammary carcinogenesis in Sprague-Dawley rats. Cancer Lett 1988;39:199-207.
(63.) Zeligs MA. Diet and estrogen status: the cruciferous connection. J Med Food 1998;1:67-81.
(64.) Auborn K J, Woodworth C, DiPaolo JA, Bradlow HL. The interaction between HPV infection and estrogen metabolism in cervical carcinogenesis. Int J Cancer 1991;49:867-869.
(65.) Chen I, McDougal A, Wang E Safe S. Aryl hydrocarbon receptor-mediated antiestrogenic and antitumorigenic activity of diindolylmethane. Carcinogenesis 1998;19:1631-1639.
(66.) Schneider J, Huh MM, Bradlow HL, Fishman J. Antiestrogen action of 2-hydroxyestrone on MCF-7 human breast cancer cells. J Biol Chem 1984:259:4840-4845.
(67.) Suto A, Bradlow HL, Wong GY, et al. Experimental down-regulation of intermediate biomarkers of carcinogenesis in mouse mammary epithelial cells. Breast Cancer Res Treat 1993;27:193-202.
(68.) Newfield L, Goldsmith A, Bradlow HL. Auborn K. Estrogen metabolism and human papillomavirus-induced tumors of the larynx: chemo-prophylaxis with indole-3-carbinol. Anticancer Res 1993;13:337-341.
(69.) Niwa T, Swaneck G, Bradlow HL. Alterations in estradiol metabolism in MCF-7 cells induced by treatment with indole-3-carbinol and related compounds. Steroids 1994;59:523-527.
(70.) Bradlow HL, Sepkovic DW, Telang NT. Osborne MP. Indole-3-carbinol. A novel approach to breast cancer prevention. Ann N Y Acad Sci 1995;768:180-200.
(71.) Bell MC, Crowley-Nowick P, Bradlow HL, et al. Placebo-controlled trial of indole-3-carbinol in the treatment of CIN. Gynecol Oncol 2000;78:123-129.
(72.) Chen DZ, Qi M, Auborn KJ, Carter TH. Indole 3-carbinol and diindolylmethane induce apoptosis of human cervical cancer cells and in murine HPV 16-transgenic preneoplastic cervical epithelium. J Nutr 2001;131:3294-3302.
(73.) Crews MG, Taper LJ, Ritchey SJ. Effects of oral contraceptive agents on copper and zinc balance in young women. Am J Clin Nutr 1980;33:1940-1945.
(74.) Butterworth CE Jr, Hatch KD, Macaluso M, et al. Folate deficiency and cervical dysplasia. JAMA 1992;267:528-533.
(75.) Butterworth CE Jr. Folic acid deficiency and cervical dysplasia: a potential preventable cancer risk. In: Bray G, ed. Vitamins and Cancer Prevention. Baton Rouge, LA: LSU Press; 1992.
(76.) Whitehead N, Reyner F, Lindenbaum J. Megaloblastic changes in the cervical epithelium: association with oral contraceptive therapy and reversal with folic acid. J Am Med Assoc 1973:226:1421-1424.
(77.) Butterworth CE Jr Effect of folate on cervical cancer. Synergism among risk factors. Ann N Y Acad Sci 1992;669:293-299.
(78.) van Duin M, Snijders PJ, Vossen MT, et al. Analysis of human papillomavirus type 16 E6 variants in relation to p53 codon 72 polymorphism genotypes in cervical carcinogenesis. J Gen Virol 2000;81:317-325.
(79.) Reidy JA, Chen AT. Folic acid and chromosome breakage. II. A methionine effect similar to that in fragile X expression. Hum Genet 1984;68:189-190.
(80.) Herbert V. The role of vitamin B12 and folate in carcinogenesis. Adv Exp Med Biol 1986;206:293-311.
(81.) Childers JM, Chu J, Voigt LF, et al. Chemoprevention of cervical cancer with folio acid: a phase III Southwest Oncology Group Intergroup study. Cancer" Epidemiol Biomarkers Prey 1995;4:155-159.
(82.) Adams RL. DNA methylation. The effect of minor bases on DNA-protein interactions. Biochem J 1990;265:309-320.
(83.) Hseih LL, Wainfan E, Hoshina S, et al. Altered expression of retrovirus-like sequences and cellular oncogenes in mice fed methyl-deficient diets. Cancer Res 1989;49:3795-3799.
(84.) Kim YI, Giuliano A, Hatch KD, et al. Global DNA hypomethylation increases progressively in cervical dysplasia and carcinoma. Cancer 1994;74:893-899.
(85.) Rosl E Arab A, Klevenz B, zur Hausen H. The effect of DNA methylation on gone regulation of human papillomaviruses. J Gen Virol 1993;74:791-801.
(86.) Butterworth CE Jr, Hatch KD, Soong SJ, et al. Oral folic acid supplementation lot cervical dysplasia: a clinical intervention trial. Am J Obstet Gynecol 1992;166:803-809.
(87.) Yeo AS, Schiff MA, Montoya G, et al. Serum micronutrients and cervical dysplasia in Southwestern American Indian women. Nutr Cancer 2000;38:141-150.
(88.) Palan PR, Mikhail MS, Basu J, Romney SL. Plasma levels of antioxidant beta-carotene and alpha-tocopherol in uterine cervix dysplasias and cancer. Nutr Cancer 1991;15:13-20.
(89.) Mikhail MS, Palan PR, Romney SL. Coenzyme Q0 and alpha tocopherol concentrations in cervical intraepithelial neoplasia and cervix cancer. Obstet Gynecol 2001;97:3S.
(90.) Basu J, Vermund SH, Mikhail M, et al. Plasma reduced and total ascorbic acid in healthy women: effects of smoking and oral contraception. Contraception 1989;39:85-93.
(91.) Basu J, Palan PR, Vermund SH, et al. Plasma ascorbic acid and beta-carotene levels in women evaluated for HPV infection, smoking and cervix dysplasia. 7th International Symposium on Prevention & Detection of Cancer. Nice, France: April 9-15, 1989.
(92.) Basu J, Mikhail MS, Goldberg GL, et al. Measurements of ascorbic acid and glutathione in exfoliated cervicovaginal epithelial cells of smokers and women with cervical dysplasias. Gynecol Obstet Invest 1990;30:48-51.
(93.) Sundstrom H, Yrjanheikki E, Kauppila A. Low serum selenium concentration in patients with cervical or endometrial cancer. Int J Gynaecol Obstet 1984;22:35-40.
(94.) Thompson FE, Patterson BH, Weinstein SJ, et al. Serum selenium and the risk of cervical cancer among women in the United States. Cancer Causes Control 2002;13:517-526.
(95.) Mohs FE. Chemosurgery: microscopically controlled method of cancer excision. Arch Surg 1941;42:279-295.
(96.) Swanson NA. Mohs surgery. Technique, indications, applications, and the future. Arch Dermatol 1983;119:761-773.
(97.) Hudson TS. Consecutive case study research of carcinoma in situ of cervix employing local escharotic treatment combined with nutritional therapy. J Naturopathic Med 1991;2:6-10.
(98.) Hudson TS. Escharotic treatment for cervical dysplasia and carcinoma. J Naturopathic Med 1993;4:23.
(99.) Cram CR The beginning of the end for cervical cancer? N Engl J Med 2002;347:1703-1705.
(100.) Borysiewicz LK, Fiander A, Nimako M, et al. A recombinant vaccinia virus encoding human papillomavirus types 16 and 18, E6 and E7 proteins as immunotherapy for cervical cancer. Lancet 1996;347:1523-1527.
(101.) Donnelly JJ, Martinez D, Jansen KU, et al. Protection against papillomavirus with a polynucleotide vaccine. J Infect Dis 1996;173:314-320.
(102.) Koutsky LA, Ault KA, Wheeler CM, et al. A controlled trial of a human papillomavirus type 16 vaccine. N Engl J Med 2002;347:1645-1651.
(103.) Kaunitz AM. An HPV vaccine--at last. Journal Watch Women's Health 2003;108:1-2.
(104.) Giuliano AR, Gapstur S. Can cervical dysplasia and cancer be prevented with nutrients? Nutr Rev 1998;56:9-16.
Keri Marshall, MS, ND--1996 Master of Science Social and Preventive Medicine, State University of New York at Buffalo; 2001 graduate, National College of Naturopathic Medicine. Private practice, Sandpoint, idaho. Email: mackaynd@aol.com
COPYRIGHT 2003 Thorne Research Inc.
COPYRIGHT 2003 Gale Group