Objectives: This study was aimed at examining whether hypothermia is neuroprotective against permanent cerebral ischemia in rats.
Methods: A total of 32 male Sprague-Dawley rats were subjected to a middle cerebral artery occlusion. In the hypothermic group, rats (n=10) underwent selective brain hypothermia for 5 hours with the use of a novel surface coil with coolant circulating inside. In the control (n=13) and sham groups (n=9), the rats were maintained at normothermia. After a period of 168 hours ischemia, animals were killed to measure the infarction volume of the brain stained with hematoxylin-eosin.
Results: There were no significant differences in physiological parameters except for the temperature. The present style of hypothermia significantly reduced infarction volume in the cortex and caudoputamen.
Discussion: The present results endorse the neuroprotective effect of our method of hypothermia in permanent focal cerebral ischemia at an endpoint of 7 week under the following two conditions: (1) reduction of muscle and caudoputamen temperature to 29 and 31°C, respectively; (2) maintenance of the mean arterial blood pressure above 90 mmHg during hypothermia. [Neurol Res 2005; 27: 613-619]
Keywords: Hemodynamics; neuroprotection; permanent cerebral ischemia; selective brain hypothermia
INTRODUCTION
The validity of hypothermia in transient cerebral ischemia has been well established1. However, the efficacy of hypothermia against permanent focal cerebral ischemia still remains to be confirmed. This controversy might be partly caused by the deteriorating cardiopulmonary condition during and after hypothermia. Thus, we chose selective brain hypothermia (SBH) instead of whole body hypothermia, which is prone to cause systemic sequelae. A novel external cooling system, including the application of a surface coil placed on the rat's head, was developed by ourselves2. Using this cooling device, neuroprotective efficacy of SBH was demonstrated against 6-, 24- and 48-hour ischemia in the rat3-5. The temperature of the brain and the temporal muscle were precisely monitored and regulated to a determined level by adjusting the flow rate of the coolant in the tube. In the present study, we tried to examine the effects of our method of SBH in a prolonged 168-hour ischemia of the rat, with careful management of systemic conditions.
METHODS
Middle cerebral artery occlusion
A total of 32 male Sprague-Dawley (SD) rats (SLC, Hamamatsu, Shizuoka, Japan) were anesthetized under spontaneous breathing through a face mask with halothane (2%) and N^sub 2^O/O^sub 2^ (2:1) following an intraperitoneal injection of atropine sulfate (0.1 mg) and benzyl penicillin (3000 units). They were put on a heating pad, which was regulated by an attached rectal temperature probe (TK-43; Asahi Electronic Industry, Higashi Osaka, Osaka, Japan). Polyethylene catheters were cannulated into the right femoral artery and vein. The arterial catheter was connected to a blood pressure monitor (7754D system; Hewlett-Packard Company, Palo Alto, California, USA).
A soft temperature probe (PTC-201; Unique Medical, Tokyo, Japan) was introduced into the right temporal muscle 2 cm from the surface. Then the animals underwent a left proximal middle cerebral artery occlusion (MCAo) according to the method described elsewhere6. Briefly, a special clip (TS-93026; Unique Medical, Tokyo, Japan) was applied to the stem of the middle cerebral artery (M1) just proximal to the lenticulostriate arteries (LSA). Then the M1 just distal to the LSA was coagulated and cut in order to prevent recanalization. After the MCAo, the concentration of halothane was changed to 0.5%.
Animals were assigned into group A (n=10): subjected to both MCAo and SBH, group B (n=13): subjected to MCAo without SBH and group C (n=9): subjected to a sham operation of a dura mater incision without SBH.
Selective brain hypothermia
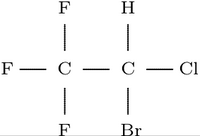
An icebox made of styrofoam filled with ice water was prepared. Cooled water was drawn from that box with the aid of an electromotive pump (STC-508; TERUMO, Tokyo, Japan) into an intervening tube and perfused within a coil placed around the head, then returned to the same box by way of another intervening tube. The coil is made of a silicone tubule, 2 mm in outside diameter, which had been rolled up and fixed with adhesives (Figure 1). The flow rate of the electromotive pump was adjusted as the muscle temperature fell to 29°C within 30 minutes after the ischemia and was re-adjusted to maintain the muscles at this level thereafter. If the temperature fell excessively or the mean arterial blood pressure (MABP) dropped, we turned off the flow for a while and turned on a light above the head if necessary. In the control and sham groups, the muscle temperature was kept at 36°C by the use of the same light.
Another 0.05 mg of atropine sulfate was administered intraperitoneally 3 hours later. A 0.1 ml of arterial blood sample was taken for gas analysis every hour. If necessary, a 7% sodium bicarbonate fluid or maintenance fluid (Sorita T3; Shimizu Pharmaceutical Co. Ltd., Shimizu, Shizuoka, Japan) was used for the correction of metabolic acidosis or hypovolemia, respectively. The second 3000 units of benzyl penicillin were injected intraperitoneally at the end of the anesthesia.
In group A, the flow rate of the pump was slowed at 3.5 hours after MCAo and the coil for SBH was removed at 4 hours of ischemia. A light was then turned on above the head until the muscle temperature rose to 32°C within 0.5 hour. In each group, after eliminating the probes and the catheters, all wounds were closed and the rat was liberated 5 hours following MCAo or sham operations into a cultivating cage. Every animal had free access to food and water under room temperature (25°C) until time of death. They received maintenance fluid subcutaneously as needed and 6000 units of benzyl penicillin every day. Body weight and a neurological score according to the criteria reported by Menzies et al. were recorded daily until death7. A transcardiac perfusion fixation with a phosphate buffer containing 10% formic aldehyde was performed under inhalation anesthesia at 168 hours after the procedure.
All of the above-mentioned experimental protocols were approved by the animal research committee at Saitama Medical Center/School.
Evaluation of tissue injury
The brain was cut into coronal sections at 1 mm intervals after paraffin embedding. Brain slices were stained with hematoxylin-eosin and scanned with a 36 bit, 1200 dots per inch scanner (ES2000; Epson, Tokyo, Japan). The scanned data were printed on paper. The brain slices were microscopically examined in a blinded evaluation (BH-2; Olympus, Tokyo, Japan). The boundaries of infarction were traced out on the printed matter according to the criteria of neuronal change described by Garcia et al.8. This traced material was rescanned and defined as the infarction map. Every component on this infarction map (hemisphere, caudoputamen and each infarction) was measured with the aid of NIH Image (version 1.62; National Institutes of Health, Bethesda, Maryland, USA). Each volume was calculated by multiplying each area by the slice thickness and integrating all the slices. The regional volume increase rate of the affected to non-affected side was defined as the edema ratio.
The results are presented as a mean value±standard deviation (SD). MABP and arterial blood gas (ABG) were analysed using two-way repeated-measures analysis of variance (ANOVA), and the infarction volume, edema ratio, neurological score, body weight and weight loss were analysed using one-way factorial ANOVA, Student's unpaired f-test and Mann-Whitney's Latest (Stat View; version 4.0; Abacus Concepts, Inc., Berkeley, California, USA). A value of p
RESULTS
All animals survived until the end of the experiment. There were no significant differences in ABG analyses (Table 1). Animals lost weight at a rate of 10 g/day; however, there was no significant difference between the corresponding groups in body weight or weight loss (Table 2). No significant differences in MABP were noted among the groups during the experiment. Regarding the rectal temperature, normothermic animals showed a constant temperature at 37°C. In the hypothermie group, the rectal temperature fell to 34°C within 15 minutes and remained there for 1.5 hours towards the end of the experiment and gradually returned to normothermia (Figure 2).
In each group, the muscle temperature was 35.5 C at the induction of the procedure. In the hypothermie group, it fell to 31°C within the first 15 minutes, and subsequently to 29°C within a further 15 minutes. It was then maintained at that level, correspondent with 31°C of the caudoputaminal temperature, for a further 3 hours. The temperature difference between the muscle and the rectum was 7°C, but this disparity did not cause any serious sequelae, such as convulsions or ventilatory failure. Re-warming was performed gradually at a rate of 3°C/hour until the muscle temperature rose up to 32°C, which is correspondent with 34°C of the caudoputaminal temperature. In the normothermic groups, the muscle temperature was unchanged throughout the anesthesia.
SBH significantly reduced hemispheric infarct volume (hypothermia: 38 ± 21 ; control: 102 ± 41; sham control: 2 ± 2 mm^sup 3^, mean ± SD, p
DISCUSSION
The importance of the systemic conditions
Since the methodology of the present study is designed for small animals, systemic parameters, such as MABP and ABG, easily deteriorate under several hours of general anesthesia even without hypothermia. We have already reported the efficacy of 6 hour SBH on the same MCAo model in 70 SD rats under artificial ventilation with endotracheal intubations and brain temperature probes using a stereotaxic frame until 48 hours post-MCAo2-5. In those studies, we used the same criteria as Garcia et al. at each time-point (6 hours; shrinkage and swelling of neuronal perikarya, 24 hours and later; red and ghost neurons8). However, some animals' MABP deteriorated to below 90 mmHg, and others' showed an elevation of the caudoputaminal temperature to more than 32 C before rewarming. In both cases, the hemispheric infarction volume reached levels of more than 100 mm^sup 3^. This implies the necessity of maintaining the MABP throughout SBH because the autoregulation of the cerebral blood flow (CBF) is disordered during hypothermia9. To maintain the MABP, correcting metabolic acidosis with sodium bicarbonate is essential. Moreover, we must pay attention not only to the lowered brain temperature, but also to the rate of the temperature decline, which falls to the temperature of venous blood. Simultaneously, the brain temperature needs to be maintained below 31°C, whereas in our system employing a surface coil, it is difficult to induce the caudoputaminal temperature below 30°C without a decline of the rectal temperature at the beginning because the circulating blood is around 37°C. Along this line of thought, we delayed use of a heating pad for an hour and left the rectal temperature decreasing to 34°C. This enabled the brain temperature to fall to the intended level without the venous blood returning to the heart below 30°C, and to prevent cardiac dysfunction. Subsequently, the heating pad was used to restore the rectal temperature to 36°C and the brain temperature was kept around 34°C.
Methodology
In this study, we tried to prohibit all conceivable trauma, such as endotracheal tube trouble, brain injury by temperature probe etc. to the animals, on a basis of results obtained from preceding studies (data not shown). In order to prevent airway complications after anesthesia, we carried out SBH under spontaneous breathing without endotracheal intubation. Ventilatory failure from the hypothermia was not manifested. The duration of 5 hours anesthesia allowed rapid recovery from the anesthesia and animals were exposed to room temperature. Thus, mild hypothermia might have been prolonged for a while after the anesthesia. We transiently used the brain temperature probe because unexpected body movements might have caused serious brain injury. Another reason for the temporary use of the brain temperature probe is that the muscle temperature correlated well with the caudoputaminal temperature at each time-point (contingency table, p
A novel external cooling device
Several methods of local cooling have been reported, but each of them has some drawbacks10-12. Thus, we have designed a newly devised cooling system employing a surface coil with coolant circulating inside. This maintained accurate control of the brain temperature with little risk of infection.
Review of the literature
So far, many experiments on hypothermia in transient cerebral ischemia have been performed, and their validity over 168 hours or more has been proven13-16. As yet, only a few have been carried out in hypothermia against permanent cerebral ischemia (Table 3). There are 13 positive results out of 15 experiments in ischemia of 24 hours or less17-31. However, only one study, using severe hypothermia, out of three experiments on 48-96-hour ischemia has demonstrated any efficacy32. The other two applied intentional hypotension or insufficient hypothermia33,34. Regarding long-term follow-up of a week or more, apart from our report there exists only one other observation, by Yanamoto et al.35. These authors kept the rectal temperature at 33°C for 2 hours and cultivated the animal in a cold room, but it was rewarmed to 35°C at 6 hours of ischemia. Although an analysis of infarction by triphenyltetrazolium chloride over a chronic period incurs many problems, the results suggest that long-lasting minimal hypothermia might be beneficial in a model of mild ischemia14. Finally, the most important issue is to maintain the cardiopulmonary condition close to the normal physiological range during hypothermia, even in experiments on small animals. These results merit further study to investigate the effect of hypothermia in large animals or primates.
CONCLUSION
To our knowledge, the present study has demonstrated, with histological confirmation, that post-ischemic transient hypothermia protects the brain up to 168 hours under the careful management of hemodynamics and respiration.
The above results suggest that the present style of hypothermia is a useful medical strategy for the treatment of patients with acute brain attack.
ACKNOWLEDGEMENT
This study was supported by a scientific grant from the Japanese Ministry of Education (09671444). Some of the results of this study were reported at the International Brain Hypothermia Symposium, Tokyo, Japan, February 2004.
REFERENCES
1 Busto R, Dietrich WD, Clobus MYT, et al. Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab 1987; 7: 729-738
2 Taniguchi T, Matsui T, Morimoto T, et al. Neuroprotective effects of selective brain hypothermia on permanent focal cerebral ischemia in rats. J Cereb Blood Flow Metab 1997; 17: S40
3 Taniguchi T, Matsui T, Morimoto T, et al. Long-lasting neuroprotective effects of selective brain hypothermia on experimental permanent focal cerebral ischemia. Cereb Blood Flow Metab (Jpn) 1998; 10: 76-77
4 Taniguchi T, Matsui T, Morimoto T, et al. Neuroprotective effects of selective brain hypothermia on experimental permanent focal cerebral ischemia. Cereb Blood Flow Metab (Jpn) 2000; 11: 438-439
5 Taniguchi T, Matsui T, Morimoto T, et al. Neuroprotective effects of selective brain hypothermia on permanent cerebral ischemia. Cereb Blood Flow Metab (Jpn) 2002; 14: 153-154
6 Matsui T, Nagafuji T, Mori T, et al. ?ω-nitro-L-arginine attenuates early ischemic neuronal damage of prolonged focal cerebral ischemia and recirculation in rats. Neurol Res 1997; 19: 192-203
7 Menzies SA, Hoff JT, Betz AL. Middle cerebral artery occlusion in rats: a neurological and pathological evaluation of a reproducible model. Neurosurg 1992; 31: 100-107
8 Garcia JH, Liu KF, Ho KL. Neuronal necrosis after middle cerebral artery occlusion in Wistar rats progresses at different time intervals in the caudoputamen and the cortex. Stroke 1995; 26: 636-643
9 Verhaegen MJJ, Todd MM, Hindman BJ, et al. Cerebral autoregulation during moderate hypothermia in rats. Stroke 1993; 24: 407-414
10 Barone FC, Feuerstein GZ, White RF. Brain cooling during transient focal ischemia provides complete neuroprotection. Neurosci Biobehav Rev 1997; 21: 31-44
11 Miyazawa T, Hossmann KA. Methodological requirements for accurate measurements of brain and body temperature during global forebrain ischemia of rat. J Cereb Blood Flow Metab 1992; 12: 817-822
12 Ohta T, Sakaguchi I, Dong LW, et al. Selective cooling of brain using profound hemodilution in dogs. Neurosurg 1992; 31: 1049-1055
13 Colbourne F, Corbett D, Zhao Z, et al. Prolonged but delayed postischemic hypothermia: a long-term outcome study in the rat middle cerebral artery occlusion model. J Cereb Blood Flow Metab 2000; 20: 1702-1708
14 Maier CM, Sun GH, Kunis D, et al. Delayed induction and long-term effects of mild hypothermia in a focal model of transient cerebral ischemia: neurological outcome and infarct size. J Neurosurg 2001; 94: 90-96
15 Zausinger S, Westermaier T, Plesnila N, et al. Neuroprotection in transient focal cerebral ischemia by combination drug therapy and mild hypothermia: comparison with customary therapeutic regimen. Stroke 2003; 34: 1526-1532
16 Miyazawa T, Tamura A, Fukui S, et al. Effect of mild hypothermia on focal cerebral ischemia. Review of experimental studies. Neurol Res 2003; 25: 457-464
17 Doerfler A, Schwab S, Hoffmann TT, et al. Combination of decompressive craniectomy and mild hypothermia ameliorates infarction volume after permanent focal ischemia in rats. Stroke 2001; 32: 2675-2681
18 Kazan S, Karasoy M, Baloglu H, et al. The effect of mild hypothermia, mannitol and insulin-induced hypoglycaemia on ischaemic infarct volume in the early period after permanent middle cerebral artery occlusion in the rat. Acta Neurochir (Wien) 1999; 141: 979-987
19 Park CK, Jun SS, Kim MC, et al. Effects of systemic hypothermia and selective brain cooling on ischemic brain damage and swelling. Acta Neurochir (Suppl) 1998; 71: 225-228
20 Schwab M, Bauer R, Zwiener U. Mild hypothermia prevents the occurrence of cytotoxic brain edema in rats. Acta Neurobiol Exp 1998; 58: 29-35
21 Winfree CJ, Baker CJ, Connolly ES, et al. Mild hypothermia reduces penumbral glutamate levels in the rat permanent focal cerebral ischemia model. Neurosurg 1996; 38: 1216-1222
22 Connolly ES, Winfree CJ, Stern DM, et al. Procedural and strainrelated variables significantly affect outcome in a murine model of focal cerebral ischemia. Neurosurg 1996; 38: 523-532
23 Baker CJ, Fiore AJ, Frazzini Vl, et al. lntraischemic hypothermia decreases the release of glutamate in the cores of permanent focal cerebral infarcts. Neurosurg 1995; 36: 994-1002
24 Frazzini Vl, Winfree CJ, Choudhri HF, et al. Mild hypothermia and MK-801 have similar but not additive degrees of cerebroprotection in the rat permanent focal ischemia model. Neurosurg 1994; 34: 1040-1046
25 Moyer DJ, Welsh FA, Zager EL. Spontaneous cerebral hypothermia diminishes focal infarction in rat brain. Stroke 1992; 23: 1812-1816
26 Xue D, Huang ZG, Buchan SM, ef al. Immediate or delayed mild hypothermia prevents focal cerebral infarction. Brain Res 1992; 587: 66-72
27 Lo EH, Steinberg GK. Effects of hypothermia on evoked potentials, magnetic resonance imaging, and blood flow in focal ischemia in rabbits. Stroke 1992; 23: 889-893
28 Onesti ST, Baker CJ, Sun PP, et al. Transient hypothermia reduces focal ischemic brain injury in the rat. Neurosurg 1991 ; 29: 369-373
29 Kader A, Brisman MH, Maraire N, et al. The effect of mild hypothermia on permanent focal ischemia in the rat. Neurosurg 1992; 31: 1056-1061
30 Baker CJ, Onesti ST, Barth KNM, et al. Hypothermic protection following middle cerebral artery occlusion in the rat. Surg Neurol 1991; 36: 175-180
31 Kozlowski P, Buchan AM, Tuor UI, et al. Effect of temperature in focal ischemia of rat brain studied by 31P and IH spectroscopic imaging. Magn Res Med 1997; 37: 346-354
32 Baker CJ, Onesti ST, Solomon RA. Reduction by delayed hypothermia of cerebral infarction following middle cerebral artery occlusion in the rat: a time-course study. J Neurosurg 1992; 77: 438-444
33 Morikawa E, Ginsberg MD, Dietrich WD, et al. The significance of brain temperature in focal cerebral ischemia: histopathological consequences of middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab 1992; 12: 380-389
34 Ridenour TR, Warner DS, Todd MM, et al. Mild hypothermia reduces infarct size resulting from temporary but not permanent focal ischemia in rats. Stroke 1992; 23: 733-738
35 Yanamoto H, Nagata I, Niitsu Y, et al. Prolonged mild hypothermia therapy protects the brain against permanent focal ischemia. Stroke 2001; 32: 232-239
Tamiki Taniguchi, Eiharu Morikawa, Takashi Mori and Toru Matsui
Department of Neurosurgery, Saitama Medical Center/School, 1981 Kamoda, Kawagoe, Saitama, Japan
Correspondence and reprint requests to: Dr Tamiki Taniguchi, Department of Neurosurgery, Saitama Medical Center/School, 1981 Kamoda, Kawagoe, Saitama 350-8550, japan. [taniguti@saitama-med.ac.jp] Accepted for publication January 2005.
Copyright Maney Publishing Sep 2005
Provided by ProQuest Information and Learning Company. All rights Reserved