Definition
Analgesics are medicines that relieve pain.
Purpose
Analgesics are those drugs whose primary purpose is pain relief. The primary classes of analgesics are the narcotics, including additional agents that are chemically based on the morphine molecule but have minimal abuse potential; nonsteroidal anti-inflammatory drugs (NSAIDs) including the salicylates; and acetaminophen. Other drugs, notably the tricyclic antidepressants and anti-epileptic agents such as gabapentin, have been used to relieve pain, particularly neurologic pain, but are not routinely classified as analgesics. Analgesics provide symptomatic relief, but have no effect on causation, although clearly the NSAIDs, by virtue of their dual activity, may be beneficial in both regards.
Description
Pain has been classified as "productive" pain and "non-productive" pain. While this distinction has no physiologic meaning, it may serve as a guide to treatment. "Productive" pain has been described as a warning of injury, and so may be both an indication of need for treatment and a guide to diagnosis. "Non-productive" pain by definition serves no purpose either as a warning or diagnostic tool.
Although pain syndromes may be dissimilar, the common factor is a sensory pathway from the affected organ to the brain. Analgesics work at the level of the nerves, either by blocking the signal from the peripheral nervous system, or by distorting the interpretation by the central nervous system. Selection of an appropriate analgesic is based on consideration of the risk-benefit factors of each class of drugs, based on type of pain, severity of pain, and risk of adverse effects. Traditionally, pain has been divided into two classes, acute and chronic, although severity and projected patient survival are other factors that must be considered in drug selection.
Acute pain
Acute pain is self limiting in duration, and includes post-operative pain, pain of injury, and childbirth. Because pain of these types is expected to be short term, the long-term side effects of analgesic therapy may routinely be ignored. Thus, these patients may safely be treated with narcotic analgesics without concern for their addictive potential, or NSAIDs with only limited concern for their ulcerogenic risks. Drugs and doses should be adjusted based on observation of healing rate, switching patients from high to low doses, and from narcotic analgesics to non-narcotics when circumstances permit.
An important consideration of pain management in severe pain is that patients should not be subject to the return of pain. Analgesics should be dosed adequately to assure that the pain is at least tolerable, and frequently enough to avoid the anxiety that accompanies the anticipated return of pain. Analgesics should never be dosed on a "prn" (as needed) basis, but should be administered often enough to assure constant blood levels of analgesic. This applies to both the narcotic and non-narcotic analgesics.
Chronic pain
Chronic pain, pain lasting over three months and severe enough to impair function, is more difficult to treat, since the anticipated side effects of the analgesics are more difficult to manage. In the case of narcotic analgesics this means the addiction potential, as well as respiratory depression and constipation. For the NSAIDs, the risk of gastric ulcers may be dose limiting. While some classes of drugs, such as the narcotic agonist/antagonist drugs bupronophine, nalbuphine and pentazocine, and the selective COX-2 inhibitors celecoxib and rofecoxib represent advances in reduction of adverse effects, they are still not fully suitable for long-term management of severe pain. Generally, chronic pain management requires a combination of drug therapy, life-style modification, and other treatment modalities.
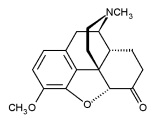
Narcotic analgesics
The narcotic analgesics, also termed opioids, are all derived from opium. The class includes morphine, codeine, and a number of semi-synthetics including meperidine (Demerol), propoxyphen (Darvon), and others. The narcotic analgesics vary in potency, but all are effective in treatment of visceral pain when used in adequate doses. Adverse effects are dose related. Because these drugs are all addictive, they are controlled under federal and state laws. A variety of dosage forms are available, including oral solids, liquids, intravenous and intrathecal injections, and transcutaneous patches.
NSAIDs, non-steroidal anti-inflammatory drugs, are effective analgesics even at doses too low to have any anti-inflammatory effects. There are a number of chemical classes, but all have similar therapeutic effects and side effects. Most are appropriate only for oral administration; however ketorolac (Toradol) is appropriate for injection and may be used in moderate to severe pain for short periods.
Acetaminophen is a non-narcotic analgesic with no anti-inflammatory properties. It is appropriate for mild to moderate pain. Although the drug is well tolerated in normal doses, it may have significant toxicity at high doses. Because acetaminophen is largely free of side effects at therapeutic doses, it has been considered the first choice for mild pain, including that of osteoarthritis.
Recommended dosage
Appropriate dosage varies by drug, and should consider the type of pain, as well as other risks associated with patient age and condition. For example, narcotic analgesics should usually be avoided in patients with a history of substance abuse, but may be fully appropriate in patients with cancer pain. Similarly, because narcotics are more rapidly metabolized in patients who have used these drugs for a long period, higher than normal doses may be needed to provide adequate pain management. NSAIDs, although comparatively safe in adults, represent an increased risk of gastrointestinal bleeding in patients over the age of 60.
Precautions
Narcotic analgesics may be contraindicated in patients with respiratory depression. NSAIDs may be hazardous to patients with ulcers or an ulcer history. They should be used with care in patients with renal insufficiency or coagulation disorders. NSAIDs are contraindicated in patients allergic to aspirin.
Side effects
Review adverse effects of each drug individually. Drugs within a class may vary in their frequency and severity of adverse effects.
The primary adverse effects of the narcotic analgesics are addiction, constipation, and respiratory depression. Because narcotic analgesics stimulate the production of enzymes that cause the metabolism of these drugs, patients on narcotics for a prolonged period may require increasing doses. This is not the same thing as addiction, and is not a reason for withholding medication from patients in severe pain.
NSAIDs are ulcerogenic and may cause kidney problems. Gastrointestinal discomfort is common, although in some cases, these drugs may cause ulcers without the prior warning of gastrointestinal distress. Platelet aggregation problems may occur, although not to the same extent as if seen with aspirin.
Interactions
Interactions depend on the specific type of analgesic. See specific references.
Opioid analgesicsDrugRoute of administrationOnset of action (min)Duration of action (h)
Strong agonists
Fentanyl (Sublimaze)IM
IV7-15
1-21-2
0.5-1
Hydromorphone (Dilaudid)Oral
IM
IV
Sub-Q30
15
10-15
154
4
2-3
4
Levorphanol (Levo-Dromoran)Oral
IM
IV
Sub-Q10-60
-
-
-4-5
4-5
4-5
4-5
Meperidine (Demerol)Oral
IM
IV
Sub-Q15
10-15
1
10-152-4
2-4
2-4
2-4
Methadone (Dolophine)Oral
IM
IV30-60
10-20
-4-6
4-5
3-4
Morphine (many trade names)Oral
IM
IV
Sub-Q
Epidural-
10-30
-
10-30
15-604-5
4-5
4-5
4-5
up to 24
Oxymorphone (Numorphan)IM
IV
Sub-Q
Rectal10-15
5-10
10-20
15-303-6
3-4
3-6
3-6
Mild-to-moderate agonists
Codiene (many trade names)Oral
Im
Sub-Q30-40
10-30
10-304
4
4
Hydrocodone (Hycodan)Oral10-304-6
Oxycodone (Percodan)Oral-3-4
Propoxyphene (Darvon, Dolene)Oral15-604-6
Butophanol (Stadol)IM
IV10-30
2-33-4
2-4
Nalbuphine (Nubian)IM
IV
Sub-Qwithin 15
2-3
within 153-6
3-4
3-6
Pentazocine (Talwin)Oral
IM
IV
Sub-Q15-30
15-20
2-3
15-203
2-3
2-3
2-3
IM= intramuscular; IV = intravenous; sub-Q = subcutaneous
Data from Ciccone, C.D. Pharmacology in Rehabilitation. 2nd ed. Philadelphia: F.A. Davis Co., 1996.
Key Terms
- Acute pain
- Pain that is usually temporary and results from something specific, such as a surgery, an injury, or an infection.
- Analgesic
- Medicine used to relieve pain.
- Chronic pain
- Pain that lasts more than three months and threatens to disrupt daily life.
- Inflammation
- Pain, redness, swelling, and heat that usually develop in response to injury or illness.
- Osteoarthritis
- Joint pain resulting from damage to the cartilage.