Treating children can be a real challenge for physicians and pharmacists. Most drugs approved by the US Food and Drug Administration are not indicated for pediatric use, and physicians must prescribe them "off label." Drug manufacturers do not produce strengths and dosage forms appropriate for children of drugs that are not indicated for this patient population. Fortunately, most children are relatively healthy and rarely require medication, but what happens when a child has to be admitted to the hospital for a medical problem? How can the child receive proper medical attention with such limited pharmaceutical resources? How does a pediatric hospital provide proper medical care when the entire patient population is younger than 21 years?
Working as a compounding pharmacist in a pediatric hospital is daily a unique compounding opportunity. In our hospital, over 40% ot the patient population requires individualized doses or dosage forms; therefore, new treatments and dosage forms are continually developed and studied. As a trained "problem-solver," the compounding pharmacist is instrumental in assisting the medical staff with developing these new treatments and compounded formulations to treat these patients.
Anesthesia and Sedation
Pain and fear of the unknown are two of the most common concerns that children have when admitted to the hospital. Prior to admission, these children have already gone through numerous procedures and tests, so many of them have become apprehensive of adults wearing white coats. Compounded medications can be used to alleviate the anxiety and pain associated with certain procedures. Compounded topical anesthetics, such as lidocaine, epinephrine, and tetracaine (LET) gel, or tetracaine 4% gel, may be used to numb the skin for injections and blood draws, to start intravenous (IV) lines, or to stitch an open wound.1
In the emergency department, LET gel is frequently used when a child needs to have stitches. It can be compounded, packaged into 5-mL unit-dose amber topical syringes, and stored for up to 154 days refrigerated prior to use so that it is immediately available at any hour of the day.2 Since the gel is being applied to open wounds, it should be compounded in a clean or preferably aseptic environment. The gel base may be sterilized via autoclave prior to the addition of the active ingredients. Lidocaine and tetracaine are both anesthetics that block the initiation and conduction of nerve impulses by decreasing the permeability of sodium ions. The epinephrine increases the duration of action of the local numbing effect of the anesthetics by causing vasoconstriction, which slows the vascular absorption of the anesthetics. Epinephrine also reduces the bleeding of the open wound. All three active ingredients have potential toxic effects, primarily cardiovascular, so the child's vital signs should be monitored by the medical staff during the procedure; however, the topical dose is relatively low and an adverse event is unlikely.
When lidocaine 2.5%/prilocaine 2.5% (EMLA) cream was on manufacturer backorder, tetracaine 4% gel was compounded in our pharmacy and used as an alternative. In studies in children, tetracaine 4% gel has a more rapid onset of action than lidocaine/prilocaine cream (30 minutes vs 60 minutes), is as effective, and is not associated with methemoglobinemia, a rare but potentially fatal adverse effect of lidocaine/prilocaine cream.1 Like LET gel, tetracaine 4% gel can be packaged after compounding into 5-mL unit-dose amber topical syringes and stored for immediate use; tetracaine 4% gel can be stored even longer than LET gel, for up to 6 months refrigerated. For hospitals that need to trim their pharmacy budgets, tetracaine 4% gel is an economic alternative to lidocaine/prilocaine cream.
Light or conscious sedation is commonly used in children who must undergo diagnostic or radiographie procedures that require them to remain still, such as a computerized tomography scan. Conscious sedation is less invasive than general anesthesia, allows protective reflexes to remain intact, and does not require intubation to maintain an open airway. Several commercial oral products are available to induce conscious sedation, including chloral hydrate syrup, lorazepam solution, midazolam syrup, and morphine solution. In the past couple of years, however, several of these products, including lorazepam solution and midazolam syrup, have been on manufacturer backorder for extended periods of time. Some children refuse to take commercial products that have a bad taste, such as chloral hydrate. The commercial midazolam syrup contains sodium benzoate, which may cause an allergic reaction in susceptible patients, especially neonates.
When commercial preparations are not available, lorazepam 2-mg/mL suspension may be easily compounded using lorazepam powder.4 The injection product should not be used to compound this preparation because of its high propylene glycol content. Propylene glycol can be toxic to newborns in high doses. If tablets are used to prepare the suspension, the concentration must be reduced to 1 mg/mL because the excipients in the tablets thicken the suspension. The compounded lorazepam suspension is stable for 91 days refrigerated and can be prepared to keep on hand for immediate use when needed. The usual dose for conscious sedation is 0.05 nig/kg (up to a maximum dose of 2 mg) given 90 to 120 minutes prior to the procedure. It has a long duration of action: 8 to 12 hours. It may be repeated every 4 to 8 hours for continued sedation or anxiety. Lorazepam has been associated with neurotoxicity and myoclonus in neonates, especially preterm infants, and may not be a first choice in these patients. All patients should be monitored for cardiovascular side effects, respiratory depression or apnea, and central nervous system depression.
Midazolam 1-mg/mL syrup may be compounded from the commercial injection or powder when the commercial product is not available, or if a patient is allergic to sodium benzoate.5 The compounded preparation is stable for 102 days at room temperature, and again can be prepared ahead of time and kept on hand for immediate use. Dosing is both age and patient specific. Neonates are usually put on continuous IV infusions and not given midazolam orally. Children older than 6 months but younger than 6 years may require doses up to 1 mg/kg. Most children aged between 6 and 16 years can be dosed with 0.25 mg/kg. High-risk pediatric patients whose respiratory or cardiac function is compromised should be started at 0.25 mg/kg. The usual dose for infants older than 6 months and children is 0.2 to 0.4 mg/kg (up to a maximum dose of 20 mg), given 30 to 45 minutes prior to the procedure. This preparation has a much shorter duration of action than lorazepam, only 1 to 3 hours. The same monitoring parameters for lorazepam apply to midazolam.
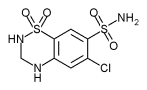
Diuretics
Spironolactone and hydrochlorothiazide are the two diuretics routinely used in children to treat hypertension, primary aldosteronism, edema associated with congestive heart failure, ascites caused by cirrhosis of the liver, and nephrotic syndrome. In these patients, these diuretics may be used as single agents, depending on the medical problem that is being treated, or in combination to increase their effects and reduce the dose of each drug and thus the accompanying side effects. The patient's serum electrolyte and blood urea nitrogen levels, blood pressure, hydration status, and body weight should be monitored while on these medications.
Spironolactone has never been commercially available as an oral liquid and must be compounded for use in neonates and children. It is used as a diuretic in neonates and to treat hypertension, edema, and primary aldosteronism in children. Several different compounded formulations have been studied since the 1980s, and the results of these studies indicate that compounded Spironolactone suspensions are stable for 28 days to 3 months refrigerated depending on the formulation/' It can be batch-compounded and kept on hand for immediate use. The usual dose as a diuretic is 1 to 3 mg/kg/day every 12 to 24 hours for neonates, and 1.5 to 3.3 mg/kg/day in divided doses every 6 to 24 hours for children. Primary aldosteronism is treated with 100 to 400 mg/nr/day in one dose or two divided doses. Spironolactone is a potassium-sparing diuretic; serum potassium levels should be monitored closely in patients taking this drug.
Hydrochlorothiazide was commercially available as an oral liquid until 2003, when it was discontinued by the manufacturer. The commercial oral solution contained sodium benzoate, which could have caused a potentially fatal toxic effect called "gasping syndrome" in neonates if large amounts were ingested. The compounded hydrochlorothiazide suspension contains no sodium benzoate and is very easy to prepare. If Hydrochlorothiazide Powder USP is used in the compound instead of crushed tablets, the suspension is also dye free, which reduces the risk of allergic reactions. The hydrochlorothiazide suspension is stable for 60 days at room temperature or refrigerated and can be batch-compounded and kept on hand for immediate use. The usual dose for neonates and infants younger than 6 months is 2 to 4 mg/kg/day in two divided doses up to a maximum daily dose of 37.5 mg. Infants older than 6 months and children may receive 2 mg/kg/day in two divided doses up to a maximum daily dose of 200 mg. Hydrochlorothiazide can cause hypokalemia.
It is common to use a combination of spironolactone and hydrochlorothiazide to enhance the diuretic effect and keep the serum potassium levels in balance. Once a child's condition is stabilized on both drugs, a combination suspension can be prepared that is stable for 60 days refrigerated.8 The combination preparation has an added benefit of administering one dose of medicine rather than two doses. Some children resist taking medicine, and a single-dose preparation can help to increase compliance.
Antihypertensive Agents
Antihypertensive agents in dosage forms suitable for children are almost nonexistent and must be compounded. Numerous studies have been published involving antihypertensive agents for children, and stability studies for some compounded formulations of these agents also have been published. Table 1 lists widely used antihypertensive agents that may be compounded for pediatric use. Fortunately, several compounding references contain formulations for these agents; these references should be added to the references maintained in the pharmacy (see Suggested Reading and Resources).
Treatments for Clostridium Difficile
Despite efforts to prevent gastrointestinal problems associated with Clostridium difficile, such as administering prebiotics and probiotics, antibiotic-associated pseudomembranous colitis caused by C difficile is still a common occurrence in hospitals.9,10 Metronidazole is used to treat this infection, but it is not commercially available as an oral suspension. A metronidazole suspension can be compounded from crushed tablets, but it has a very nasty taste and most children resist or refuse to take it. The benzoate ester form of metronidazole, however, does not have a bad taste at all and may be used to prepare the suspension.11
Metronidazole benzoate is a heavier ester form than the metronidazole base. Two hundred milligrams of the benzoate ester is equal to 125 mg of the base. Dosing for metronidazole is based on the metronidazole base weight; therefore, the base concentration should be listed on the label of the compound to avoid any confusion about the dose. The metronidazole suspension is stable for 90 days at room temperature and can be batch-compounded to keep on hand for immediate use. The dose for pseudomembranous colitis in infants and children is 30 mg/kg/day divided every 6 hours for 7 to 10 days.
Metronidazole is also used to treat anaerobic infections in neonates, and the dose is both age and weight dependent. Metronidazole is metabolized by the liver, and liver function in neonates is less developed. Neonates younger than 4 weeks old who weigh less than 1200 g should receive 7.5 mg/kg every 48 hours; neonates younger than 7 days who weigh between 1200-2000 g should receive 7.5 mg/kg/day every 24 hours; and neonates who weigh less than 2000 g can be given 15 mg/kg/day in divided doses every 12 hours. Neonates older than 7 days and weighing 1200 to 2000 g should receive 15 mg/kg/day in divided doses every 12 hours, and those weighing over 2000 g should receive 30 mg/kg/day every 12 hours. Dosing for infants and children with anaerobic infection is the same as for pseudomembranous colitis. Metronidazole can cause leukopenia and neutropenia, and therefore the child's white blood cell count should be monitored.
Adrenal Corticosteroids
Adrenal corticosteroids are commonly used in hospitals and have many indications, including acute adrenal insufficiency, inflammation, immunosuppression, congenital adrenal hyperplasia, and neonatal hypoglycemia. In the past few years, however, the adrenal corticosteroids have been on and off manufacturer backorder, especially the injectable dosage forms. Hospitals have been conservative with the injectable supply and switch patients to an oral dosage form if possible. Switching pediatric patients to an oral dosage form, however, has also been a problem.
In July 1998, Cortef (hydrocortisone) suspension was reformulated, and the suspending agent in this commercial product was changed from tragacanth to xanthan gum. Cortef suspension was found not to be bioequivalent to the tablets, and higher doses had to be given of the suspension (19.6 mg/nr/day) than of the tablets (15.2 mg/m^sup 2^/day). As a result, Cortef suspension was voluntarily recalled from the market on July 18, 2000.
Hydrocortisone oral suspension can be compounded from hydrocortisone base powder with sodium carboxymethylcellulose as the suspending agent.12 Tablets, which are also the base form, may be used to prepare the suspension, after being crushed to a fine powder; however, the excipients in the tablets can cause the compound to be unstable, and the beyond-use date is shortened to 30 days refrigerated. The hydrocortisone suspension is stable for 90 days refrigerated and can be batch-compounded to keep on hand for immediate use. Dosing varies depending on the medical condition that is being treated. It is very important to monitor the patient's blood pressure, weight, serum glucose and electrolyte levels, and growth.
Transplants
Although children undergo organ transplants, some of the medications used after transplant to prevent rejection or infection are not available in an oral liquid dosage form. Tacrolimus is used with corticosteroids to prevent graft-versus-host-disease in transplant patients who are not responding to cyclosporin. It can be easily compounded into an oral suspension; however, the compounder should use cytotoxic precautions and prepare the suspension in a biological safety cabinet or barrier isolator." Since a transplant may be done any time, day or night, tacrolimus needs to be batch-compounded and kept on hand, especially if the hospital specializes in transplants. The suspension is stable for 60 days at room temperature. Children generally require higher doses than adults: 0.15 to 0.4 mg/kg/day divided every 12 hours. Transplant patients are constantly monitored for signs of rejection or infection, in addition to blood cell counts with differential, electrolyte levels, liver and kidney functions, and blood tacrolimus concentrations.
Valganciclovir, an antiviral agent, is used in patients undergoing kidney, heart, or kidney/pancreas (but not liver) transplant to prevent cytomegalovirus (CMV) disease acquired from a CMV-positive donor. Valganciclovir is a prodrug of ganciclovir, but a dose of valganciclovir cannot be substituted on a one-to-one basis for ganciclovir owing to differences in the bioavailability. The bioavailability of ganciclovir from an oral valganciclovir dose is 10-fold higher than that of ganciclovir. Although valganciclovir is not indicated for pédiatrie use, it is routinely used for prevention of CMV. The dose is usually 10 to 15 mg/kg/day,14 and treatment should be started within 10 days after transplant and continued for 100 days. Patients need to be monitored for adverse effects, especially blood dyscrasias such as thrombocytopenia and retinal detachment. There are a couple of formulations for valganciclovir suspension that have relatively long beyond-use dates, and these preparations may be compounded and kept on hand for immediate use.15,16 The chocolate-cherry formulation is popular with most children.
There is a nonprofit website that is a very useful resource for obtaining compounding information for transplant patients, called The Drug Monitor (see Suggested Reading and Resources), on which Dr. Nasr Anaizi posts formulations that he has studied and published in pharmacy journals.
Treatments for Cancer
This year there has been a severe shortage of methotrexate injection due to a manufacturer backorder. Although it can cause serious adverse effects, methotrexate is used to treat the following lifethreatening conditions: trophoblastic neoplasms, leukemias, meningeal leukemia, histiocytoses, osteosarcoma, and non-Hodgkin's lymphoma. It also is used to treat severe polyarticular juvenile rheumatoid arthritis that has not responded to other medications. Dosing is very specific to the disease that is being treated, and the drug has a very narrow therapeutic range. The Institute for Safe Medication Practices has included methotrexate on its list of drugs that have a heightened risk of causing significant patient harm when used in error. Errors have occurred resulting in death when oral methotrexate was given daily instead of the recommended weekly dose.
Methotrexate syrup can be compounded from powder into a preservative-free injection or an oral suspension. Compounding of these preparations requires aseptic technique and antineoplastic precautions to prevent harmful exposure to the compounder. Since proper dosing is critical with methotrexate, the potency of the preparation must be verified along with the sterility and pyrogenicity. It can be batch-compounded to keep on hand, but the batch should be quarantined until all of the end product testing has been completed and the results are acceptable. Some compounded methotrexate injection formulas contain a preservative, benzyl alcohol; these should not be used for high-dose therapies, for intrathecal administration, or for susceptible patients such as neonates.
Methotrexate may be compounded into an oral suspension that can be administered by the patient or caregiver at home after the patient has been discharged from the hospital.17 No stability studies have been published on compounded methotrexate, so the United States Pharmacopoeial Convention (USP) guidelines for beyond-use dating of an aqueous preparation must be followed (14 days refrigerated). The short beyond-use dating can be a good safety factor for the patient. Because oral methotrexate is usually dosed weekly, the pharmacist may compound and dispense only two doses at a time.
Mercaptopurine is used in conjunction with methotrexate for maintenance therapy of childhood acute lymphoblastic leukemia and in combination protocols for the treatment of acute myelogenous leukemia, chronic myelogenous leukemia, and non-Hodgkin's lymphoma. Mercaptopurine can be compounded into a suspension from crushed tablets or the monohydrate powder.18 The compound should be prepared specifically for each patient. The formulation reported by Dressman and Poust is stable for 14 days at room temperature.18 For induction therapy, the oral dose is 2.5 to 5 mg/kg/day given once daily, or 70 to 100 mg/m^sup 2^/day once daily. The maintenance oral dose is 1.5 to 2.5 mg/kg/day daily or 50 to 75 mg/m^sup 2^/day once daily. Mercaptopurine should not be administered with food or meals. There are studies suggesting that, in children with acute lymphohlastic leukemia, evening administration may lower the risk of relapse compared to morning administration.
All chemotherapy patients have the following parameters monitored: complete blood count with differential and platelet count, liver function tests, uric acid, urinalysis, and blood urea nitrogen, serum creatinine, electrolyte, and drug levels. The following physical symptoms should be monitored and immediately reported to the physician: fever, sore throat, bleeding, bruising, black or tarry stools, yellowing of the skin or eyes, and shortness of breath.
Diaper Rash and Bedsores
Diaper rash is a common problem for babies and toddlers, but it can turn into an extremely painful condition for children who are immunocompromised, such as transplant recipients or those receiving chemotherapy. A simple diaper rash can quickly turn into a bloody, painful rash because these patients cannot fight off the causative fungi. An oncologist at Riley Hospital for Children routinely treated children who developed these severe rashes and tried all single agents commonly used in treating diaper rash with limited success. The oncologist decided to combine all of the agents into one preparation, with the assistance of the compounding pharmacist, which not only enhanced the therapeutic effect of each ingredient but made it much easier for the nursing staff to apply. This compound, known as "Riley Butt Cream," is now a frequently ordered compound within Clarian Health Partners.
Riley Butt Cream contains the following active ingredients: nystatin, zinc oxide, vitamin A & D ointment, dibucaine, and tincture of benzoin. Nystatin cream and topical powder are the antifungal agents used to treat the causative candidal infection. The zinc oxide provides a protective coating against any urine or feces touching the sensitive skin and rash. It also promotes healing of chapped skin and diaper rash. The vitamin A & D ointment provides temporary relief of discomfort due to the diaper rash. Dibucaine is a topical anesthetic and provides fast, temporary relief for the pain associated with the rash. Benzoin is a mild topical antibiotic and a skin protectant.
Since several jars of the cream are ordered and used daily, it is best to batch-compound this preparation using a commercial grade mixer. Mixing order is very important in preparing this compound.
1. The creams and powder are mixed first into a smooth homogenous paste.
2. The ointments are then incorporated and mixed with the first mixture.
3. Finally, the tincture of benzoin is added last so that it will not "stain" the powder and cause black flecks in the preparation.
Although the stability is untested, it can be given a 6-month beyond-use date, according to United States Pharmacopeia (USP) guidelines.
Proton Pump Inhibitors
Gastrointestinal problems, especially gastroesophageal reflux disease (GERD), are very common in pediatric patients and are treated, like those in adult patients, with proton pump inhibitors. Unfortunately, none of the proton pump inhibitors are commercially available in an oral liquid dosage form and thus they must be compounded into smooth suspensions. Patients who receive medications and feedings through tubes require a compounded suspension, because the enteric coated beads in the capsules will clog the tubes. Tap Pharmaceutical Products, Inc., Lake Forest, Illinois, attempted to produce an oral lansoprazole powder that could be mixed prior to use; however, it contained xantham gum, which thickened the suspension and again clogged the tubes. Tap now has a rapid-dissolve tablet that easily dissolves in water and will not clog the tubes; however, it is cost-prohibitive in the hospital setting and the drug is still in smaller enteric coated beads. Infants younger than 1 year are dosed by weight, and doses cannot be accurately measured using the rapid-dissolve tablets.
Both lansoprazole and omeprazole can be compounded into suspensions to allow for dosing in infants, children, and patients with tubes.19-21 The beyond-use dating for these preparations is relatively short: 45 days refrigerated for omeprazole and 28 days refrigerated for lansoprazole. Since these compounds are ordered frequently in a pédiatrie hospital, preparing them in batches to keep on hand is both efficient and cost-effective. Both suspensions can be prepared in an 8.4% sodium bicarbonate liquid base; however, acidic vehicles must not be used. The sodium bicarbonate base serves two purposes: (1) it stabilizes the active drug, and (2) it neutralizes stomach acid when the dose is administered so that the drug remains active and can be absorbed in the small intestine.
For GERD, dosing of omeprazole and lansoprazole is dependent on the child's age, weight, and metabolic clearance. Omeprazole generally is dosed 1 mg/kg/day once or twice daily in children, although higher doses (up to 3.5 mg/kg/day) may be necessary in younger children (1 to 6 years of age) because of increased metabolic clearance; dosing every 6 to 8 hours may be necessary. Children younger than 2 years may be given 10 mg (body weight
Conclusion
The preparations described here are just a few examples of medications that are compounded in pediatric hospitals. Since most drugs are used "off label" in children, there is a strong need to develop and compound dosage forms for children. Being a compounding pharmacist for a pediatric hospital can be a challenging but rewarding experience. The compounding pharmacist needs to be skilled in doing literature searches, creative in developing goodtasting compounds, and willing to work with the medical staff to resolve treatment problems.
Suggested Reading and Resoure
* Children's Hospital of Philadelphia Extemporaneous Formulations
* CompoundingToday.com (www.compoundingtoday.com)
* The Drug Monitor (www.thedrugmonitor.com)
* International Journal of Pharmaceutical Compounding (www.ijpc.com)
* Lexi-Comp Online (www.online.lexi.com)
* Trissel's Stability of Compounded Formulations. 3rd ed. Washington, DC: American Pharmaceutical Association; 2005.
References
1. Allen LV. Topical gels for skin lacerations. US Pharmacist 1995; 20(6): 86-87.
2. Lidocaine, Epinephrine, and Tetracaine Gel [product information]. Englewood, CO: Baxa Corporation.
3. Taddio A, Gurguis MG, Koren G. Lidocaine-prilocaine cream versus tetracaine gel for procedural pain in children. Ann Pharmacother 2002; 36(4): 687-692.
4. Wan-Man EL, Lugo RA, Rusho WJ et al. Chemical stability of extemporaneously prepared lorazepam suspension at two temperatures. Paper presented at: Annual Meeting of the Pediatric Advocacy Group (PPAG): October 2-5, 2002; St. Petersburg, FL.
5. Soy D, Lopez MC, Salvador L et al. Stability of an oral midazolam solution for premedication in paediatric patients. Pharm World Sci 1994; 16(6): 260-264.
6. Trissel LA. Trissel's Stability of Compounded Formulations. 2nd ed. Washington, DC: American Pharmaceutical Association; 2000: 348-351.
7. Totterman AM, Luukkonen P, Riukka L et al. Formulation of enterai hydrochlorothiazide suspension for premature infants. Eur J Hosp Pharm 1994; 4: 65-69.
8. Allen LV Jr, Erickson MA. Stability of labetalol hydrochloride, metoprolol tartrate, verapamil hydrochloride, and spironolactone with hydrochlorothiazide in extemporaneously compounded oral liquids. Am J Health Syst Pharm 1996; 53(19): 2304-2309.
9. Boehm G, Jelinek J, Stahl B et al. Prebiotics in infant formulas. J Clin Gastroenterol 2004; 38 (Suppl 6): S76-S79.
10. Moro G, Minoli I, Mosca M et al. Dosage-related bifidogenic effects of galacto- and fructooligosaccharides in formula-fed term infants. J Pediatr Gastroenterol Nutr 2002: 34(3); 291-295.
11. Mathew M, Das Gupta V, Bethea C. Stability of metronidazole benzoate in suspensions. J Clin Pharm Ther 1994; 19(1); 31-34.
12. Fawcett JP, Boulton DW, Jiang R et al. Stability of hydrocortisone oral suspensions prepared from tablets and powder. Ann Pharmacother 1995: 29(10):987-990.
13. Allen LV Jr. Tacrolimus oral suspension. US Pharmacist 2000; 25(9): 75-76.
14. Khositseth S, Matas A, Cook ME et al. Thymoglobulin versus ATGAM induction therapy in pediatric kidney transplant recipients: A single-center report. Transplantation 2005; 79(8): 958-963.
15. Anaizi NH, Dentinger PJ, Swenson CF. Stability of valganciclovir in an extemporaneously compounded oral liquid. Am J Health System Pharm 2002; 59(131:1267-1270.
16. Allen LV Jr. Valganciclovir oral liquid for CMV infection. US Pharmacist 2003; 28(6): 60-63.
17. Stuart JF, Caiman KC, Waiters J et al. Bioavailability of methotrexate: Implications for clinical use. Cancer Chemother Pharmacol 1979; 3(4): 239-241.
18. Dressman JB, Poust RI. Stability of allopurinol and of five antineoplastics in suspension. Am J Hosp Pharm 1983; 40(4): 616-618.
19. DiGiacinto JL, Olsen KM, Bergman KL et al. Stability of suspension formulations of lansoprazole and omeprazole stored in amber-colored plastic oral syringes. Ann Pharmacother 2000; 34(5): 600-605.
20. Sharma VK. Comparison of 24-hour intragastric pH using four liquid formulations of lansoprazole and omeprazole. Am J Health Syst Pharm 1999; 56(23Suppl 4): S18-S21.
21. Phillips JO, Metzler MH, Palmieri MT et al. A prospective study of simplified omeprazole suspension for the prophylaxis of stress-related mucosal damage. Crit Care Med 1996; 24(11): 1793-1800.
Linda F. McElhiney, PharmD, RPh * Clarian Health Partners, Inc. * Indianapolis, Indiana
Address correspondence to Linda F. McElhiney, PharmD, RPh, Clarian Health Partners, Inc. E-mail: lmcelhin@clarian.org
Copyright International Journal of Pharmaceutical Compounding Nov/Dec 2005
Provided by ProQuest Information and Learning Company. All rights Reserved