Influenza
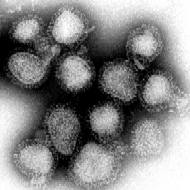
Influenza (or as it is commonly known, the flu or the grippe) is a contagious disease of the upper airways and the lungs, caused by an RNA virus of the orthomyxoviridae family. It rapidly spreads around the world in seasonal epidemics, imposing considerable economic burden, in the form of health care costs and lost productivity. Three influenza pandemics in the 20th century, each following a major genetic change in the virus, killed millions of people. more...
The term influenza has its origins in 15th century Italy, where the cause of the disease was ascribed to unfavorable astrological influences. Evolution in medical thought led to its modification to "influenza di freddo" (meaning "influence of the cold"), which by the 18th century became the prevalent terminology in the English-speaking world as well.
Types
There are three genera of the virus, identified by antigenic differences in their nucleoprotein and matrix protein:
- Influenza A viruses are known to infect humans, other mammals and birds (see also avian influenza) The annual flu vaccine is made by combining new versions of influenza A viruses that nature produces each year.
- Influenza B viruses are known to infect humans and seals
- Influenza C viruses are known to infect humans and pigs .
The A type of influenza virus, also called avian flu virus, is the type most likely to cause epidemics and pandemics. This is because the influenza A virus can undergo antigenic shift and present a new, immune target to susceptible people. Populations tend to have more resistance to influenza B and C, because they only undergo antigenic drift, and have more similarity with previous strains.
The avian flu virus is a species of virus. Its genetic code is RNA not DNA. It mutates very fast by comparison to both DNA and non-viruses. Cold preserves it while heat destroys it. It mutates enough so after a year of mutating in birds, humans can catch the new strain and not be protected by their body from last year's strain. Cold preserves it enough so in the winter it can pass from bird to human to human without being destroyed by heat. Sometimes an avian virus strain mutates into a very deadly version. H5N1 did just that.
Influenza A viruses can be further classified, based on the viral surface proteins hemagglutinin (HA or H) and neuraminidase (NA or N) that are essential to the virus' life cycle. Sixteen H subtypes and nine N subtypes have been identified for influenza A virus. Only one H subtype and one N subtype have been identified for influenza B virus. At present, the most common antigenic variants of influenza A virus are H1N1 and H3N2 (Yohannes et al., 2004).
Yet further variation exists; thus, specific influenza strain isolates are identified by a standard nomenclature specifying virus type, geographical location where first isolated, year of isolation, sequential number of isolation, and HA and NA subtype (Yohannes et al., 2004) Examples of the nomenclature are A/Moscow/10/99 (H3N2) and B/Hong Kong/330/2001.
The term superflu is used to refer to a strain of flu that spreads unusually quickly, is unusually virulent, or for which the host is uncommonly unresponsive to treatment— the kinds of strains which cause epidemics or pandemics. There is no exact scientific definition of a superflu.
Read more at Wikipedia.org