Background & objectives: Lamotrigine is a relatively newer antiepileptic drug used in the treatment of partial seizures. It has a narrow therapeutic index and hence the achieved blood level of the drug is closely related to the therapeutic efficacy and toxicity. The bioavailability of lamotrigine is affected by food, hence the present study was done to investigate the effect of two types of food on the bioavailability of lamotrigine.
Methods: A randomized, open-label, three treatment, three period, single dose and cross-over study was done in nine healthy male volunteers. A single dose of lamotrigine (100 mg) was administered at three occasions: after a north Indian diet (high calorie, high fat), after a south Indian diet (low calorie, low fat), and after an overnight fasting. Serial blood samples were collected up to 24 h post dose. Plasma lamotrigine concentrations were determined and pharmacokinetic parameters studied.
Results: A statistically significant decrease in rate and extent of absorption was observed with north Indian diet and south Indian diet when compared with fasting group. Presence of both types of food causes decrease in mean values of C^sub max^, AUC^sub (0-t)^ and AUC^sub (0-α)^ thus reducing the bioavailability of lamotrigine at significant level (P
Interpretation & conclusion: Lamotrigine should be taken preferably in fasting condition, as presence of food (low fat, low calorie or high fat, high calorie) decreases the bioavailability to a significant extent.
Key words Bioavailability - food - lamotrigine - pharmacokinetics
The nutrients, non-nutrients and other contents present in the food are known to affect the bioavailability of the drugs. Concomitant administration of drug with food is a common practice that may inadvertently reduce or enhance the drug effect. However, in order to evaluate the clinical relevance of a food-drug interaction, the impact of food intake needs to be quantified. These interactions are associated with a high risk of treatment failure, which arises from a reduced bioavailability in the fed state1. Such interactions frequently occurred due to chelation with components in food or dairy products, or by other direct interactions between the drug and certain food components. In addition, the physiological response to food intake, in particular gastric acid secretion, may reduce the bioavailability of certain drugs. In other cases, rate of absorption is decreased, but the extent and the rate of elimination are not decreased due to the presence of food2. For certain drugs such as albendazole, griseofulvin, etc., concomitant food intake may result in an increase in drug bioavailability, and such an increase results in increase in drug effect, but in others such as halofantrine it may result in serious toxicity3.
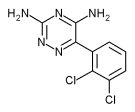
Lamotrigine [6-(2,3-dichloro phenyl)-1,2,4 triazine-3, 5 diamine] is a relatively newer antiepileptic drug used in treatment of partial seizures. The achieved blood level of the drug is closely related to the therapeutic efficacy and toxicity4. The absorption of lamotrigine is affected by the presence of food (according to the drug approval documents submitted by Glaxo SmithKline to US Food and Drug Administration (FDA), the innovator company)5. To our knowledge, no other information is available regarding pharmacokinetics of lamotrigine when taken with food in Indian population. The Indian breakfast is known to affect the bioavailability of drugs6. Hence, the present study was designed to investigate the effect of food on absorption kinetics of lamotrigine in healthy adult human male volunteers.
Material & Methods
The study was carried out as per WHO guidelines for Good Clinical Practice (GCP) for trials of pharmaceutical products7. The study protocol and the informed consent form (ICF) were approved by Jamia Hamdard Institutional Review Board (JHIRB), New Delhi. The study was carried out at Ranbaxy Clinical Pharmacology Unit (RCPU), Majeedia Hospital, New Delhi. Written informed consent was obtained from all the subjects prior to the enrollment in the study.
Study subjects: The volunteers were selected randomly from the volunteer bank of RCPU, Majeedia Hospital. Of the 20 volunteers who underwent a standardized screening procedure, nine were included in the study [age 27.88 ± 7.62 yr (range 18-44 yr), weight 58.5 ± 7.65 kg (range 48-68 kg) and height 166.88 ± 4.51 cm (range 159-173 cm)]. The subjects were selected on the basis of exclusion and inclusion criteria. The inclusion criteria were (i) age range of 18-45 yr; (ii) normal health as determined by medical history and physical examination of the subjects performed within 15 days prior to the commencement of the study; (iii) absence of disease markers of HIV-1 and -2, hepatitis B virus and syphilis infection; and (iv) normal haematology and biochemistry parameters. The exclusion criteria were (i) history of any allergy to lamotrigine and related compounds; (ii) organ dysfunction or history of serious disease; (iii) regular smoker who smoke more than 10 cigarettes daily or had difficulty in abstaining from smoking for the duration of each study period; (iv) history of drug dependence or excessive alcohol intake; (v) used any enzyme modifying drugs within 30 days or any systemic medication [including over the counter (OTC) preparation]; and (vi) participated in any clinical trial within six weeks preceding day one of this study or donated and/or lost more than 350 ml of blood in the past three months.
Study design: The study was a randomized, open-label, three treatment, three period, single dose, cross-over study to where fasting served as a reference. The subjects were given diets assigned as treatment A (north Indian breakfast, wheat based high fat, high calorie diet), treatment B (south Indian breakfast, rice based, low fat, low calorie diet) and treatment C (as fasting) as per the randomization schedule with the drug lamotrigine. North Indian diet (treatment A) consists of pooris (made with 100 gm raw wheat flour, 5 medium), chana (chole kabuli, 150 gm) and mint coriander chutney (20 gm). South Indian diet (treatment B) consists of idlis [(rice : urad dal) (2:1), 4 medium], sambhar (normal, 130 gm) and chutney [bengal gram: coconut (1:1), 70 gm]. Treatment A contained fat 53, protein 9.7 and carbohydrate 37.9 per cent, total 980 Kcal. Treatment B contained fat 16, protein 12 and carbohydrate 72.2 per cent, total 659 Kcal8. All the subjects were required to fast over night before 100 mg lamotrigine administration and 4 h of post dose for treatment C. The single oral dose of 100 mg of lamotrigine (Lamitor® tablets, Torrent Pharmaceuticals, Ahmedabad, India) was given 30 min after the intake of treatment A and B. Each tablet of lamotrigine was administered with 240 ml of drinking water. A wash out period of 7 days was given between two periods. Water restriction was enforced for water 1 h prior to dosing and 2 h post-dose. All the subjects were monitored for oral temperature, blood pressure at sitting position and radial pulse at the time of admission, prior to dose administration and before discharge.
Sample collection: The blood samples (3 ml each) were collected prior to lamotridine and at 0.25, 0.50, 0.75, 1.0, 1.25, 1.5, 2.0, 3.0, 4.0, 6.0, 8.0, 10.0,12.0 and 24.0 h after the dose administration. Samples were collected in vacutainers and immediately centrifuged under refrigeration to separate plasma. Plasma samples were stored in polypropylene tubes at -70°C until analysis.
Sample analysis: The protein precipitation method9 by high performance liquid chromatography (HPLC) was used. The instrument consisted of analytical column Lichrosphere RP 185 m, Guard column 100, RP 185, 5µm (Merck®) water delta 600 pump with photo diode array (PDA) detector (310 nm), Millennium 32 software for the data processing. The mobile phase consisted of phosphate buffer: methanol: acetonitrile (60:30:10, pH 7.1). The mobile phase was prepared from mixture of disodium hydrogen phosphate (Na^sub 2^HPO^sub 4^) and sodium dihydrogen phosphate (NaH^sub 2^PO^sub 4^) salt in water for HPLC, from Merck (8 parts of Na^sub 2^HPO^sub 4^ and 2 parts of NaH^sub 2^PO^sub 4^) with molarity of the buffer solution as 10 mmol/l, at pH 7.1. The linearity, precision and accuracy evaluations were performed on four replicates of spiked plasma samples. The method was linear from 0.16 to 10.0 µm/ml. The stability ranged between 89 to 103 per cent. The total recovery of lamotrigine was 76.05 per cent. The stability ranged for one thaw cycle and two-thaw cycle was 84 to 92 per cent and 90 to 100 per cent respectively. During the course of validation r was constantly greater than 0.99. To 100 µl of plasma from samples, 200 µl of acetonitrile (S.D. Fine Chemicals, New Delhi) was added and vortexed for 2 min and then centrifuged at 900 g for 10 min using cold centrifuge to ensure complete precipitation. The 100 µl of supernatant was injected into column for HPLC analysis at a flow rate of 1.5 ml/min. Lamotrigine was measured at 310 nm using PDA detector.
Pharmacokinetic and statistical analysis: Pharmacokinetic parameters viz., maximal plasma concentration after lamotrigine administration (C^sub max^), time when Cmax achieved (T^sub max^), terminal half life (t^sub 1/2,^), area under plasma concentration vs time curve from time zero to the concentration at 24 h (AUC^sub 0-t^) and area under plasma concentration vs time curve from time zero to concentration at infinite time (AUC^sub 0-α^) were calculated for lamotrigine using Biopak software version 2.1/Win Nonlin professional software version 1.5 (Scientific Consulting, Inc., USA). The statistical differences of pharmacokinetic parameters between the treatments and fasting groups were analyzed by ANOVA on data obtained from all the subjects. Confidence interval (CI 95%) was calculated for all treatments. Ratio analysis was calculated using the Least Square Mean (LSM) for both untransformed and log transformed pharmacokinetic parameters10. A probability of 5 per cent (P
Results
The administration of lamotrigine did not show any adverse effects (AEs) in the subjects. AEs were recorded after every 4 h interval and vital signs were recorded after; oral temperature, BP at sitting position and radial pulse were measured for all the subjects at the time of their check in, prior to the dose administration, 1 h post-dose, 12 h post-dose and before check out during the entire study. Physical examinations and clinical laboratory tests including hemoglobin, total white blood cells count, differential WBC count, erythrocyte sedimentation rate (ESR), serum creatinine, blood urea, serum aspartate amino transferase (AST), serum alanine amino transferase (ALT), serum alkaline phosphatase, serum bilirubin, serum glucose (fasting), serum cholesterol, and urine (routine and microscopic) were within normal limits for all the subjects during and after completion of the study. A significant difference was seen in the mean values of T^sub max^, C^sub max^, AUC^sub (0-t)^, and AUC^sub (0-α)^ with north and south Indian diets (Table I). The log transformed ratios for C^sub max^, AUC^sub (0-t)^ and AUC^sub (0-α)^ between different treatments at 95 per cent CI are presented in Table II and the mean plot for the mean lamotrigine plasma concentration for the subjects under different treatments is presented in Fig. 1.
Percentage difference between treatments A and C: The per cent difference of treatment A with treatment C for T^sub max^, C^sub max^, AUC^sub 0-t^ and AUC^sub 0-α^ were 21.44, -61.45, -52.89 and -24.32 per cent respectively.
Percentage difference between treatments B and C: The per cent difference of treatment B with treatment C for T^sub max^, AUC^sub 0-t^ and AUC^sub 0-α^, were -3.041, -29.39, and -25.94 per cent respectively.
Discussion
Epilepsy is a chronic disease requiring long term therapy, so choice of drug should be such that therapeutic efficacy is maintained with minimal adverse effects (AEs). Mostly the AEs are related to plasma concentration i.e., rate of adverse effect increases as dose increases or vice-versa11. The decrease in peak plasma concentration (Cmax) is often advantageous if the area under curve (AUC) is not affected. Various drugs like cefaclor (immediate release), rufinamide, bropirimire, fenretinide, nifedipine, vinpocetine, etc., have decrease in C^sub max^, which increases the absorption of drug from the gastrointestinal tract without affecting the bioavailability12. The log transformed ratio for C^sub max^ in treatment A vs C and treatment B vs C were 38.63 and 67.18 respectively. Both the ratios are unacceptable suggesting a significant influence of food (specially in treatment A which was high calorie) on the absorption of lamotrigine. This observation is similar to that shown by cholinesterase inhibitor, ambenoium chloride, where C^sub max^ and AUCs were decreased but T^sub max^ was moderately increased13.
The log transformed AUC^sub (0-α)^ ratio between treatments A and C was 67.24 and 72.20 when treatments B was compared with treatment C. Although the ratio is unacceptable according to FDA guidelines7, but still the ratio (72.20) is quite near to 100 per cent which suggests that lamotrigine if necessary, can be administered with treatment B as it is possible to reduce the various adverse reactions associated with drug when taken in fasting state. Ideally, the ratio between AUC^sub 0-t^/AUC^sub 0-α^ for any drug should be 0.87, but it was found to 0.47 for treatment A and 0.58 for treatment B. The lower value is because of inadequate sampling points set up during the study. Blood samples should have been collected for 4-5 time half life of lamotrigine, but since lamotrigine possesses a very long half life of 24-29 h, it was not possible to sample more than one half life due to certain practical problems. Moreover, it is in agreement with a previous study where sampling was carried out till 24 h14 and additionally, it is only the absorption phase, which was under study. So initial samples were taken quite frequently than latter part of study schedule.
The t^sub ½β^ of lamotrigine was found to vary from 10-17 h when fasting group was compared with fed groups. Although the variation in t^sub 1/2β^ is well documented after single dose administration of lamotrigine, which subsides on multiple dosing15. However, in the present study, the variation in t^sub 1/2β^ can be inferred because of inadequate sampling of blood from subject in each period.
It can be concluded from the present study that lamotrigine should be taken in fasting condition with at least 4 h post-dose administration, as this is the mean gastric emptying time required for any drug to pass through stomach. The presence of high fat, high calorie diet decreases the bioavailability of lamotrigine to a great extent.
Acknowledgment
The authors thank Torrent Pharmaceuticals Ltd., Ahmedabad for providing samples of drugs, and University Grants Commission (UGC), New Delhi for providing research fellowship to one of the author (Ms Charu Sharma) and Ranbaxy Research Laboratories, Gurgaon for providing clinical services utilized in the study.
References
1. Schmidt LE. Dalhoff K. Food-drug interactions. Drugs 2002; 62 : 1481-502.
2. Karim S, Ahmed T, Monif T, SahaN, Sharma PL. The effect of four different types of food on the bioavailability of cefaclor. Eur J Drug Metab Pharmacokinet 2003; 28: 185-90.
3. Singh BN. Effects of food on clinical pharmacokinetics. Clin Pharmacokinet 1999; 37 : 213-55.
4. Eadie MJ. Therapeutic drug monitoring - antiepileptic drugs. Br J Clin Pharmacol 2001 ; 52 (Suppl 1) : S11-20.
5. Centre for Drug Evaluation and Research(CDER). New and Generic drug approvals 1998-2004, Glaxo -Wellcome, Lamictal Advisory Board Briefing Document; USA 1997.
6. Vasu S, Adithan C, Shashindran CH, Azad M, Koumaravelou K, Topno I. Effect of two types of Indian breakfast on bioavailability of cefuroxime axetil. Indian J Med Res 2000; 112 : 104-8.
7. Guidance for industry (draft guidance). Food effect bioavailability and bioequivalence studies, US Department of Health and Human Services, Food and Drug Administration. Centre of Drug Evaluation and Research (CDER) USA; 2002 p.1-12.
8. Narasinga Rao BS, Deasthale YG, Pant KC. Nutritive value of Indian foods, National Institute of Nutrition, Hyderabad : Indian Council of Medical Research (ICMR); 1989.
9. Bottiger Y, Svensson JO, Stahle L. Lamotrigine drug interactions in a TDM material. Ther Drug Monit 1999; 21 : 171-4.
10. Khan AH, MonifT, Shah N, SharmaPL. Influence of dietary source and fat content on the bioavailability of an extended release formulation of cefaclor in healthy human volunteers. Abstracts of XXXIII Annual Conference of the Indian Pharmacological Society, Gandhinagar, December 28-30, 2000. Indian J Pharmacol 2001; 33 : 55.
11. Welling PG. Effects of food on drug absorption. Pharmacol Ther 1989; 43 : 425-41.
12. Brahmankar DM, Jaiswal SB. Absorption of drugs. In: Biopharmaceutics and clinicalpharmacokinetics- A treatise. 1st ed. Delhi: Vallabh Prakashan; 2000 p. 5-74.
13. Ohtsubok K, Fujii N, Higuchi S, Aoyama T, Goto I, Tatsuhara T. Influence of food on serum ambenonium concentration in patients with myasthenia gravis. Eur J Clin Pharmacol 1992; 42 : 371-4.
14. Garnett WR. Lamotrigine pharmacokinetics. J Child Neural 1997;32 (Suppl 1): S10-5.
15. Peck AW. Clinical pharmacology of lamotrigine. Epilepsia 1991; 32 (Suppl2): S9-12.
C. Sharrna#*, R. Dubey*, H. Kumar+ & N. Saha++
* Department of Pharmaceutics, Delhi Institute of Pharmaceutical Sciences (DIPS), + Clinical Pharmacologist, & ++ Ranbaxy Clinical Pharmacology Unit, Majeedia Hospital, New Delhi, India
Received January 21, 2004
# Present address: Dabur Research Foundation, 22, Site IV Ghaziabad, India
Reprint requests: Dr Nilanjan Saha, Head, Clinical Research & Medical Services, Dabur Research Foundation 22, Site IV, Sahibabad, Ghaziabad 201010, India
e-mail: sahan@dabur.com
Copyright Indian Council of Medical Research May 2005
Provided by ProQuest Information and Learning Company. All rights Reserved