INTRODUCTION
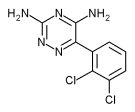
Although a large number of psychotropic agents have been investigated for the treatment of cocaine addiction, none has clearly demonstrated efficacy in clinical trials. This lack of success has pointed out the need to evaluate agents that possess mechanisms of action different from those hitherto investigated, which have been primarily dopaminergic or monamingeric in activity. Agents that modulate the excitatory amino acid (EAA) system have been the subject of recent attention in the addictions [e.g., (1)]. Here we report on a preliminary study of lamotrigine, a novel anticonvulsant medication. Neurochemical studies suggest that lamotrigine indirectly decreases release of glutamate, a widely occurring EAA, through inhibition of voltage-sensitive sodium channels (2, 3). In animal seizure tests, the pharmacologic profile of lamotrigine is similar to that of carbamazepine (4), an anticonvulsant that has been investigated for the treatment of cocaine addiction with mixed results (cf. 5, 6). Lamotrigine and carbamazepine, however, possess a number of potentially significant differences. Although they both decrease membrane excitability, they are structurally unrelated, and research has suggested that they differ in their specific mode of interaction with the sodium channel (7). Findings also indicate that lamotrigine, but not carbamazepine, prevents MPTP-induced dopamine depletion in mice (8). Studies with epileptic patients have found that lamotrigine has a low potential for toxicity, is nonsedating, and is better tolerated than carbamazepine (9-11). A preliminary evaluation of lamotrigine for the treatment of cocaine abuse was suggested by its potential to offer protection against cocaine's neurotoxic effects as well as by the possibility that it may decrease cocaine use.
A number of studies indicate that cocaine is neurotoxic (cf. 12) and that this neurotoxicity may be glutamate mediated. Systemic vasoconstriction subsequent to cocaine use may cause brain ischemia (13), which is associated with excess glutamate release and with subsequent injury, or death, to neurons due to excessive calcium influx (14). There are suggestions in the literature that the neurotoxic effects of glutamate may be potentiated by dopamine (12, 15). These processes may be responsible, in part, for the patchy perfusion deficits in cerebral cortical blood flow revealed by SPECT scans of cocaine-dependent individuals (13, 16), and for the neuropsychological deficits found in this patient population (17, 18). The theoretical implications of lamotrigine's glutamate-inhibiting properties for reducing cocaine-mediated neurotoxicity is supported by a number of preclinical studies; for example, in the rat lamotrigine has been found to protect against presumptive glutamate-mediated phenomena such as neurological deficits following ischemia (19, 20), as well as kainic acid neurotoxicity (21).
Lamotrigine's potential utility as a treatment agent for cocaine abuse stems from research into glutamatergic control of dopamine release (cf. 1, 22). Findings suggest that EAA antagonists decrease the ability of cocaine to elevate extracellular dopamine levels in the striatum (23), as well as cocaine-stimulated extracellular dopamine levels in the nucleus accumbens (24). This is supported by preclinical studies that indicate that EAA antagonists alter cocaine self-administration in rats (25) and reduce cocaine's behavioral effects (26). Because dopamine is thought to be central to the rewarding effects of cocaine (27), this raises the possibility that these effects may be reduced by lamotrigine, through glutamate inhibition.
An agent that both decreases cocaine use and is potentially neuroprotective may have clinical utility for a wide variety of chronic cocaine abusers. These properties may be of particular relevance to the subpopulation of HIV-seropositive cocaine abusers, who may be at heightened risk for neurological damage from the additive or synergistic neurotoxic effects of cocaine use and HIV disease. Although the relative contributions of illicit drug use and HIV disease to cognitive impairment is unclear (cf. 28), several studies have found higher levels of cognitive impairment in HIV-seropositive methadone-maintained patients compared to HIV-seronegative methadone-maintained patients (29, 30). There are suggestions in the literature that the neurotoxicity of the HIV-1 glycoprotein gp120 secreted by HIV 1-infected macrophages may be mediated by overactivation of NMDA-type EAA receptors (31, 32), raising the possibility that a glutamate-inhibiting agent such as lamotrigine might offer additional neuroprotection for HIV-seropositive drug abusers.
Although HIV-seropositive cocaine-abusing individuals have been the subject of numerous epidemiologic and demographic studies (cf. 33), and may constitute an especially difficult to treat patient population (34), we are not aware of any cocaine pharmacotherapy trial that has specifically targeted this patient group. In view of the urgent need to develop treatments for cocaine-abusing, HIV-seropositive patients, the current study evaluated lamotrigine in a sample composed exclusively of these patients.
One concern regarding anti-glutamatergic agents is that, although they may confer neuroprotective effects, they may also interfere with experience-dependent cellular plasticity (e.g., long-term potentiation) and hence may disrupt learning and memory (35). Although lamotrigine is apparently free of such cognitive side-effects (36-38), there are no data of which we are aware regarding lamotrigine's effects on cognitive functioning in HIV-seropositive individuals. The current study therefore had two primary goals: (1) to conduct a preliminary evaluation of lamotrigine's efficacy for cocaine addiction, based on urine toxicology screens and self-reported drug use, and (2) to explore lamotrigine's effects on cognitive functioning by administering a neuropsychological assessment battery pre- and posttreatment.
METHODS
Participants
Participants were 18 (11 male; 7 female) HIV-seropositive patients enrolled in an inner-city methadone maintenance program. All subjects met DSM-IV criteria for cocaine dependence. Fifty percent used cocaine by intravenous route of administration: 44% by smoking (freebasing) and 6% intranasally. Subjects dependent on any substance other than opiates, cocaine, or nicotine were excluded from the study, as were women who were pregnant or not using adequate birth-control measures. Twelve subjects (67%) were maintained on methadone [82 ([+ or -] 10) mg/day], and six were maintained on buprenorphine (12 mg/day). The mean age of participants was 39 ([+ or -] 6.4) years; 6 (33%) were white; 10 (56%) African American; and 2 (11%) Hispanic. Seven (39%) had completed high school; 94% were unemployed.
Patients had been using opiates for 15.2 ([+ or -] 7.3) years and cocaine for 13.3 ([+ or -] 6.7) years. The week prior to entering the study they reported using cocaine an average of 3.3 ([+ or -] 2.4) days per week and used an average of 1.3 ([+ or -] 2.3) grams per week. Severity of drug use as assessed by the Addiction Severity Index (ASI) was .35 ([+ or -] .08). Patients had 4.4 ([+ or -] 3.4) unsuccessful prior drug treatment episodes. The length of time since testing HIV-seropositive ranged from 3 to 11 years [mean: 6.5 ([+ or -] 2.4) years]; CD4 counts ranged from 45 to 771 [mean: 355 ([+ or -] 236)]; five patients had CD4 counts less than 200. Seven patients were taking antiretroviral medications (AZT, four patients; D4T, two patients; DDI, one patient).
Treatments
The target dose of lamotrigine for this study was 300 mg/day. We began by employing a 6-week induction schedule, recommended for lamotrigine in the treatment of epilepsy. After the first eight patients, the schedule was halved to three weeks, in order to explore whether the target dose could be attained more rapidly, yielding a longer period of time for patients to be maintained on the full dose in a standard 3-month study. This change offered the opportunity to compare the treatment outcomes of patients assigned to these two induction schedules. Patients in the standard induction group (n = 8) reached full dose in week 6, on the following schedule: weeks 1 and 2, 50 mg/day; weeks 3 and 4, 100 mg/day; week 5, 200 mg/day; weeks 6-12, 300 mg/day. Patients in the accelerated induction group (n = 10) reached full dose in week 3, on the following schedule: week 1, days 1-3, 50 mg/day; week 1, days 4-7, 100 mg/day; week 2, 200 mg/day; weeks 3-12, 300 mg/day.
Treatment Context
The context in which lamotrigine was investigated comprised daily opiate-agonist treatment (methadone or buprenorphine), case management, and twice-weekly manual-guided psychosocial group therapy (Risk Reduction Therapy) (39) delivered by two master's-level clinicians. The psychosocial treatment was developed specifically for use with HIV-seropositive drug abusers who may have cognitive impairment, and employs cognitive remediation strategies traditionally used in rehabilitation settings with patients with traumatic brain injury. These include multimodal presentation of material, simplification of content, frequent review of material with quizzes and feedback, and extensive use of memory books and behavioral games.
Procedure and Assessments
After determination that the patient was eligible for the study, informed consent was obtained, and the assessment battery was administered. This included the substance abuse sections of the SCID for DSM-IV (40), the Addiction Severity Index (41), the Beck Depression Inventory (42), the State--Trait Anxiety Scale (State Version) (43), the Wechsler Adult Intelligence Scale--Revised (WAIS-R) (44), and nine neuropsychological tests: Rey Auditory Verbal Learning Test (RVLT) (45); the visual reproduction and logical memory subtests (immediate and delayed) of the Wechsler Memory Scales--Revised (WMS-R) (46); Paced Auditory Serial Addition Test (PASAT) (47); Controlled Oral Word Association Test (COWA) (48); Trail Making Tests A and B (49). Assessments were repeated posttreatment. Urine samples were collected three times weekly and analyzed for benzoylecognine using the Abbott Tdx/Adx method (50); levels greater than 300 ng/ml were counted as positive. Self-reported frequency of cocaine use and average cocaine craving as well as medication side-effects were assessed weekly.
RESULTS
Patients assigned to the two treatment groups did not differ on any measured sociodemographic or drug use variable, with the exception of race. Subjects assigned to the accelerated-induction schedule were more likely to be ethnic minorities ([chi square] = 6.12, p [is less than] .05). Outcome data were therefore first analyzed by race; no significant differences were found, and results are presented collapsed across race. Table 1 presents demographic and drug use data by treatment group.
Although agents that modulate glutamate release offer the potential to simultaneously target a number of areas pertinent to HIV-seropositive cocaine abusers, they may also benefit HIV-negative cocaine abusers as well. However, results obtained in either group may not be generalizable to the other. Future studies could examine lamotrigine in HIV-negative as well as HIV-seropositive cocaine-abusing patients, perhaps employing a 2(HIV status) X 2(medication/ placebo) design. Although the epilepsy literature does not suggest a clear relationship between lamotrigine blood levels and clinical response, dose-ranging studies may also be useful in a cocaine-abusing population.
We conclude that lamotrigine, 300 mg/day, inducted over 6 weeks, appears to be well tolerated in a group of HIV-seropositive cocaine-abusing subjects and may decrease cocaine use. It therefore warrants further investigation for the treatment of cocaine abuse. Longer studies may be needed to evaluate lamotrigine's effect on neuropsychological performance, both for patients who continue to abuse cocaine as well as for those who attain abstinence and continue taking the mediation.
ACKNOWLEDGMENTS
Supported by grants DA09250 (Medications Research Development Center), DA00277 (SKA), and DA00112 (TRK) from the National Institute on Drug Abuse, National Institutes of Health. We wish to thank Charles Bradberry, Ph.D., and Steve Grant, Ph.D., for helpful criticism of an earlier draft of this article.
REFERENCES
(1.) McGinty, J. F., Introduction to the role of excitatory amino acids in the actions of abused drugs: A symposium presented at the 1993 annual meeting of the College on Problems of Drug Dependence, Drug Alcohol Depend. 37:91-94 (1995).
(2.) Leach, M. J., Marden, C. M., and Miller, A. A., Pharmacological studies on lamotrigine, a novel potential antiepileptic drug: II. Neurochemical studies on the mechanism of action, Epilepsia 27:490-497 (1986).
(3.) Meldrum, B., and Leach, M., The mechanisms of action of lamotrigine, Reviews of Contemporary Pharmacotherapy 5:107-114 (1994).
(4.) Miller, A. A., Wheatley, P., Sawyer, D. A., Baxter, M. G., and Roth, B. Pharmacological studies on lamotrigine, a novel potential antiepileptic drug: I. Anticonvulsant profile in mice and rats, Epilepsia 27:483-489 (1986).
(5.) Cornish, J. W., Maany, I., Fudala, P. J., Neal, S., Poole, S. A., Volicelli, P., and O'Brien, C. P. Carbamazepine treatment for cocaine dependence, Drug Alcohol Depend. 38(3):221-227(1995).
(6.) Halikas, J. A., Kuhn, K. L., Crea, F. S., Carlson, G. A., and Crosby, R. Treatment of crack cocaine use with carbamazapine, Am. J. Drug Alcohol Abuse 18(1):45-56 (1992).
(7.) Xie, S., Landaster, B., and Peakman, T. Interaction to the antiepileptic drug lamotrigine with recombinant rat brain ripe IIA Na channels and with native Na channels in rat hippocampal neurones, Pflugers Archive-European Journal of Physiology 430:437-446 (1995).
(8.) Jones-Himble, S. A., Morgan, P. F., and Cooper, B. R. The novel anticonvulsant lamotrigine prevents dopamine depletion in C57 black mice in the MPTP animal model of parkinson's disease, Life Sciences 54:245-252 (1993).
(9.) Brodie, M. J., Lamotrigine versus other antiepileptic drugs: A star rating system is born, Epilepsia 35(Suppl 5):S41-S46 (1994).
(10.) Fitton, A., and Gao, K. L., Lamotrigine: An update of its pharmacology and therapeutic use in epilepsy, Drug Evaluation 50(4):691-713 (1995).
(11.) Yuen, A. W. C., Lamotrigine vs. carbamazepine as monotherapy in patients with newly diagnosed or recurrent epilepsy, Epilepsia 35(Suppl 8):31 (1994).
(12.) Majewska, M. D., Cocaine addiction as a neurological disorder: Implications for treatment, in Neurotoxicity and Neuropathology Associated with Cocaine Abuse, Vol. 163 (M. D. Majewska, Ed.), NIDA Research Monograph, Washington, D.C., 1996, pp. 1-26.
(13.) Kosten, T. R., Malison, R., and Wallace, E., Neuropsychological abnormalities in cocaine abusers: Possible correlates in SPECT neuroimaging, in Neurotoxicity and Neuropathology Associated with Cocaine Abuse, Vol. 163 (M. D. Majewska, Ed.), NIDA Research Monograph, Washington, D.C., 1996, pp. 175-192.
(14.) Lipton, S. A., and Rosenberg, P. A., Excitatory amino acids as a final common pathway for neurologic disorders, N. Engl. J. Med. 330(9):613-622 (1994).
(15.) Wood, E. R., Coury, A., Blaha, C. D., and Phillips, A. G., Extracellular dopamine in the rat striatum during ischemia and reperfusion as measured by in vivo electrochemistry and in vivo microdialysis, Brain Research 591:151-159 (1992).
(16.) Holman, B. I., Carvalho, P. A., Mendelson, J., Teoh, S. K., Nardin, R., Hallgring, E., Hebben, N., and Johnson, K. A., Brain perfusion is abnormal in cocaine-dependent polydrug users: A study using technetium-99m-HMPAO and ASPECT, Journal of Nuclear Medicine 32:1206-1210 (1991).
(17.) Herning, R. I., Glover, B. J., Koeppl, B., Weddington, W., and Jaffe, J. H., Cognitive deficits in abstaining cocaine abusers, in Residual Effects of Abused Drugs on Behavior, Vol. 101 (J. W. Spencer and J. J. Boren, Eds.), NIDA Research Monograph, Washington, D.C., 1990.
(18.) O'Malley, S., Adamse, M., Heaton, R. K., and Gawin, F. H., Neuropsychological impairment in chronic cocaine abusers, Am. J. Drug Alcohol Abuse 18(2):131-144 (1992).
(19.) Smith, S. E., and Meldrum, B. S., Cerebroprotective effect of lamotrigine after focal ischemia in rats, Stroke 26(1):117-121 (1995).
(20.) Wiard, R. P., Dickerson, M. C., Beek, O., Norton, R., and Cooper, B. R., Neuroprotective properties of the novel antiepileptic lamotrigine in a gerbil model of global cerebral ischemia, Stroke 26(3):466-472 (1995).
(21.) McGreer, E. G., and Zhu, S. G., Lamotrigine protects against kainate but not ibotenate lesions in rat striatum, Neuroscience Letter 112:348-351 (1990).
(22.) Freed, W. J., Glutamatergic mechanisms mediating stimulant and antipsychotic drug effects, Neurosci. and Biobehav. Rev. 18(1):111-120 (1994).
(23.) Moghaddam, R., and M. L. B., Glutamatergic antagonists attenuate ability of dopamine uptake blockers to increase extracellular levels of dopamine: Implications for tonic influence of glutamate on dopamine release, Synapse 18:337-342 (1994).
(24.) Pap, A., and Bradberry, C. W., Excitatory amino acid antagonists attenuate the effects of cocaine on extracellular dopamine in the nucleus accumbens, J. Pharmacol. Exp. Ther. 274(1):127-133 (1995).
(25.) Pulvirenti, L., Sung, R., and Koob, G. F., Microinjection of NMDA but not quisqualate receptor antagonists into the nucleus accumbens modulates intravenous cocaine self-administration in rats, Soc. Neurosci. Abstr. 15:1098 (1989).
(26.) Kalivas, P. W., Interactions between dopamine and excitatory amino acids in behavioral sensitization to psychostimulants, Drug Alcohol Depend. 37:95-100 (1995).
(27.) Beitner-Johnson, D., and Nestler, E. J. (Eds.), Basic Neurobiology of Cocaine: Actions Within the Mesolimbic Dopamine System [Clinician's Guide to Cocaine Addiction], Guilford Press, New York, 1992.
(28.) Pakesch, G., Loimer, N., Grunberger, J., Pfersmann, D., Linzmayer, L., and Mayerhofer, S., Neuropsychological findings and psychiatric symptoms in HIV-1 infected and noninfected drug users, Psychiatry Res. 41:163-177 (1992).
(29.) McKegney, F. P., O'Dowd, M. A., Feiner, C., Selwyn, P., Drucker, E., and Friedland, G. H., A prospective comparison of neuropsychologic function in HIV-seropositive and seronegative methadone-maintained patients, AIDS 4:565-569 (1990).
(30.) Woods, S. W., O'Malley, S. S., Martini, B. L., McDougle, C. J., Price, L. H., Krystal, J. H., Hoffer, P. B., and Kosten, T. R., SPECT regional cerebral blood flow and neuropsychological testing in non-demented HIV-positive drug abusers, Prog. Neuropsychopharmacol. Bio. Psychiatry 15:649-662 (1991).
(31.) Barks, J. D. E., Sun, R., Malinak, C., and Silverstein, F. S., gp120, an HIV-1 protein, increases susceptibility to hypoglycemic and ischemic brain injury in perinatal rats, Exp. Neurol. 132:123-133 (1995).
(32.) Pellegrini, J. W., and Lipton, S. A., Delayed administration of memantine prevents N-methyl-D-aspartate receptor-mediated neurotoxicity. Ann. Neurol. 33:403-407 (1993).
(33.) Larrat, E. P., and Zierler, S., Entangled epidemics: Cocaine use and HIV disease, J. Psychoactive Drugs 25(3):207-220 (1993).
(34.) Camacho, L. M., Brown, B. S., and Simpson, D. D., Psychological dysfunction and HIV/ AIDS risk behavior, J. of Acquired Immune Deficiency Syndromes and Human Retrovirology 11(2):198-202 (1996).
(35.) Fagnou, D. D. T., J.M., The biochemistry of learning and memory, Mol. Cell. Biochem. 149-150:279-286 (1995).
(36.) Binnie, C. D., Cognitive impairment: Is it inevitable? Seizure 3(Supp A): 17-22 (1994).
(37.) Cohen, A. J., Ashby, L., Crowley, D., Land, G., Peck, A. W., and Miller, A. A., Lamotrigine (BW430C), a potential anticonvulsant. Effects on the central nervous system in comparison with phenytoin and diazepam, Br. J. Pharmacol. 20:619-629 (1985).
(38.) Hamilton, M. J., Cohen, A. F., and Yuen, A. W. C., Carbamazepine and lamotrigine in healthy volunteers: Relevance to early tolerance and clinical trial dosage, Epilepsia 34:166-173(1993).
(39.) Avants, S. K., Risk Reduction Therapy (RRT) for HIV-positive injection drug users, Unpublished treatment manual (1996).
(40.) First, M., Spitzer, R. L., Gibbon, M., and Williams, J., Structured Clinical Interview for DSM-IV Axis I Disorders--Patient Edition (SCID-I/P-Version 2.0), Biometrics Research Department, New York State Psychiatric Institute, 722 W. 168th Street, New York, NY 10032, 1996.
(41.) McLellan, A. T., Luborksy, L., Woody, G. E., and O'Brien, C. P., An improved diagnostic instrument for substance abuse patients: The Addiction Severity Index. J. Nerv. Ment. Dis. 168:26-33 (1980).
(42.) Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., and Erbaugh, J., An inventory for measuring depression, Arch. Gen. Psychiatry 4:561-571 (1961).
(43.) Spielberger, C. D., Gorsuch, R. L., and Lushene, R. E., The State-Trait Anxiety Inventory Test Manual, Consulting Psychologists Press, Palo Alto, California, 1970.
(44.) Wechsler, D., WAIS-R Manual, Psychological Corporation, New York, 1981.
(45.) Rey, A., L'examen Clinique en Psychologie, Presses Universitaires de France, Paris, 1964.
(46.) Russell, E. W., A multiple scoring method for the assessment of complex memory functions, J. Consult. Clin. Psychol. 43:800-809 (1975).
(47.) Gronwall, D. M. A., Paced auditory serial-addition task: A measure of recovery from concussion, Perceptual and Motor Skills 44:367-373 (1977).
(48.) Benton, A. L., and Hamsher, K., Multilingual Aphasia Examination, University of Iowa, Iowa City, 1976.
(49.) Army, Army Individual Test Battery. Manual of Directions and Scoring, War Department, Adjutant General's Office, Washington, D.C. 1994.
(50.) Poklis, A., Evaluation of Tdx cocaine metabolite assay, J. Anal. Toxicol. 11:228-230 (1987).
(51.) Pellock, J. M., The clinical efficacy of lamotrigine as an antiepileptic drug, Neurology 44(Suppl 8):829-835 (1994).
(52.) Mendelson, J. H., Holman, B. I., Teoh, S. W., Levin, J., and Mello, N. K., Buprenorphine treatment improves brain perfusion abnormalities in men with concurrent cocaine and heroin dependence: A SPECT brain imaging analysis, in Problems of Drug Dependence, 1994, Vol. 153 (L. Harris, Ed.), NIDA Research Monograph Series, Washington, D.C., 1995.
(53.) Calabrese, J. R., Faterni, S. H., and Woyshville, M. J., Antidepressant effects of lamotrigine in rapid cycling bipolar disorder, Am. J. Psychiatry 153:1236 (1996).
(54.) Mervaala, E., Koivisto, K., and Hanninen, T., Electrophysiological and neuropsychological profiles of lamotrigine in young and age-associated memory impairment subjects, Neurology 46(Suppl 4):A259 (1995).
(55.) Lezak, M., Neuropsychological Assessment, Oxford University Press, New York, 1983.
Arthur Margolin, Ph.D.(*) S. Kelly Avants, Ph.D. Dominick DePhilippis, Ph.D. Thomas R. Kosten, M.D.
Substance Abuse Center Department of Psychiatry Yale University School of Medicine New Haven, Connecticut
(*) To whom correspondence should be addressed at Substance Abuse Center, 34 Park St., New Haven, CT 06519.
COPYRIGHT 1998 Marcel Dekker, Inc.
COPYRIGHT 2001 Gale Group