Byline: B. Yadav, S. Sharma
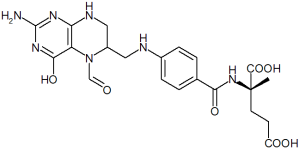
Fluorouracil is an analogue of fluorinated pyramidine commonly used in the treatment of several cancers. After rapid intravenous injection, fluorouracil rapidly diffuses into all body compartments, including the nervous system. The drug is primarily degraded by the liver. The toxicity of 5-FU is strongly influenced by the dosage used and the rate and duration of drug administration. Neurologic toxicity manifested by somnolence, confusion, seizures, cerebellar ataxia and rarely encephalopathy are known but uncommon. They are usually totally reversible on withdrawal of drug. Leucovorin which is commonly combined with 5-FU enhances the antitumor activity as well as toxicity.
Case report
A 49-year-old female, a known case of diabetes mellitus for 15 years, on insulin presented with complaint of lump left breast since April 2003 to the Radiotherapy outpatient department. She was treated for depression in 1997, but was doing well since then.
Her general physical examination was with in normal limits. Her local examination revealed that her left nipple was retracted and there was an 8x6 cm lump in the left breast which was hard, not fixed to underlying muscle or chest wall. The skin over the lump was normal. There was a 1x1 cm lymph node in the left axilla. Opposite breast and axilla were normal. Her abdominal and gynecological examinations were within normal limits.
Fine needle aspiration cytology (FNAC) from the lump revealed infiltrating ductal carcinoma. Her chest X-ray and ultrasound of abdomen and pelvis were normal. Her blood sugar was under control with insulin and other biochemical and hematological parameters were also normal. So she was diagnosed as Stage-III carcinoma breast.
Being a locally advanced case of carcinoma breast, she was started on neoadjuvant chemotherapy with FAC (5-fluorouracil, adriamycin and cyclophosphamide) regimen. The first cycle of chemotherapy was given on 3.5.03 at 2 pm. She developed generalized tonic clonic seizure at 11:30 pm on 3.5.03. She also had froathing and postictal incontinence.
On general physical examination she was disoriented to time, place and person. She was agitated, confused and had loss of both short as well as long term memory. Her behavior was altered and her talking was irrelevant. The pupils were reacting to light. The patient was sedated with iv diazepam. Neurological as well as psychiatric consultations were taken and she was also started on phenytoin.
On investigation her electrolytes, blood sugar, calcium, liver and kidney functions were within normal limits. Her ECG, chest X-ray, CT-scan brain both plain as well as contrast were also normal. On 4.5.03 at 7 am she was oriented but complained of loss of vision. Her electroencephalogram (EEG) and lipidogram were within normal limits. Her vision returned spontaneously on 5.5.03 at 6 am and her condition also improved and subsequently she was discharged on phenytoin.
She was given a second cycle of chemotherapy on 24.5.03 at 4 pm. She had similar symptoms again as on 3.5.03 and was managed with the same drugs. As no other cause could be found for her symptoms and the symptoms developed each time after chemotherapy, the 5-FU induced encephalopathy and convulsions were suspected; therefore 5-FU was omitted from next the course. She did not develop a similar problem after that and completed the rest of the chemotherapy without any problem.
Discussion
Many cases associated with high-dose infusion of 5-FU-induced encephalopathy have been reported in the literature.[1] To our knowledge this is the first case being reported to have been caused by bolus 5-FU (600 mg/m[2]. Neurotoxicity is a well known but rather rare adverse effect of 5-FU. In the literature its incidence ranges from 0.9% -7%.[2],[3] Yeh et al had reported among 280 patients who had received high dose 5-FU infusion and leucovorin (HDFL) between 1991 and 1995, 16 (5.7%) developed HDFL related encephalopathy. The incidence of this complication was 12.1% in gastric cancer, 4.3% in breast cancer and 2.4% in colorectal cancer.[4] Similarly Weh et al [5] reported 4 out of 64 cases of various gastrointestinal cancers treated weekly with folinic acid and high dose 5-FU infusion who developed clinically relevant neurotoxicity Koenig and Patel formulated the hypothesis that ammonia- the end product of 5-FU may be responsible for such clinical picture. ATP-dependent urea cycle normally clears this ammonia but fluoroacetate, the intermediate product of 5-FU, directly inhibits the ATP production in Kreb's cycle and results in lactic acidosis and impairment of the ATP depedent urea cycle. The end result is a transient hyperammonaemia state with encephalopathy.[6]
This clinical picture has been observed after 5-FU alone or in combination with allopurinol, folinic acid, thymidine and PALA (N-Phosphono Acetyl L-Aspartate).[7],[8],[9],[10],[11] But none of these agents were taken by this patient. The only risk factor in this patient was that she had received treatment for depression in 1997 but was asymptomatic since then.
The patient may present with encephalopathy, including confusion, agitation, reversible somnolence, euphoria, transient blindness, neurosensory hearing impairment, cerebellar ataxia, nystagmus, headache, lethargy, seizure, stupor and deep coma, even death has been reported in a case series [4] .
Diagnostic criteria include 1) development of encephalopathy during or shortly after completion of 5-FU therapy. 2) exclusion of other metabolic or physical factors that may have an effect the level of consciousness, such as hyperglycemia, hypoglycemia, azotemia, hepatic failure, electrolyte imbalance, sepsis and brain metastasis and 3) exclusion of drug effect by concomitant medications [4] .
Other differential diagnosis of 5-FU related toxicity such as familial deficiency of dihydropyrimidine dehydrogenase (DPD), the primary inactivating enzyme of 5-FU, should be ruled out. Malnutrition and thiamine deficiencies have also been seen to contribute to this syndrome. 5-FU exacerbates the pre-existing thiamine deficiency by blocking conversion of thiamine to active thiamine pyrophosphate. Hepatic, renal, nutritional and other metabolic causes were not seen in this patient.
Thus it can be concluded that encephalopathy, although rare, is an important complication due to 5-FU and should not be forgotten when the patient is being treated with this chemotherapeutic agent, alone or in combination with other drugs. It is a transient phenomenon and recovery is complete, but the patient should be managed symptomatically and supportive care should be provided to avoid complications related to unconscious state and convulsions.
References
1. Ardalan B, Chua L, Tian EM, Reddy R, Sridhar K, Benedetto P, et al . A phase II study of weekly 24-hour infusion with high-dose fluorouracil with leucovorin in colorectal carcinoma. J Clin Oncol 1991;9:625-30.
2. Weiss HD, Walker MD, Wiernik PH. Neurotoxicity of commonly used antineoplastic agents (first of two parts). N Engl J Med 1974;291:75-81.
3. Kaplan RS, Wiernik PH. Neurotoxocity of antineoplastic drugs. Sem Oncol 1982;9:103-30.
4. Yeh KH, Cheng AL. High-dose 5-fluorouracil infusional therapy is associated with hyperammonaemia, lactic acidosis and encephalopathy. Brit J Cancer 1997;75:464-5.
5. Weh HJ, Bittner S, Hoffknecht M, Hossfeld DK. Neurotoxicity following weekly therapy with folinic acid and high-dose 5-fluorouracil 24-h infusion in patients with gastrointestinal malignancies. Eur J Cancer 1993;29A:1218-9.
6. Koenig H, Patel A. Biochemical basis for fluorouracil neurotoxicity. The role of Krebs cycle inhibition by fluoroacetate. Arch Neurol 1970;23:155-60.
7. Kroener JF, Saleh F, Anderson RE, Howell SB. 5-fluorouracil and allopurinol: Toxicity modulation and phase II results in colon cancer. Proc Am Assoc Cancer Res 1981;22:459.
8. Tsavaris N, Bacoyannis C, Milonakis N, Sarafidou M, Zamanis N, Magoulas D, et al . Folinic acid plus high-dose 5-fluorouracil with allopurinol protection in the treatment of advanced colorectal carcinoma. Eur J Cancer 1990;26:1054-6.
9. Laufman LR, Krzeczowaski KA, Roach R, Segal M. Leucovorin plus 5-fluorouracil: an effective treatment of metastatic colon cancer. J Clin Oncol 1987;5:1394-400.
10. Buroker TR, Moertel CG, Fleming TR, Everson LK, Cullinan SA, Krook JE, et al . A controlled evaluation of recent approaches to biochemical modulation or enhancement of 5-fluorouracil therapy in colorectal carcinoma. J Clin Oncol. 1985;3:1624-31.
11. O'Dwyer PJ, Paul AR, Walczak J, Weiner LM, Litwin S, Comis RL. Phase II study of biochemical modulation of fluorouracil by low dose PALA in patients with colorectal cancer. J Clin Oncol 1990;8:1497-503.
COPYRIGHT 2005 Medknow Publications
COPYRIGHT 2005 Gale Group