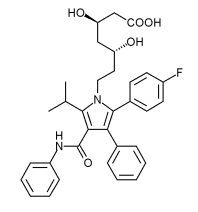
The findings were considered to be so important that The New England Journal of Medicine made the study freely available on its Web site one month earlier than the April 8 publication date. Two cholesterol-lowering statin drugs--Lipitor (atorvastatin) and Pravachol (pravastatin)--were compared in a clinical trial that involved 4,162 people who had been hospitalized for a sudden attack of chest pain due to heart disease. Lipitor proved to be more effective at reducing the rate of deaths from heart disease, heart-related problems and the need for procedures, such as bypass surgery and angioplasty. Once the news caught media attention, the reporting made the benefit appear larger than it is.
Some of the participants, all of whom had heart disease and low levels of LDL, the so-called bad cholesterol, benefited from even further reductions in their LDL with Lipitor. The finding is widely expected to lead to a lowering of what constitutes the ideal level of LDL. Currently, people are told to keep their LDL below 100 mg.
The participants had been randomly assigned to take either a higher than normal dose of Lipitor (80 mg) or the standard 40 mg dose of Pravachol each day. Because of the high stakes, drug companies rarely pit their drug against a competitor in a clinical trial. Bristol-Myers Squibb, maker of Pravachol, lost big time by sponsoring this trial. It was designed to prove that Pravachol, which had been losing market share, is just as good as the more costly high dose Lipitor.
At the time this trial was planned, Pravachol's highest dose was 40 mg. The study is known by the catchy name of Prove It, or Pravastatin or Atorvastatin Evaluation and Infection Therapy.
Here are the differences in outcomes in the Prove It trial: After two years, the people on Pravachol had a combined rate of heart attack, bypass surgery, angioplasty, stroke and death of 26.3% compared with 22.4% for people on Lipitor. The death rate from heart disease was 1.1% for the Lipitor group compared to 1.4% for the Pravachol group. The rate of death from any cause was 2.2% for people on Lipitor and 3.2% for people on Pravachol.
These 1- 3% differences in favor of Lipitor have cardiologists across the country quite excited and ready to raise the statin dose and lower the threshold for safe LDL levels. The Prove It results would be exciting if we had the full picture on high-dose Lipitor. As is often the case, the serious adverse effects experienced by the study participants taking Lipitor were not reported.
Christopher P. Cannon, MD, who led the Prove It trial, was asked about this information gap. "We do plan a separate full publication of all the safety data soon...the journal only allows a certain amount of space for only one paper," he responded by e-mail. "There were more liver function test abnormalities with Lipitor at 80 mg, but these were all transient and were resolved when the dose was stopped or reduced." Still, adverse reactions caused nearly one out of every three participants to stop the drug. 3% more people in the Lipitor group stopped taking the drug. Besides liver failure, muscle pain is a known consequence of high-dose statin therapy.
Dr. Cannon said that his study found Lipitor to be better than Pravachol for both men and women, though women represented only 22% of the participants (911). The above-quoted statistics apply to all participants, and the researcher did not break things down to show how large the benefits are to women, or whether they have a higher rate of serious adverse reactions.
90% of participants were white and the rest were not specified. This leaves an information gap for everyone else. Earlier studies have shown that Asians, for example, are at a higher risk for severe muscle damage if they take any statin at daily doses of 80 mg. For unknown reasons, the drug tends to remain in the body longer in Asians, which raises their odds of this and other adverse effects. Dr. Cannon and colleagues suggest that their findings point to the need for 62 mg as the new LDL threshold for people with "established coronary heart disease."
Judging from the media reports of Prove It trial, many cardiologists seem poised to extend its results to people without heart disease. None of the physicians quoted in the media warned that this would amount to a dangerous experiment. In all the previous clinical trials that involved people without heart disease, statin drugs were administered in doses no higher than 40 mg. Only one prevention trial involved people taking Lipitor. None lasted more than seven years.
Interestingly, the new results have revived an old controversy about whether the benefits of statins are due to their cholesterol lowering, anti-inflammatory or some other effects. "Unfortunately, we do not know the precise mechanism of action responsible for atorvastatin's [Lipitor's] superiority," wrote Eric J. Topol, MD, of the Cleveland Clinic in an accompanying editorial. Dr. Topol believes that "only a fraction of the patients who should be treated with a statin are actually receiving such therapy." He sees cost as the biggest stumbling block. Lipitor, at the recommended starting dose of 10 mg, is about $900 per year. At the 80-mg dose used in the Prove It trial, Lipitor costs about $1,400 per year.
What you can do
Here are several non-drug ways to reduce your odds of having a heart attack.
-Cut trans fatty acids from your diet because they have long been known to be damaging to the heart. Trans fatty acids are formed during the hydrogenation of either vegetable or fish oils. They are used extensively in processed foods to ensure a longer shelf life. Certain foods like donuts, potato chips and other snack foods are particularly high in trans fatty acids. Look for the words "partially hydrogenated oil" or "shortening" on the ingredients list.
-Take niacin supplements. The Coronary Drug Project followed 3,908 men taking a placebo or niacin therapy for nine years. The niacin group had a lower rate of nonfatal heart attacks and an 11% lower rate of all-cause mortality than the men in the placebo group. A recent survey of the various types of niacin on the market found that immediate-release niacin is the least expensive and safest version to purchase (and the no-flush niacin products are useless, see HealthFacts January 2004).
-Add heart healthy foods with omega-3 fatty acids and folic acid to your diet. Omega-3 fats can be found in fish, omega-3-enriched eggs, walnuts and flax seeds. Folic acid is in green vegetables, beans, wheat germ and certain fruits and vegetables.
COPYRIGHT 2004 Center for Medical Consumers, Inc.
COPYRIGHT 2004 Gale Group