Definition
Tricyclic antidepressants are medicines that relieve mental depression.
Purpose
Since their discovery in the 1950s, tricyclic antidepressants have been used to treat mental depression. Like other antidepressant drugs, they reduce symptoms such as extreme sadness, hopelessness, and lack of energy. Some tricyclic antidepressants are also used to treat bulimia, cocaine withdrawal, panic disorder, obsessive-compulsive disorders, certain types of chronic pain, and bed-wetting in children.
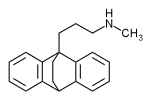
Description
Named for their three-ring chemical structure, tricyclic antidepressants work by correcting chemical imbalances in the brain. But because they also affect other chemicals throughout the body, these drugs may produce many unwanted side effects.
Tricyclic antidepressants are available only with a physician's prescription and are sold in tablet, capsule, liquid, and injectable forms. Some commonly used tricyclic antidepressants are amitriptyline (Elavil), desipramine (Norpramin), imipramine (Tofranil), nortriptyline (Pamelor), and protriptyline (Vivactil). Different drugs in this family have different effects, and physicians can choose the drug that best fits the patient's symptoms. For example, a physician might prescribe Elavil for a person with depression who has trouble sleeping, because this drug is more likely to make people feel calm and sleepy. Other tricyclic antidepressants might be more appropriate for depressed people with low energy.
Recommended dosage
The recommended dosage depends on many factors, including the patient's age, weight, general health and symptoms. The type of tricyclic antidepressant and its strength also must be considered. Check with the physician who prescribed the drug or the pharmacist who filled the prescription for the correct dosage.
Always take tricyclic antidepressants exactly as directed. Never take larger or more frequent doses, and do not take the drug for longer than directed. Do not stop taking the medicine just because it does not seem to be working. Several weeks may be needed for its effects to be felt. Visit the physician as often as recommended so that the physician can check to see if the drug is working and to note for side effects.
Do not stop taking this medicine suddenly after taking it for several weeks or more. Gradually tapering the dose may be necessary to reduce the chance of withdrawal symptoms.
Taking this medicine with food may prevent upset stomach.
Precautions
The effects of this medicine may continue for 3-7 days after patients stop taking it. All precautions should be observed during this period, as well as throughout treatment with tricyclic antidepressants.
Some people feel drowsy, dizzy, or lightheaded, when taking these drugs. The drugs may also cause blurred vision. Anyone who takes these drugs should not drive, use machines or do anything else that might be dangerous until they have found out how the drugs affect them.
Because tricyclic antidepressants work on the central nervous system, they may add to the effects of alcohol and other drugs that cause drowsiness, such as antihistamines, cold medicine, allergy medicine, sleep aids, medicine for seizures, tranquilizers, some pain relievers, and muscle relaxants. Anyone taking tricyclic antidepressants should check with his or her physician before drinking alcohol or taking any drugs that cause drowsiness.
These medicines make some people feel lightheaded, dizzy, or faint when they get up after sitting or lying down. To lessen the problem, get up gradually and hold onto something for support if possible.
Tricyclic antidepressants may interact with medicines used during surgery, dental procedures, or emergency treatment. These interactions could increase the chance of side effects. Anyone who is taking tricyclic antidepressants should be sure to tell the health care professional in charge before having any surgical or dental procedures or receiving emergency treatment.
These drugs may also change the results of medical tests. Before having medical tests, anyone taking this medicine should alert the health care professional in charge.
This medicine may increase sensitivity to sunlight. Even brief exposure to sun can cause a severe sunburn or a rash. While being treated with this tricyclic antidepressants, avoid being in direct sunlight, especially between 10 a.m. and 3 p.m.; wear a hat and tightly woven clothing that covers the arms and legs; use a sunscreen with a skin protection factor (SPF) of at least 15; protect the lips with a sun block lipstick; and do not use tanning beds, tanning booths, or sunlamps.
Tricyclic antidepressants may cause dry mouth. To temporarily relieve the discomfort, chew sugarless gum, suck on sugarless candy or ice chips, or use saliva substitutes, which come in liquid and tablet forms and are available without a prescription.
Children and older people are especially sensitive to the effects of tricyclic antidepressants. This increased sensitivity may increase the chance of side effects.
Special conditions
People with certain medical conditions or who are taking certain other medicines can have problems if they take tricyclic antidepressants. Before taking these drugs, be sure to let the physician know about any of these conditions:
Allergies
Anyone who has had unusual reactions to tricyclic antidepressants or to carbamazepine (Tegretol), maprotiline (Ludiomil), or trazodone (Desyrel) in the past should let his or her physician know before taking tricyclic antidepressants. The physician should also be told about any allergies to foods, dyes, preservatives, or other substances.
Pregnancy
Problems have been reported in babies whose mothers took tricyclic antidepressants just before delivery. Women who are pregnant or who may become pregnant should check with their physicians about the safety of using tricyclic antidepressants.
Breastfeeding
Tricyclic antidepressants pass into breast milk and may cause drowsiness in nursing babies whose mothers take the drugs. Women who are breastfeeding should check with their physicians before using tricyclic antidepressants.
Diabetes
Tricyclic antidepressants may affect blood sugar levels. Diabetic patients who notice changes in blood or urine test results while taking this medicine should check with their physicians.
Other medical conditions
Before using tricyclic antidepressants, people with any of these medical problems should make sure their physicians are aware of their conditions:
- Current or past alcohol or drug abuse
- Bipolar disorder (manic-depressive illness)
- Schizophrenia
- Seizures (convulsions)
- Heart disease
- High blood pressure
- Kidney disease
- Liver disease
- Overactive thyroid
- Stomach or intestinal problems
- Enlarged prostate
- Problems urinating
- Glaucoma
- Asthma.
Use of certain medicines
Taking tricyclic antidepressants with certain other drugs may affect the way the drugs work or may increase the chance of side effects.
Side effects
The most common side effects are dizziness, drowsiness, dry mouth, unpleasant taste, headache, nausea, mild tiredness or weakness, increased appetite or craving for sweets, and weight gain. These problems usually go away as the body adjusts to the drug and do not require medical treatment. Less common side effects, such as diarrhea, vomiting, sleep problems, sweating, and heartburn also may occur and do not need medical attention unless they do not go away or they interfere with normal activities.
More serious side effects are not common, but may occur. If any of the following side effects occur, check with the physician who prescribed the medicine as soon as possible:
- Blurred vision
- Eye pain
- Confusion
- Hallucinations
- Fainting
- Loss of balance
- Swallowing problems
- Difficulty speaking
- Mask-like face
- Shakiness or trembling
- Nervousness or restlessness
- Movement problems, such as shuffling walk, stiff arms and legs, or slow movement
- Decreased sexual ability
- Fast or irregular heartbeat
- Constipation
- Problems urinating.
Some side effects may continue after treatment with tricyclic antidepressants has ended. Check with a physician if these symptoms occur:
- Headache
- Nausea, vomiting, or diarrhea
- Sleep problems, including vivid dreams
- Unusual excitement, restlessness, or irritability.
Interactions
Life-threatening reactions, such as extrememly high blood pressure, may occur when tricyclic antidepressants are taken with other antidepressants called monoamine oxidase (MAO) inhibitors (such as Nardil and Parnate). Do not take tricyclic antidepressants within 2 weeks of taking a MAO inhibitor. However, a patient can take an MAO inhibitor immediately after tricyclic antidepressant therapy is stopped by the physician.
Tricyclic antidepressants may interact with many other medicines. When this happens, the effects of one or both of the drugs may change or the risk of side effects may be greater. Anyone who takes tricyclic antidepressants should let the physician know all other medicines he or she is taking. Among the drugs that may interact with tricyclic antidepressants are:
- Central nervous system (CNS) depressants such as medicine for allergies, colds, hay fever, and asthma; sedatives; tranquilizers; prescription pain medicine; muscle relaxants; medicine for seizures; sleep aids; barbiturates; and anesthetics.
- Diet pills
- Amphetamines
- Blood thinning drugs
- Medicine for overactive thyroid
- Cimetidine (Tagamet)
- Other antidepressant drugs, including MAO inhibitors (such as Nardil and Parnate) and antidepressants that raise serotonin levels (such as Prozac and Zoloft)
- Blood pressure medicines such as clonidine (Catapres) and guanethidine monosulfate (Ismelin)
- Disulfiram (Antabuse), used to treat alcohol abuse
- Major tranquilizers such as thioridazine (Mellaril) and chlorpromazine (Thorazine)
- Antianxiety drugs such as chlordiazepoxide (Librium) and alprazolam (Xanax)
- Antiseizure medicines such as carbamazaepine (Tegretol) and phenytoin (Dilantin).
The list above does not include every drug that may interact with tricyclic antidepressants. Be sure to check with a physician or pharmacist before combining tricyclic antidepressants with any other prescription or nonprescription (over-the-counter) medicine.
Key Terms
- Asthma
- A disease in which the air passages of the lungs become inflamed and narrowed.
- Bulimia
- An eating disorder in which a person binges on food and then induces vomiting, uses laxatives, or goes without food for some time.
- Chronic
- A word used to describe a long-lasting condition. Chronic conditions often develop gradually and involve slow changes.
- Delusion
- An abnormal mental state characterized by the acceptance of something as true that is actually false or unreal, such as the belief that one is Jesus Christ.
- Depression
- A mental condition in which a person feels extremely sad and loses interest in life. A person with depression may also have sleep problems and loss of appetite and may have trouble concentrating and carrying out everyday activities.
- Glaucoma
- A condition in which pressure in the eye is abnormally high. If not treated, glaucoma may lead to blindness.
- Hallucination
- A false or distorted perception of objects, sounds, or events that seems real. Hallucinations usually result from drugs or mental disorders.
- Obsessive-compulsive disorder
- An anxiety disorder in which a person cannot prevent himself from dwelling on unwanted thoughts, acting on urges, or performing repetitious rituals, such as washing his hands or checking to make sure he turned off the lights.
- Panic disorder
- An disorder in which a person has sudden and intense attacks of anxiety in certain situations. Symptoms such as shortness of breath, sweating, dizziness, chest pain, and extreme fear often accompany the attacks.
- Prostate
- A donut-shaped gland in males below the bladder that contributes to the production of semen.
- Schizophrenia
- A severe mental disorder in which a person loses touch with reality and may have illogical thoughts, delusions, hallucinations, behavioral problems and other disturbances.
- Seizure
- A sudden attack, spasm, or convulsion.
- Serotonin
- A natural chemical found in the brain and other parts of the body, that carries signals between nerve cells.
- Withdrawal symptoms
- A group of physical or mental symptoms that may occur when a person suddenly stops using a drug to which he or she has become dependent.
Further Reading
Gale Encyclopedia of Medicine. Gale Research, 1999.