Approximately 282,000 adults, adolescents, and children are currently living with human immunodeficiency virus (HIV) infection or acquired immunodeficiency syndrome (AIDS) in the United States as of the year 2002.1 With the advent of highly active antiretroviral therapy (HAART), the life span of these individuals has dramatically increased,2 and HIV infection is now considered a chronic illness with accompanying episodes of exacerbations and remissions of symptoms.3 Numerous conditions such as lipodystrophy syndrome4-6 and skeletal myopathy7-9 have been associated with HIV and its medical management, many of which may result in physical disability and diminished quality of life. Due to the chronic nature of this condition, physical therapists will continue to manage many of these conditions in increased numbers of people who are living with HIV. Although guidelines for physical therapy evaluation and management of this potentially disabling condition have not been established, it appears that aerobic exercise training may have a beneficial effect on the cardiorespiratory health of people who are living with HIV. Thus, an understanding of the factors that limit the oxidative metabolic response to physical activity is paramount in developing effective exercise training programs for people with this virus. The focus of this Update is to examine the biological factors that might limit the oxidative metabolic response to physical activity in people with HIV.
[Cade WT, Peralta L, Keyser RE. Aerobic exercise dysfunction in human immunodeficiency virus: a potential link to physical disability. Phys Ther. 2004;84:655-664.]
Key Words: Antiretroviral therapy, Disability, Physical activity.
Features of Fatigue and Physical Disability
HIV-related disability has been associated with fatigue and decreased physical functioning10-13 as well as other factors that may limit people's ability to carry out necessary life activities.12,14,15 Fatigue in adults with HIV has been identified using patient self-reports of physical and functional limitations while performing activities of daily living such as housework, climbing stairs, and walking15 and activities required for employment.10,11 Asymptomatic HIV infection is defined as having no symptoms or as having symptoms related only to acute primary HIV infection, such as persistent generalized lymphadenopathy (swollen and firm lymph glands).11 Thirty-one percent of men and 53% of women with asymptomatic HIV infection have reported at least one limitation to physical activity as a result of fatigue.11 Among those with symptomatic HIV infection, defined as having a condition such as thrush (a fungal infection of the mouth, throat, and tongue) or having diarrhea or a fever longer than 1 month, who reported fatigue, 52.6% of men and 62.3% of women reported at least one or more limitations to physical activity resulting from fatigue.11 Seventy percent of men and 80% of women with AIDS reporting fatigue also were found to have at least one functional limitation resulting from fatigue.11 Moreover, approximately half the adults with HIV who reported fatigue in this particular study also reported a chronic inability to participate in other life activities, such as attending school or working at a job.11 Recreational activities that involve strenuous activity such as running, cycling, or hiking16 have been thought to be further limited in this population.17,18
Exercise and Activity Intolerance
The aerobic or oxidative system provides energy (adenosine triphosphate [ATP]) to working muscles during physical activity through the oxidation of glucose, fatty acids, and amino acids in the mitochondria.19 According to the Pick equation, the total volume of oxygen consumed (V(dot above)O^sub 2^), the primary measure of oxidative capacity, equals the product of oxygen delivery to the working muscles (cardiac output) and the ability of the muscle to extract and utilize the oxygen to produce energy (arteriovenous oxygen difference).19 Disruption of any part of the pathway-from pulmonary extraction of atmospheric oxygen to mitochondrial uptake and utilization, including inhalation into the lungs, diffusion from the alveoli to the lung capillaries, blood transport by the heart and circulatory system to the working muscles, diffusion across the capillaries into the muscle cell, and movement across the cell and into the mitochondriawould impair oxidative metabolism.
Instrumental activities of daily living include tasks such as housework, meal preparation, grocery shopping, and light lawn work; these activities have energy requirements of between 3 and 5 metabolic equivalents (METs).20 One MET equals the average resting metabolic rate in the general population: 3.5 mL of oxygen consumed per kilogram of body weight per minute. Physical activity lasting over a minute requires the presence and use of oxygen, or aerobic respiration, to liberate energy.21 When activity is sustained at a high oxygen demand, the slow responsiveness of the oxidative system requires that the source of energy must be supplemented by a metabolic pathway that does not require oxygen: the glycolytic pathway. While the nonoxidative glycolytic pathway provides a small amount of energy supplement rapidly, among its by-products are hydrogen ions and lactic acid. These by-products tend to lower intracellular pH, and higher concentrations of these substances are associated with fatigue.22 Thus, in order for an individual to tolerate a particular intensity of physical activity without becoming fatigued, the effectiveness of the oxidative metabolic pathway must be high enough to meet the energy demand with minimal nonoxidative supplementation. Aerobic insufficiency, defined as aerobic capacity that is insufficient for meeting required energy demands, results in physical activity intolerance23 and may result in functional limitations placed on performance of daily activities and in physical disability. Age normative values for peak aerobic capacity, measured by indirect calorimetry during exercise testing, for sedentary men and women with no known pathology or impairments in the 50th percentile ranges16 are reported in the Table.
Diminished aerobic capacity in both adolescents and adults with HIV appears to be one mechanism of fatigue and physical disability.17,18,24 Diminished peak V(dot above)O^sub 2^ has been identified among adults with HIV25-28 and ranges approximately 15% to 40% below that predicted for sedentary age-matched controls without HIV.17,18,25,26,28 Functional aerobic impairment, defined as peak V(dot above)O^sub 2^ of > or =27% below predicted values for age, sex, and physical activity level, was found in both adolescents17 and adults24 who had asymptomatic to mildly symptomatic HIV infection.
Ventilatory threshold, a physiological marker of the onset of fatigue, was found to occur earlier during maximal exercise tests25,27 in people with HIV than in people without HIV.21 Ventilatory threshold occurs at a point during a progressive physical activity load where expired carbon dioxide (V(dot above)CO^sub 2^) and minute ventilation begins to increase more rapidly than V(dot above)O^sub 2^.29 This increase in expired V(dot above)CO^sub 2^ has been associated with increases in blood lactate and hydrogen ions and results from pulmonary buffering of these metabolites due to an increased need for glycolytic metabolic supplementation.21 If the oxidative system is inadequate (ie, during pathology) to meet the energy requirements of a particular activity, the glycolytic system will increase its contribution in order to meet the energy needs and the Ventilatory threshold, and thus the onset of fatigue will occur at a lower intensity of activity. Ventilatory threshold has been shown to occur during the energy requirements associated with light instrumental activities of daily living (3.0-4.0 METs [10.5-14.0 mL.kg^sup -1^.mk^sup -1^]) in adolescents with HIV.17 In combination with the finding of low peak V(dot above)O^sub 2^, this report suggested that adolescents with HIV may not have had the ability to sustain some activities of daily living or to perform recreational or occupational activities at even slightly higher energy requirements.17 Indexes of aerobic impairment and oxidative metabolic dysfunction might provide quantitative evidence for fatigue-related disability in adolescents and adults with HIV.
Potential Mechanisms for Exercise and Physical Activity Intolerance
Muscle Dysfunction
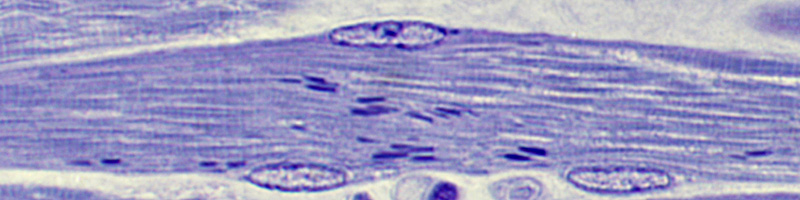
Several possible mechanisms for exercise and activity dysfunction in people with HIV have been reported. Structural and inflammatory muscle abnormalities in people with HIV, which may impair the muscle's ability to extract or utilize oxygen during exercise, have been widely reported. HIV infection-mediated myopathy, as identified by the presence of necrosis (cell death), nemaline rod bodies (rod-shaped inclusion bodies consisting of alpha-actinin and desmin), inflammation, and vasculitis (inflammation uf microvasculature) were found in 26% of individuals infected with HIV who either had never taken antiretroviral therapy or had a low lifetime dose, indicating a deleterious effect of HIV infection on skeletal muscle.30 Mitochondrial abnormalities also were found in people with HIV who had neve: taken HAART, including abnormal size, shape, and cristac (inner and outer mitochondrial membrane) structure.31 Cytokine expression (ie, interleukin-1 and tumor necrosis factor-[alpha]) and macrophages were detected in muscle, indicating proteolysis and inflammation, in 5 individuals with HIV and known polymyositis or wasting syndrome.32 Although there has not been strong evidence for direct HIV infection of skeletal muscle, antigens have been identified in macrophages invading the muscle, implicating inflammation33,34 as a potential mediator of muscle tissue infection by the virus. Clinical manifestations of HIV-associated myopathy have been reported to include proximal weakness, myalgia, abnormal electromyographic activity, elevated creatine kinase, and diminished physical functioning of the muscle.7-9
Medical management of HIV includes a combination of antiretroviral drugs aimed at stopping the replication of the virus and restoring and preserving immune function. Initial therapy recommendations for both people with asymptomatic HIV infection and those with advanced HIV disease include at least one nucleoside analog reverse transcriptase inhibitor (ie, stavudine, didanosine), a protease inhibitor (ie, ritonovir, indinavir), or a non-nucleoside reverse transcriptase inhibitor (ie, efavirenz). Intervention considerations include the quantity of the plasma viral burden, immunological function (ie, CD4 count), known antiretroviral drug resistance genotypes, adherence, and potential drug toxicities.35 Nucleoside analogs were first introduced in the late 1980s, followed by the introduction of other components of HAART (non-nucleoside reverse transcriptase inhibitors and protease inhibitors) in the 1990s. Therefore, physiological complications associated with HIV and their interventions appear to have changed since the initial advent of the disease.
Substantial evidence for the mediating role of nucleoside analog therapy with respect to mitochondrial dysfunction has been presented. Nucleoside analogmediated inhibition of HIV replication occurs by substitution of the phosphorylated drug into the DNA in place of deoxythymidine triphosphate (dTTP). This alteration results in termination of the elongating DNA chain, which, in turn, blocks reverse transcription. A similar action of nucleoside analogs on the mitochondrial transcription enzyme, DNA polymerase [gamma], and mitochondrial DNA (mtDNA) chain terminators has been proposed as a mechanism of mitochondrial dysfunction.36-39 Mitochondrial abnormalities secondary to the effects of nucleoside analog therapy have been found in both human and animal studies. The mitochondrial enzyme, cytochrome-c oxidase, which is essential in ATP production via oxidative phosphorylation, has been found to be deficient in both in vitro and in vivo muscle treated with a nucleoside analog.40-43 Numerous other nucleoside analog-induced mitochondrial alterations also have been identified, including oxidative damage to and decreases in mtDNA44-49; decreased mitochondrial RNA (mtRNA)50; ultrastructural damage to mitochondria (eg, swelling, cristae disruption, inclusion-body presence )31,50-52; presence of mitochondrial-bound interleukin-la in zidovudine-treated muscle fibers32; inhibition of both NADH-linked respiration and NADH-reductase activity53; and a diminished aerobic training response of cytochrome-c oxidase by means of chronic electrical stimulation.54 These abnormalities were further evidenced by the presence of lactic acidosis, which has frequently been found in people with HIV who were receiving nucleoside analog therapy.55-57 Other reported nucleoside analogmediated muscle abnormalities have included diminished muscle cell and myoblast (somite cells, which will develop into muscle cells) proliferation58; increased amounts of intramuscular lipid, glycogen, and lipofuscin (the pigment remaining after the breakdown and digestion of damaged blood cells)7; and ragged red and necrotic fibers (histological features that are associated with myopathy).59
Deleterious effects of nucleoside analog therapy may be seen during in vivo metabolism as well. A delayed recovery and larger depletion of phosphocreatine following muscular exercise were reported in a group that received nucleoside analog therapy as compared with a group that did not receive nucleoside analog therapy.60 A recent study61 further demonstrated decreased arteriovenous oxygen difference during peak treadmill exercise in a group of individuals with HIV who received HAART compared with a group of individuals with HIV who did not receive HAART and with a non-HIV-infected control group, indicating a deleterious effect of HAART on peak peripheral muscle oxygen extraction and utilization during exercise. This decrease in peripheral muscle extraction and utilization during exercise appears to reduce peak exercise capacity and would likely limit participation in many recreational activities for individuals with HIV who are receiving HAART. However, it also appears that HIV infection alone, apart from the effects of HAART, independently impairs oxygen on-kinetics (the speed with which the muscle is able to extract and utilize oxygen to create energy upon the initiation or change in the intensity of activity) during exercise intensities above the ventilatory threshold in both those receiving and not receiving HAART.10 How impaired oxygen on-kinetics affect activity tolerance is not yet clear, but early indications are that people with HIV appear to have a reduced ability to quickly obtain a steady state of oxidative metabolism for certain activities above the ventilatory threshold.
The effect of protease inhibitors on muscle function is unclear, but it appears that at least one protease inhibitor, indinavir, has a direct effect on glucose uptake. Indinavir has been shown to be inhibitory to the skeletal muscle glucose transporter, GLUT-4, in rats.63 If this inhibition also occurs in humans, it could potentially impair plasma glucose uptake and limit the amount of plasma glucose used for glycolysis and subsequent oxidation. This inhibition could potentially limit the amount of fuel that could be used for energy production during activity. An impairment of glucose transport also might reduce the amount of glycogen that could be stored in the skeletal muscle, thereby further limiting a potential substrate for energy production. The combination of these impairments would most likely be seen during higher-intensity activities such as sports and other recreational activities.
Cardiovascular Abnormalities
The prevalence of cardiac abnormalities in adults with HIV and AIDS has been reported to range between 28% and 73%.64 Greater longevity in patients with HFV and AIDS due to improved intervention has increased manifestations of late-stage cardiac disease.65 Cardiac diseases seen in people with HIV infection have included myocarditis, pericardial effusion, dilated cardiomyopathy, endocarditis, coronary artery disease, pulmonary hypertension, neoplasms, drug-related cardiomyopathy, and vascular lesions.65-67 Abnormalities have often been associated with infectious organisms such as Toxoplasma gondii, Mycobactmum tuberculosis, Crytococcus neoformans, and Candia albicans and the resulting inflammatory response.65 Autoantibodies to the myocardium68 as well as direct infection of cardiac muscle by HIV also have been reported in people with HIV.69,70 When compared with people with idiopathic cardiomyopathy, individuals with HIV-related cardiomyopathy had a lower likelihood of survival, indicating an independent relationship among HIV infection, cardiomyopathy, and greater mortality.71
Antiretroviial therapy, particularly the use of protease inhibitors, has been associated with abnormal lipid metabolism, including hyperglycemia, hypertriglyceridemia, hypercholesterolemia, glucose intolerance, insulin resistance, and abnormal fat distribution (ie, visceral adiposity and peripheral lipoatrophy).4-6,27-74 All of these conditions are known to increase the risk of cardiovascular disease.75,76 However, marked increased triglycerides in those with HIV also have been independently linked to HIV infection alone,72 indicating that HAART does not account for all of the risk. Protease inhibitors also have been associated with cardiac dysfunction via impaired diastolic function,77 myocardial infarction,78 and an increased risk of coronary artery disease through endothelial dysfunction.79
The effect of nucleoside analog medications on cardiac function among people with HIV also has been examined.80 It has been demonstrated that a child taking zidovudinc was 8.4 times more likely to develop cardiomyopathy than a child who was not taking the medication.80 Rats treated with zidovudine showed marked and widespread cardiac mitochondrial swelling with fractured and disrupted cristae and decreased mitochondrial cytochrome-b mRNA expression when compared with control animals.48 Overall, these cardiac abnormalities may impair left ventricular function, lower oxygen delivery to working musculature, and diminish exercise and activity tolerance.81 This reduction in cardiac pump function may lead to physical inactivity and peripheral muscle atrophy, potentially further limiting exercise and activity tolerance.
Although the majority of HIV-related cardiac dysfunction has been reported in patients with AIDS, recent reports64,65,82 have indicated that cardiac dysfunction may be seen subclinically (absence of overt clinical symptoms) in patients with asymptomatic and mildly symptomatic HIV infection. Subclinical findings suggest that the onset of cardiac abnormalities during the initial stages of HIV infection progresses with the disease and with susceptibility to opportunistic infections, as well as the potential cumulative effects of HAART. Subclinical cardiac abnormalities might combine with other complications of HIV infection, exacerbating fatigue and physical activity intolerance and resulting in functional limitations and physical disability.
The exercise dysfunction that accompanies HIV infection appears to have several characteristics in common with those seen in people with congestive heart failure. Individuals with congestive heart failure also demonstrate ventricular dysfunction and profound muscle dysfunction, specifically mitochondrial deficits, atrophy, and weakness, but further demonstrate respiratory muscle weakness and increased vascular resistance.83-85 Physical disability in people with congestive heart failure is well described and may provide insight into evaluation and management of physical function limitations in people with HIV.86
Anemia
The Centers for Disease Control and Prevention reported the 1-year incidence of anemia (hemoglobin
Deconditioning
Physiological deconditioning also may play a role in activity intolerance in people with HIV.101 Researchers in a number of aerobic exercise training studies of people with HIV have suggested that a training effect was achievable, reporting an increase in peak V(dot above)O^sub 2^ and ventilatory threshold and a decrease in resting submaximal heart rate.26,28,102 interpretation of these findings was that aerobic impairment in people with HIV maybe due only to deconditioning26,28,101 However, the finding of functional aerobic impairment in adolescents17 and adults24 with HIV indicated that aerobic capacity was limited far below that occurring as a result of physiologic deconditioning alone.17 Some authors18,24 concluded that it was likely that deconditioning played a part in aerobic insufficiency and activity intolerance in HIV infection, but that deconditioning alone could not have fully accounted for the severity of the limitation or the fatigue-mediated functional limitations associated with HIV infection. Numerous reports64-71,73 of cardiac dysfunction in individuals with HIV, especially those with symptomatic infection,64 make it unlikely that deconditioning alone accounts for the decreases in aerobic function. Furthermore, results from recent studies24,61 suggest that the exercising musculature's ability to extract and utilize oxygen accounts for peak aerobic exercise dysfunction in individuals with asymptomatic HIV infection and that HAART, rather than deconditioning alone, appears to limit peak aerobic capacity.
Smoking
Smoking may add to exercise and activity limitation by increasing carboxyhemoglobin content and subsequently reducing the oxygen-carrying content capacity in the blood. Carbon monoxide has been reported to compete with oxygen for binding sites on the hemoglobin molecule, thus reducing the amount of bound oxygen and subsequently the amount of oxygen delivered to the working muscles.101 Smoking has been reported to have a small, but significant, effect on peak V(dot above)O^sub 2^,103 but not all evidence supports smoking-mediated decreases in aerobic capacity.104 The percentages of smokers in exercise studies involving subjects with HIV ranged from 27% to 59%.25,26,28 Smoking may account for a small decrease in exercise capacity due to the high prevalence of smokers in previous, studies but it is not likely to have caused the large decreases in aerobic capacity seen in individuals with HIV.
Pulmonory Ventilation Limitations
Decreased total lung capacity, vital capacity, and other lung volumes have been seen in some subjects with AIDS and various pulmonary disorders, including Pneumocystis carinii pneumonia, Kaposi sarcoma, cytomegalovirus, and nonspecific pneumonia.105,106 There have been mixed findings in airflow rates (forced expiratory volume in 1 second [FEV^sub 1^] and forced vital capacity [FVC]) in people with AIDS.107-109 Diffusion capacity also has been reported to be lower in some people with HIV.106,110 study by Smith et al,111 severe exercise hypoxemia was found in 15 of 16 individuals with AIDS, with an average of 79% oxygen saturation as measured by pulse oximetry. Diminished gas transfer was further seen in subjects with HIV who had no history of respiratory disease when compared with controls.27 In contrast, Stringer101 found no evidence for ventilation/perfusion mismatching in 34 subjects with asymptomatic HIV infection. Furthermore, other investigators25,27 found resting FEV^sub 1^ and FVC to have been within 95% to 100% of predicted values in subjects with HIV who had no history or current evidence of pulmonary disease. Although no study to date has associated pulmonary ventilation limitations with reduced exercise capacity and activity intolerance in people with HIV, this association has been reported in other pathologies.112 Therefore, in people with HIV with acute or chronic respiratory disease, pulmonary limitations might contribute to exercise and activity intolerance; however, the majority of exercise dysfunction in people with HIV is most likely associated with other factors.
Miscellaneous
Other possible mechanisms that might be related to fatigue and associated physical limitations include decreased immunological function as indicated by decreases in CD4 counts,113 magnesium deficiencies,114 autoantibodies to acetylcholine receptors at the neuromuscular junction,115 low testosterone levels,116 nutritional deficiencies,116 cortisol abnormalities,117 depression,118 and sleep abnormalities, including increased levels of TNF-[alpha] at night, increased slow-wave sleep,10 altered delta-frequency sleep electroencephalogram patterns, and altered growth hormone secretion relationships.56
Implications for Rehabilitation
Exercise and activity intolerance in people with HIV has been manifested as decreased peak aerobic capacity, ventilatory threshold occurring during MET levels associated with instrumental activities of daily living, and prolonged oxygen on-kinetics. Decreased peak aerobic capacity in people with HIV indicates an impaired ability to participate in recreational activities that are associated with a high-energy requirement. A reduced ventilatory threshold in these individuals indicates that early anaerobic energy supplementation and the onset of fatigue may occur during activities of daily living such as housework, lawn care, and employment activities. These impairments may have important implications for physical disability in this population. Moreover, these impairments provide an opportunity for rehabilitation clinicians and researchers to address mechanisms and interventions for these limitations.
Evidence for an achievable aerobic training effect has been documented in the literature,26,28,102,119-122 suggesting a potential role for physical therapy in the management of this disorder. Increases in aerobic capacity have been reported as increased time on the treadmill during a maximal exercise test,119-121 increased peak V(dot above)O^sub 2^ (13%-24%),26,28,102,120 and increased ventilatory threshold (13%).26 Other beneficial effects of aerobic exercise training may include decreased body mass index, subcutaneous fat, and abdominal girth120 and reports of improved quality of life.26 Although reports of the effect of aerobic exercise on immune function in people with HIV are equivocal,26,28,119-122 it appears that aerobic exercise training does not adversely affect immunological function in people with HIV and is safe.122
These physiological adaptations to aerobic exercise training may improve fatigue, decrease functional limitations, and reduce physical disability resulting from HIV infection. It appears that performing constant or interval aerobic exercise for at least 20 minutes, at least 3 times per week for 4 weeks, may lead to improved cardiopulmonary fitness and improved psychological status, with an accompanying maintenance of immunological function.123 Among people with HIV who have known cardiovascular disease, pulmonary limitations, or muscle dysfunction, exercise prescription should be tailored to address the limitation, and the referring physician should determine any contraindications for exercise participation. Furthermore, as in people without HIV or AIDS,16 regular resistance training may improve muscle force and maintain lean body mass, especially in those with muscle wasting and unintended weight loss.124
Conclusions and Limitations
Aerobic exercise and activity dysfunction in individuals with HIV appears to be multifactorial, including detrimental inflammatory effects of the HIV virus as well as the pharmacological toxicity in skeletal and cardiac muscle. This oxidative dysfunction in HIV may be manifested as fatigue and physical functional limitations, and therefore physical disability, in both people with asymptomatic and symptomatic HIV infection. Impairments from HIV infection may now occur to a lesser extent from a better-controlled viral burden since the advent of HAART in the mid-1990s. However, the prevalence of impairments resulting from HAART itself may be increasing due to additions of the newer medications (ie, protease inhibitors). Moreover, people who have HIV infection are living longer, so the normal effects of aging also may result in physical disability in those with HIV. A limitation of this Update includes the lack of direct evidence for the link between physiological alterations and exercise and physical activity limitations in people with HIV. The complex nature of HIV disease also may influence interpretation of the pathophysiological and exercise limitation data in this population. Physical therapists can play an important role in diagnosis and management of aerobic insufficiency and the related physical dysfunction in people with HIV. Further studies are warranted on the specific role of aerobic dysfunction and disability in people with HIV infection.
References
1 HIV/AIDS Surveillance Report. Atlanta, Ga: Centers for Disease Control and Prevention; 2003;14:10.
2 Palella FJ Jr, Delaney KM, Moorman AC, et al (HIV Outpatient Study investigators). Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med. 1998;338(13):853-860.
3 Selwyn PA, Rivard M, Kappell D, et al. Palliative care for AIDS at a large urban leaching hospital: program description and preliminary outcomes. J Palliat Med. 2003;6:461-474.
4 Carr A, Samaras K, Chisholm DJ, Cooper DA. Abnormal fat distribution and use of prolease inhibitors, Lancet. 1998;351(9117):1736.
5 Walli R, Herfort O, Michl GM, et al. Treatment with protease inhibitors associated with peripheral insulin resistance and impaired oral glucose tolerance in HIV-1-infected patients. AIDS. 1998;12(15): F167-F173.
6 Behrens G, Dejam A, Schmidt H, et al. Impaired glucose tolerance, beta cell function and lipid metabolism in HIV patients under treatment with protease inhibitors. AIDS. 1999;13(10):F63-F70.
7 Cupler EJ, Danon MJ, Jay C, et al. Early features of zidovudine-associated myopathy: histopathological findings and clinical correlations. Acta Neuropathol. 1995;90:1-6.
8 Lane RJ, McLean KA, Moss J, Woodrow DF. Myopathy in HIV infection: the role of zidovudine and the significance of tubuloreticular inclusions. Neuropathol Appl Neurobiol. 1993;19:406-413.
9 Simpson DM, Citak KA, Godfrey E, et al. Myopathies associated with human immunodeficiency virus and zidovudine: can their effects be distinguished? Neurology. 1993;43:971-976.
10 Darko DF, McCutchan JA, Kripke DF, et al. Fatigue, sleep disturbance, disability, and indices of progression of HIV infection. Am J Psychiatry. 1992;149:514-520.
11 Sebasta D, Laplante MP. HIV/AIDS, Disability, and Employment. Disability Statistics Rehabilitation Research and Training Center, Institute for Health and Aging, University of California, San Francisco. Available at: http://dsc.ucsf.edu/reps/aids/index.html. Accessed July 20, 1999.
12 Crystal S, Fleishman JA, Hays RD, et al. Physical and role functioning among persons wilh HIV: results from a nationally representative survey. Med Care. 2000;38:1210-1223.
13 O'Dell MW, Meighen M, Riggs RV. Correlates of fatigue in HIV infection prior to AIDS: a pilot study. Disabil Rehabil. 1996;18:249-254.
14 Jelsma J, Mielke J, Powell G, et al. Disability in an urban black community in Zimbabwe. Disabil Rehabil. 2002;24:851-859.
15 O'Dell MW, Hubert HB, Lubeck DP, O'Driscoll P. Physical disability in a cohort of persons wilh AIDS: data from the AIDS Time-Oriented Health Outcome Study. AIDS. 1996;10:667-673.
16 American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 6th ed. Baltimore, Md: Lippincott, Williams & Wilkins; 2000.
17 Keyser RE, Peralta L, Cade WT, et al. Functional aerobic impairment in adolescents seropositive for HIV: a quasiexperimental analysis. Arch Phys Med Rehabil. 2000;81:1479-1484.
18 Cade WT, Peralta L, Keyser RE. Aerobic capacity in late adolescents infected with HIV and controls. Pediatr Rehabil. 2002;5:161-169.
19 Guyton AC, Hall JE. Textbook of Medical Physiology. 9th ed. Philadelphia, Pa: WB Saunders Co; 1996:1061-1062.
20 Gunn SM, Brooks AG, Withers RT, et al. Determining energy expenditure during some household and garden tasks. Med Sci Sports Exerc. 2002;34:895-902.
21 Brooks GA, Fahey TD, White TP, Baldwin KM. Exercise Physiology: Human Bioenergetics and Its Applications. 3rd ed. Mountain View, Calif: Mayfield Publishing Co; 2000.
22 Fitts RH. Cellular mechanisms of muscle fatigue. Physiol Rev. 1994; 74:49-94.
23 Ades PA, Savage PD, Tischler MD, et al. Determinants of disability in older coronary patients. Am Heart J. 2002;143:151-156.
24 Cade WT, Fantry LE, Nabar SR, Keyser RE. Decreased arteriovenous oxygen difference during treadmill testing in individuals infected with HIV. Arch Phys Med Reliabil. 2003;84:1595-1603.
25 Johnson JE, Anders GT, Blanton HM, et al. Exercise dysfunction in patients seropositive for the human immunodeficiency virus. Am Rev Respir Dis. 1990;141:618-622.
26 Stringer WW, Berezovskaya M, O'Brien WA, et al. The effect of exercise training on aerobic fitness, immune indices, and quality of life in HIV+ patients. Med Sci Sports Exerc. 1998;30:11-16.
27 Potholf G, Wassermann K, Ostmann H. Impairment of exercise capacity in various groups of HIV-infected patients. Respiration. 1994; 61:80-85.
28 Perna FM, LaPerriere A, Klimas N, et al. Cardiopulmonary and CD4 cell changes in response to exercise training in early symptomatic HIV infection. Med Sci Sports Exerc. 1999;31:973-979.
29 Feitosa MF, Gaskill SE, Rice T, et al. Major gene effects on exercise ventilatory threshold: the HERITAGE Family Study. J Appl Physiol. 2002;93:1000-1006.
30 Grau JM, Masanes F, Pedrol E, etal. Human immunodeficiency virus type 1 infection and myopathy: clinical relevance of zidovudine therapy. Ann Neural. 1993;34:206-211.
31 Morgello S, Wolfe D, Godfrey E, et al. Mitochondrial abnormalities in human immunodeficiency virus-associated myopathy. Acta Neuropathol. 1995;90:366-374.
32 Gherardi RK, Florea-Strat A, Fromont G, et al. Cytokine expression in the muscle of HIV-infected patients: evidence for interleukin-1 alpha accumulation in mitochondria of AZT fibers. Ann Neural. 1994:36:752-758.
33 Chad DA, Smith TW, Blumenfeld A, et al. Human immunodeficiency virus (HlV)-associated myopathy: immunocytochemical identification of an HIV antigen (gp 41) in muscle macrophages. Ann Neural. 1990;28:579-582.
34 Dalakas MG, Pezeshkpour GH, Gravell M, Sever JL. Polymyositis associated with AIDS retrovirus. JAMA 1986:256:2381-2383.
35 Dybul M, Fauci AS, Bartlett JG, et al. Guidelines for using antiretroviral agents among HIV-infected adults and adolescents: recommendations of the Panel on Clinical Practices for Treatment of HIV. MMWR Recomm Rep. 2002;51(RR-7):1-55.
36 Brinkman K, ter Hofstede HJ, Burger DM, et al. Adverse effects of reverse transcriptase inhibitors: mitochondrial toxicity as common pathway. AIDS. 1998;12:1735-1744.
37 Izuta S, Saneyoshi M, Sakurai T, et al. The 5'-triphosphates of 3'-azido-3'-deoxythymidine and 2', 3'- dideoxynucleosides inhibit DNA polymerase gamma by different mechanisms. Biochem Biophys Res Commun. 1991;179:776-783.
38 Kakuda TN. Phannacology of nucleoside and nucleoude reverse transcriptase inhibitor-induced mitochondrial toxicity. Clin Ther. 2000:22:685-708.
39 Simpson MV, Chin CD, Keilbaugh SA, etal. Studies on the inhibition of mitochondrial DNA replication by 3'-azido- 3'-deoxythymidine and other dideoxynucleoside analogs which inhibit HIV-1 replication. Biochem Pharmacol. 1989;38:1033-1036.
40 Benbrik E, Chariot P, Bonavaud S, et al. Cellular and mitochondrial toxicity of zidovudine (AZT), didanosine (ddI) and zalcitabine (ddC) on cultured human muscle cells. J Neural Sci. 1997;149:19-25.
41 Chairot P, Le Magnet F, Authier FJ, et al. Cytochrome c oxidase deficiency in zidovudine myopathy affects perifascicular muscle fibres and arterial smooth muscle cells. Neuropathol Appl Neurobiol, 1995:21:540-547.
42 Chariot P, Benbrik E, Schaeffer A, Gherardi R. Tubular aggregates and partial cytochrome c oxidase deficiency in skeletal muscle of patients with AIDS treated with zidovudine. Acta Neuropathol. 1993;85: 431-436.
43 McCurdy DT III, Kennedy JM. AZT decreases rat myocardial cytochrome oxidase activity and increases beta-myosin heavy chain content. J Mol Cell Cardiol. 1998;30:1979-1989.
44 Arnaudo E, Dalakas M, Shanske S, et al. Depletion of muscle mitochondrial DNA in AIDS patients with zidovudine-induced myopathy. Lancet. 1991;337(8740):508-510.
45 Casademont J, Barrientos A, Grau JM, et al. The effect of zidovudine on skeletal muscle mtDNA in HIV-1 infected patients with mild or no muscle dysfunction. Brain. 1996;119(pt 4): 1357-1364.
46 de la Asuncion JG, del Olmo ML, Sastre J, et al. Zidovudine (AZT) causes an oxidation of mitochondrial DNA in mouse liver. Hepatology. 1999;29:985-987.
47 Gonzales, Cid M, Larripa I. Genotoxic activity of azidothymidine (AZT) in in vitro systems. Mutat Res. 1994;321(1-2):113-118.
48 Lewis W, Papoian T, Gonzalez B, et al. Mitochondrial ultrastructural and molecular changes induced by zidovudine in rat hearts. Lab Invest. 1991:65:228-236.
49 Szabados E, Fischer GM, Toth K, et al. Role of reactive oxygen species and poly-ADP-ribose polymerase in the development of AZTinduced cardiomyopathy in rat. Free Radic Biol Med. 1999;26(3-4): 309-317.
50 Lewis W, Gonzalez B, Chomyn A, Papoian T. Zidovudine induces molecular, biochemical, and ultrastructural changes in rat skeletal muscle mitochondria. J Clin Invest. 1992:89:1354-1360.
51 Chen SC, Barker SM, Mitchell DH, et al. Concurrent zidovudineinduced myopathy and hepatoxicity in patients treated for human immunodeficiency virus (HIV) infection. Pathology. 1992:24:109-111.
52 Dalakas MC, Illa I, Pezeshkpour GH, et al. Mitochondrial myopathy caused by long-term zidovudine therapy. N Engl J Med. 1990;322: 1098-1105.
53 Modica-Napolitano JS. AZT causes tissue-specific inhibition of milochondrial biocnergetic function. Biochem Biophys Res Commun. 1993; 194:170-177.
54 McCurdy DT III, Kennedy JM. Skeletal muscle mitochondria from AZT-treated rats have a diminished response to chronic electrical stimulation. J Appl Physiol. 1996;81:326-334.
55 Chariot P, Monnet I, Mouchel M, et al. Determination of the blood lactate:pyruvate ratio as a noninvasive test for the diagnosis of zidovudine myopathy. Arthritis Rheum. 1994;37:583-586.
56 Darko DF, Mitler MM, Miller JC. Growth hormone, fatigue, poor sleep, and disability in HIV infection. Neuroendocrinology, 1998;67: 317-324.
57 Roy PM, Gouello JP, Pennison-Besnier I, Chennebault JM. Severe lactic acidosis induced by nucleoside analogues in an HIV-infected man. Ann Emerg Med. 1999;34:282-284.
58 Herzberg NH, Zorn I, Zwart R, et al. Major growth reduction and minor decrease in mitochondrial enzyme activity in cultured human muscle cells after exposure to zidovudine. Muscle Nerve. 1992;15: 706-710.
59 Chalmers AC, Greco CM, Miller RG. Prognosis in AZT myopathy. Neurology. 1991;41:1181-1184.
60 Sinnwell TM, Sivakumar K, Soueidan S, et al. Metabolic abnormalities in skeletal muscle of patients receiving zidovudine therapy observed by 31P in vivo magnetic resonance spectroscopy. J Clin Invest. 1995:96:126-131.
61 Cade WT, Fantry LE, Nabar SR, et al. A comparison of Qt and a-vO^sub 2^ in individuals with HIV taking and not taking HAART. Med Sci Sports Exerc. 2003;35:1108-1117.
62 Cade WT, Fantry LE, Nabar SR, et al. Impaired oxygen on-kinetics in individuals with HIV. Arch Phys Med Rehabol. 2003;84:1831-1838.
63 Nolte LA, Yarasheski KE, Kawanaka K, et al. The HIV protease inhibitor indinavir decreases insulin- and contraction-stimulated glucose transport in skeletal muscle. Diabetes. 2001;50:1397-1401.
64 Kaul S, Fishbein MC, Siegel RJ. Cardiac manifestations of acquired immune deficiency syndrome: a 1991 update. Am Heart J. 1991;122: 535-544.
65 Rerkpattanapipat P, Wongpraparut N, Jacobs LE, Kotler MN. Cardiac manifestations of acquired immunodeficiency syndrome. Arch Intern Med. 2000;160:602-608.
66 Milei J, Grana D, Fernandez Alonso G, Matturri L (Committee for the Study of Cardiac Involvement in AIDS). Cardiac involvement in acquired immunodeficiency syndrome: a review to push action. Clin Cardiol. 1998;21:465-472.
67 Yunis NA, Stone VE. Cardiac manifestations of HIV/AIDS: a review of disease spectrum and clinical management. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18:145-154.
68 Currie PF, Goldman JH, Caforio AL, et al. Cardiac autoimmunity in HIV related heart muscle disease. Heart. 1998;79:599-604.
69 Calabrese LH, Proffitt MR, Yen-Lieberman B, et al. Congestive cardiomyopathy and illness related to the acquired immunodeficiency syndrome (AIDS) associated with isolation of retrovirus from myocardium. Ann Intern Med. 1987;107:691-692.
70 Grody WW, Cheng L, Lewis W. Infection of the heart by the human immunodeficiency virus. Am J Cardiol. 1990;66:203-200.
71 Felker GM, Thompson RE, Hare JM, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342:1077-1084.
72 Grunfeld C, Kotler DP, Hamadeh R, et al. Hypertriglyceridemia in the acquired immunodeficiency syndrome. Am. J Med. 1989;86:27-31.
73 Sullivan AK, Nelson MR, Moyle GJ, et al. Coronary artery disease occurring with prolease inhibitor therapy. Int J STD AIDS. 1998;9: 711-712.
74 Ault A. FDA warns of potential protease-inhibitor link to hyperglycaemia. Lancet. 1997;349(9068):1819.
75 Assmann G, Cullen P, Schulte H. The Munster Heart Study (PROCAM). Results of follow-up at 8 years. Eur Heart J. 1998;19(suppl A):A2-A11.
76 Haim M, Benderly M, Brunner D, et al. Elevated serum triglyceride levels and long-term mortality in patients with coronary heart disease: the Bezafibrate Infarction Prevention (BIP) Registry. Circulation. 1999; 100:475-482.
77 Meng Q, Lima JA, Lai H, et al. Coronary artery calcification, atherogenic lipid changes, and increased erythrocyte volume in black injection drug users infected with human immunodeficiency virus-1 treated with protease inhibitors. Am Heart J. 2002;144:642-648.
78 Holmberg SD, Moorman AC, Williamson JM, et al. Protease inhibitors and cardiovascular outcomes in patients with HIV-1. Lancet. 2002;360(9347):1747-1748.
79 Stein JH, Klein MA, Bellehumeur JL, et al. Use of human immunodeficiency virus-1 protease inhibitors is associated with atherogenic lipoprotein changes and endothelial dysfunction. Circulation. 2001; 104:257-202.
80 Domanski MJ, Sloas MM, Follmann DA, et al. Effect of zidovudine and didanosine treatment on heart function in children infected with human immunodeficiency virus. J Pediatr. 1995;127:137-146.
81 Hecht SR, Berger M, Van Tosh A, Croxson S. Unsuspected cardiac abnormalities in the acquired immune deficiency syndrome: an echocardiographic study. Chest. 1989;96:805-808.
82 Duong M, Cottin Y, Piroth L, et al. Exercise stress testing for detection of silent myocardial ischemia in human immunodeficiency virus-infected patients receiving antiretroviral therapy. Clin Infect Dis. 2002;34:523-528.
83 McKelvie RS, Teo KK, McCartney N, et al. Effects of exercise training in patients with congestive heart failure: a critical review. J Am Coll Cardiol. 1995:25:789-796.
84 Hambrecht R, Niebauer J, Fiehn K, et al. Physical training in patients with stable chronic heart failure: effects on cardiorespiratory fitness and ultrastructural abnormalities of leg muscles. J Am Coll Cardiol. 1995;25:1239-1249.
85 Lipkin DP, Jones DA, Round JM, Poole-Wilson PA. Abnormalities of skeletal muscle in patients with chronic heart failure. Int J Cardiol. 1988;18:187-195.
86 Aggarwal A, Ades PA. Exercise rehabilitation of older patients with cardiovascular disease. Cardiol Clin. 2001;19:525-536.
87 Sullivan PS, Hanson DL, Chu SY, et al. Epidemiology of anemia in human immunodeficiency virus (HIV)-infected persons: results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood. 1998;91:301-308.
88 Richman DD, Fischl MA, Grieco MH, et al. The toxicity of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex: a double-blind, placebo-controlled trial. N Engl J Med. 1987;317:192-197.
89 Faulds D, Heel RC. Ganciclovir: a review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy in cytomegalovirus infections. Drugs. 1990;39:597-638.
90 Keisu M, Wiholm BF, Palmblad J. Trimethoprim-sulphamethoxazole-associated blood dyscrasias: ten years' experience of the Swedish spontaneous reporting system. J Intern Med. 1990;228:353-360.
91 Maciejewski JP, Weichold FF, Young NS. HIV-1 suppression of hematopoiesis in vitro mediated by envelope glycoprotein and TNF-alpha. J Immunol. 1994;153:4303-4310.
92 Zauli G, Re MC, Visani G, et al. Evidence for a human immunodeficiency virus type 1-mediated suppression of uninfected hematopoielic (CD34+) cells in AIDS patients. J Infect Dis. 1992;166:710-716.
93 Naides SJ, Howard EJ, Swack NS, et al. Parvovirus B19 infection in human immunodeficiency virus type 1-infected persons failing or intolerant to zidovudine therapy. J Infect Dis. 1993;168:101-105.
94 Horsburgh CR Jr. Mycobacterium avium complex infection in the acquired immunodeficiency syndrome. N Engl J Med. 1991;324: 1332-1338.
95 Remacha AF, Riera A, Cadafalch J, Gimferrer E. Vitamin B-12 abnormalities in HIV-infected patients. Eur J Haematol. 1991;47:60-64.
96 Ciaffoni S, Luzzati R, Roata C, et al. Presence and significance of cold agglutinins in patients with HIV infection. Haematologica. 1992; 77:233-236.
97 Koskolou MD, Roach RC, Calbet JA, et al. Cardiovascular responses to dynamic exercise with acute anemia in humans. Am J Physiol. 1997;273(4 pt 2):H1787-H1793.
98 Gregg SG, Willis WT, Brooks GA. Interactive effects of anemia and muscle oxidative capacity on exercise endurance. J Appl Physiol 1989;67:765-770.
99 Sproule BJ, Mitchell JH, Miller WF. Cardiopulmonary physiological responses to heavy exercise in patients with anemia. J Clin Invest. 1960;39:378-388.
100 Astrand PO, Saltin B. Plasma and red cell volume after prolonged severe exercise. J Appl Physiol. 1964;19:829-832.
101 Stringer WW. Mechanisms of exercise limitation in HIV+ individuals. Med Sci Sports Exerc. 2000;32(suppl 7):S412-S421.
102 MacArthur RD, Levine SD, Birk TJ. Supervised exercise training improves cardiopulmonary fitness in HIV-infected persons. Med Sci Sports Exerc. 1993;25:684-688.
103 Chatterjee S, Dey SK, Nag SK. Maximum oxygen uptake capacity of smokers of different age groups. Jpn J Physiol. 1987;37:837-850.
104 Song EY, Lim CL, Lim MK. A comparison of maximum oxygen consumption, aerobic performance, and endurance in young and active male smokers and nonsmokers. Mil Med. 1998;163:770-774.
105 Curtis J, Goodman P, Hopewell P. Non-invasive tests in the diagnostic evaluation for P carinni pneumonia in patients with or suspected of having AIDS. Am Rev Respir Dis. 1986;133(suppl):A182.
106 Stover DE, White DA, Romano PA, et al. Spectrum of pulmonary diseases associated with the acquired immune deficiency syndrome. Am J Med. 1985;78:429-437.
107 Coleman DL, Dodek PM, Golden JA, et al. Correlation between serial pulmonary function tests and fiberoptic bronchoscopy in patients with Pneumocystis carinii pneumonia and the acquired immune deficiency syndrome. Am Rev Respir Dis. 1984;129:491-493.
108 Gagliardi A, White DA, Meduri GU, et al. Pulmonary function abnormalities in AIDS patients with respiratory illness. Am Rev Respir Dis. 1985;131(suppl):A75.
109 Gagliardi A, White DA, Stover DE, et al. A non-invasive index for the diagnosis of pneumocytis carinni pneumonia (PCP) in patients with the acquired immunodeficiency syndrome (AIDS). Am Rev Respir Dis. 1986;133(suppl):A183.
110 Hopewell PC, Luce JM. Pulmonary involvement in the acquired immunodeficiency syndrome. Chest. 1985;87:104-112.
111 Smith DE, McLuckie A, Wyatt J, Gazzard B. Severe exercise hypoxaemia with normal or near normal X-rays: a feature of Pneumocystis carinii infection. Lancet. 1988;2(8619):1049-1051.
112 Hsia CC. Cardiopulmonary limitations to exercise in restrictive lung disease. Med Sci Sports Exerc. 1999;31(suppl 1):S28-S32.
113 Walker K, McGown A, Jantos M, Anson J. Fatigue, depression, and quality of life in HIV-positive men. J Psychosoc Nurs Ment Health Serv. 1997;35:32-40.
114 Skurnick JH, Bogden JD, Baker H, et al. Micronutrient profiles in HIV-1-infected heterosexual adults. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;12:75-83.
115 Cupler EJ, Otero C, Hench K, et al. Acetylcholine receptor antibodies as a marker of treatable fatigue in HIV-1 infected individuals. Muscle Nerve. 1996;19:1186-1188.
116 Groopman JE. Fatigue in cancer and HIV/AIDS. Oncology (Huntingt). 1998;12:335-344; discussion 345-336, 351.
117 Abbott M, Khoo SH, Hammer MR, Wilkins EG. Prevalence of cortisol deficiency in late HIV disease. J Infect. 1995;31:1-4.
118 Perkins DO, Leserman J, Stern RA, et al. Somatic symptoms and HIV infection: relationship to depressive symptoms and indicators of HIV disease. Am J Psychiatry. 1995;152:1776-1781.
119 Rigsby LW, Dishman RK, Jackson AW, et al. Effects of exercise training on men seropositive for the human immunodeficiency virus-1. Med Sci Sports Exerc. 1992;24:6-12.
120 Smith BA, Neidig JL, Nickel JT, et al. Aerobic exercise: effects on parameters related to fatigue, dyspnea, weight and body composition in HIV-infected adults. AIDS. 2001;15:693-701.
121 Terry L, Sprinz E, Ribeiro JP. Moderate and high intensity exercise training in HIV-1 seropositive individuals: a randomized trial. Int J Sports Med. 1999;20:142-146.
122 LaPerriere A, Klimas N, Fletcher MA, et al. Change in CD4+ cell enumeration following aerobic exercise training in HIV-1 disease: possible mechanisms and practical applications. Int J Sports Med. 1997;18(suppl 1):S56-S61.
123 Nixon S, O'Brien K, Glazier RH, Wilkins AL. Aerobic exercise interventions for people with HIV/AIDS. Cochrane Database Syst Rev. 2001(1):CD001796.
124 Grinspoon S, Mulligan K. Weight loss and wasting in patients infected with human immunodeficiency virus. Clin Infect Dis. 2003; 36(suppl 2):S69-S78.
WT Cade, PT, PhD, is Postdoctoral Fellow, Division of Endocrinology, Metabolism and Lipid Research, Department of Internal Medicine, Washington University School of Medicine, 660 S Euclid Ave, St Louis, MO 63110 (USA) (tcade@im.wustl.edu). He was a doctoral student in the Department of Physical Therapy and Graduate School, University of Maryland School of Medicine, Baltimore, Md, at the time this article was written. Address all correspondence to Dr Cade.
L. Peralta, MD, is Associate Professor of Pediatrics and Chief, Division of Adolescent and Young Adult Medicine, and Director, Adolescent HIV Program, Department of Pediatrics, University of Maryland School of Medicine.
RE Keyser, PhD, is Assistant Professor, Department of Physical Therapy, University of Maryland School of Medicine.
Dr Cade provided conccpt/idea/projcct design, writing, and data collection and analysis. Dr Peralta and Dr Keyser provided consultation (including review of manuscript before submission).
Copyright American Physical Therapy Association Jul 2004
Provided by ProQuest Information and Learning Company. All rights Reserved