An 11-year-old, right-handed boy presented with a long-standing history of motor difficulties, including a slow, awkward running style and difficulty jumping. His developmental history was notable for motor delay and persistent mild gross motor difficulties. He did not sit until 9½ months, had difficulty pulling to stand, and did not walk independently until 2 years. Past medical history was unremarkable, except for an uneventful tooth extraction under general anesthesia. No history of myoglobinuria or myalgias was given. Several paternal family members had similar motor difficulties, and a cousin had a malignant hyperthermic response to general anesthesia. Physical examination revealed a cooperative boy with a slender build but no dysmorphisms or neurocutaneous stigmata. Mild proximal muscle weakness of the upper and lower extremities was evident, and he had difficulty getting up from a lying position and a modified Gower maneuver. Gait was normal, but running was abnormal with limited hip flexion. Electromyography and creatine kinase levels were normal.
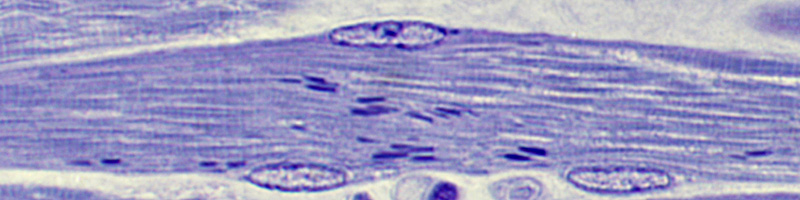
A biopsy of the left quadriceps muscle was performed under local anesthesia. Hematoxylin-eosin-stained sections showed circular rings of light basophilia in many fibers. Fiber size varied moderately, and a mixture of both atrophied and slightly hypertrophied fibers was present (Figure 1). Mild increased endomysial fibrous tissue and rare perivascular lymphocytes were also noted. Enzyme histochemistry revealed deficient nicotinamide-adenine dinucleotide dehydrogenase (NADH) (Figure 2) and cytochrome c oxidase activity in circular areas within predominantly type I fibers. Esterase, periodic acid-Schiff, and oil red O stains also highlighted these areas. Electron microscopy of the abnormal regions showed focal derangements of sarcomeric architecture, increased accumulations of Z disc material, and a lack of mitochondria (Figure 3, original magnification ×4600). Areas outside the cores were ultrastructurally normal.
What is your diagnosis?
Pathologic Diagnosis: Central Core Disease
The congenital myopathies are loosely defined as a group of muscle diseases that typically feature hypotonia in infancy, a slowly progressive or nonprogressive course, and characteristic histochemical features on biopsy.1,2 Most congenital myopathies are related to inheritable protein derangements that disrupt muscle development and organization. Central core disease (CCD) was the first congenital myopathy described and was initially reported in 1956.3 Subsequent investigations verified the original clinical and histopathologic findings, and showed the disorder to be associated with malignant hyperthermia susceptibility (MHS).1,2,4-6
Central core disease represents a wide spectrum of clinical severity. A typical case presents with hypotonia in infancy and proximal muscle weakness in early childhood; these conditions persist throughout adolescence and adulthood. Motor milestones are delayed, and some patients may not walk independently until 4 years. Contractures are rare. With increasing age, weakness persists and seems to favor the lower extremities. Running, rising from a supine position, and climbing stairs are the most common difficulties. Atrophy is not conspicuous, but most muscles are thin. Cranial nerve musculature is less involved, and ophthalmoplegia is rare. Associated skeletal alterations, including kyphoscoliosis, congenital hip dislocation, flat feet, clubfoot, and flexion deformities of the fingers, are common and may require surgery. Cardiac abnormalities, including mitral valve prolapse and arrhythmias, are rare. The course is usually nonprogressive or slowly progressive without a significant impact on life expectancy. Intellect is unaffected. Creatine kinase levels are normal or slightly elevated. Electromyography may show short-duration, small-amplitude, polyphasic motor units with an increased terminal innervation ratio (number of fibers innervated by a single anterior horn cell). Nerve conduction studies are usually unremarkable.1,2,6
The dominant feature of the muscle by light microscopy is the myofibril core.1,2,5 The cores are easily detected in frozen specimens, where they show reduced enzyme activity with NADH, succinate dehydrogenase, and cytochrome c oxidase stains. In adenine triphosphatase and phosphorylase-stained sections, the cores appear light compared to surrounding tissue. The noncore elements stain normally, although a thin rim of increased oxidative activity around the core may be apparent. The cores are usually centrally positioned in transverse section but may be eccentrically located. In longitudinal sections, they appear to run along the long axis of the muscle fiber across several sarcomeres, up to 300 µm in total distance.5 An increase in central nuclei and a type I fiber predominance have been described, usually in more severely affected individuals. Increased endomysial fibrous tissue and perivascular lymphocytes may be seen in severe cases. The cores can be multiple and small, causing some confusion with multi-minicore disease.5 Ultrastructurally, the cores contain sharply marginated areas of densely packed myo-filaments with varying disruption of sarcomere structure and irregular Z bands.2 Mitochondria and glycogen granules are decreased or absent. Sarcoplasmic reticulum and T tubules are apparent, but abnormal.
From a pathologic standpoint, the presence of cores may represent several entities. Cores are similar in morphology to the target fibers found in denervation atrophy. Targets, which also have a type I fiber predominance, typically consist of 3 zones-a central zone lacking enzyme activity, an intermediate zone with increased activity, and a peripheral zone of normal activity. Target structures are more commonly single and centrally located. Cores usually run a greater length of the muscle fiber than target lesions.2 A distinction from multi-minicore disease can be difficult when the cores of CCD are smaller than usual and multiple in number. True multi-minicore samples feature loss of cross-striation and staining intensity in multiple areas of a longitudinal section. Multi-minicores can be found in many myopathies and rarely in normal controls.1 Finally, cores have been found in combination with nemaline rods in patients with congenital myopathy.6,7
Central core disease has been thought of as an autosomal dominant disorder. Descriptions of sporadic cases and recessive inheritance patterns suggest that the disorder is a heterogeneous one in which most forms are autosomal dominant with variable penetration.1 The disorder has been assigned to chromosome 19q12-13.2 and the RYRI gene locus.8 RYR1 encodes a 560-kd protein, the ryanodine receptor, which forms a calcium release channel spanning the membrane of the sarcoplasmic reticulum and mediates calcium release from the sarcoplasmic reticulum to the myoplasm in excitation-contraction coupling. More than 20 mutations have been described in the RYR1 locus.9,10 The manner in which mutations in RYR1 and the ryanodine receptor lead to CCD has yet to be determined. The finding of abnormal ryanodine receptor in cores implicates this protein in the process of core formation.7
The association between MHS and CCD was recognized long before RYR1 was found to be linked with both disorders.4 It was once thought that all CCD patients also had MHS, but this does not appear to be the case. Segregation analyses have not shown all MHS cases to be linked to chromosome 19, and not all patients with CCD necessarily have MHS. Furthermore, of 22 mutations in the RYR1 gene region studied, 21 are related to MHS, 7 have been linked to CCD, and 1 mutation segregated with CCD and not MHS.10 The precise determinants of whether an RYR1 mutation leads to MHS, CCD, or both have yet to be discovered.
References
1. Bodensteiner P. Congenital myopathies. Muscle Nerve. 1994:17:131-144.
2. Fardeau M, Tome FMS. Congenital myopathies. In: Engel AG, Franzini-Armstrong C, eds. Myology. 2nd ed. New York, NY: McGraw-Hill Inc; 1994:1487-1532.
3. Shy GM, Magee K. A new congenital nonprogressive myopathy. Brain. 1956:79:610-621.
4. Denborough MA, Dennet X, Anderson RM. Central core disease and malignant hyperpyrexia. Br Med J. 1973;1:272-273.
5. Goebel HH. Central core disease. In: Karpati G, ed. Structural and Molecular Basis of Skeletal Muscle Disease. Basel, Switzerland: International Society of Neuropathology Neuropath Press; 2002:65-67.
6. Shuaib A, Paasuke RT, Brownell KW. Central core disease: clinical features in 13 patients. Medicine (Baltimore). 1987:66:389-396.
7. Scacheri PC, Hoffman EP, Fratkin JD, et al. A novel ryanodine receptor mutation causing both cores and rods in congenital myopathy. Neurology. 2000:55: 1689-1696.
8. Mulley JC, Kozman HM, Phillips HA, et al. Refined genetic localization for central core disease. Am J Hum Genet. 1993:52:398-405.
9. Curran JL, Hall WJ, Halsall PJ, et al. Segregation of malignant hyperthermia, central core disease and chromosome 19 markers. Br J Anaesth. 1999:83:217-222
10. McCarthy T, Quane KA, Lynch PJ. Ryanodine receptor mutations in malignant hyperthermia and central core disease. Hum Mutat. 2000;15:410-417.
David M. Giampetro, MD; Richard A. Prayson, MD; Neil R. Friedman, MD; Susan M. Staugaitis, MD, PhD
Accepted for publication November 6, 2003.
From the Department of Neurology, Cleveland Clinic Florida, Weston, Fla (Dr Giampetro); and the Departments of Anatomic Pathology (Drs Prayson and Staugaitis) and Neurology (Dr Friedman), Cleveland Clinic Foundation, Cleveland, Ohio.
The authors have no relevant financial interest in the products or companies described in this article.
Corresponding author: Richard A. Prayson, MD, Department of Anatomic Pathology, The Cleveland Clinic Foundation, 9500 Euclid Ave, Cleveland, OH 44195 (e-mail: praysor@ccf.org).
Reprints not available from the authors.
Copyright College of American Pathologists Apr 2004
Provided by ProQuest Information and Learning Company. All rights Reserved