Molecular diagnostics is a branch of clinical diagnostics that uses primarily DNA or RNA as a biomarker for clinical testing. It combines various gene-based amplification technologies with highly sophisticated detection methods for the clinical diagnosis of a vast variety of diseases including infectious diseases, cancer, and inherited diseases. The principal application of gene-based amplification technology is to identify pathogen or gene-specific nucleic acid sequences that are used as surrogate markers for the identification of either infectious pathogens or alteration of disease-related genes. There are generally three classes of gene-based amplification technologies: target-based, e.g., PCR; probe-based, e.g., LCR; and signal-based, e.g., bDNA. Real-time detection of PCR allows us to quantify amplified amplicons with a broad dynamic range and it offers a unique way to detect genetic mutations. Other technologies such as immuno-PCR and bio-barcode assay (BCA) combine different amplification tactics offering extreme detection sensitivity ranging from femtogram (10^sup -15^) to zeptogram (10^sup -21^). Even though quantum dots technology is in its infant stage, its potential to further increase diagnostic sensitivity and specificity is likely beyond our current imagination. Future diagnostic technologies include the use of genomic and proteomic approaches especially in pure cell types or even in the single-cell level, which open up endless new possibilities for gene-based diagnostics at entirely different levels. In this article, principles of various current gene-based amplification and detection technologies along with their clinical applications are discussed. New technologies that could potentially be used in future gene-based diagnosis are introduced.
ABBREVIATIONS: BCA = bio-barcode amplification; bDNA = branched DNA; FRET = fluorescence resonance energy transfer; IPCR = immuno-PCR; LCM = laser capture microdissection; LCR = ligase chain reaction; NASBA = nucleic acid sequence based amplification; PCR = polymerase chain reaction; qdots = quantum dots; SDA = strand displacement array; SNP = single nucleotide polymorphism; T^sup M^ = melting temperature.
INDEX TERMS: gene-based amplification; molecular diagnostics.
Clin Lab Sci 2005;18(4):254
LEARNING OBJECTIVES
1. Describe the classification of gene-based amplification methods.
2. State the principles of gene-based amplification methods.
3. Discuss the advantages and disadvantages of gene-based diagnostics.
4. Define future prospectives of gene-based diagnostics.
Twenty years has passed since the first description of the polymerase chain reaction (PCR) technique and its application to amplification of the β-globin gene sequence and to restriction fragment length polymorphism analyses for the diagnosis of sickle-cell anemia.1 During this period of time, there has been a nearly explosive growth in the number and variety of new gene-based methodologies in the field of genebased diagnostics, also called molecular diagnostics.
Molecular diagnostics, based on nucleic acid amplification and detection technologies, is a branch of clinical diagnostics that uses primarily DNA or RNA originated either from patients or pathogens as the biomarker for the clinical testing. These genebased diagnostic approaches span from detection of infectious diseases, cancer detection, and genetic diseases to forensic identity testing. One of the most desirable features of gene-based technologies in clinical diagnostics is their rapid, specific, and direct detection of genes of interest with very high sensitivity. Many of them allow additional and precise quantification of genes of interest with broad dynamic range. Importantly, they can be performed directly from clinical specimens without the need for laboratory cultivation, which is often time-consuming.
A unique feature of gene-based diagnosis of infectious diseases is that it can detect pathogens that cannot be detected by conventional diagnostic tests. For example, we can now readily detect many of the viral infections that are either difficult or impossible to culture in the laboratory. Another example of using gene-based assays is that we can now detect HIV infection in newborns on the day of birth. Previously, when antibody-based tests were used, a positive diagnosis was not possible until three to seven months of age. In another article in this Focus section, Drs Niel Constantine and Richard Zhao from University of Maryland School of Medicine describe in detail the molecularbased diagnosis of HIV-1 infections.
Molecular testing can also be used to predict potential risk of an individual for onset of a specific cancer such as breast cancer with predispositions oibrcal/2 gene mutations.2·3 Dr W Craig Hooper and his colleague Stacy C League from the Centers for Disease Control and Prevention provide a detailed description of this type of testing in congenital thrombosis in this issue. If clinical symptoms or other diagnostic tests implicate a specific cancer such as T-cell leukemia, gene-based testing could also be used to confirm diagnosis by detecting possible known T-cell gene arrangements. Furthermore, these same tests could be used to monitor success of anti-cancer therapy. For example, disappearance of the same T-cell gene re-arrangement would indicate cancer remission in the patient.
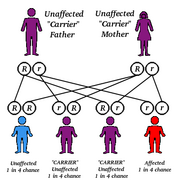
Molecular-based genetic tests can be used for many different purposes including carrier screening, prenatal testing, cancer risk, or confirmatory cancer testing, and genetic identification. Carrier testing normally involves identification of an individual who carries one copy of a gene for a disease that requires two copies for the disease to be expressed. An example of such a carrier testing includes Ashkenazi genetic carrier screening for an array of genetic diseases including Tay-Sachs diseases, Gaucher disease, cystic fibrosis, Canavan disease, Niemann-Pick, and familial dysautonomia. For further introduction on the use of molecular-based methodologies in genetic testing for cystic fibrosis, see the article in the next issue of Clinical Laboratory Science (Winter 2006) by Dr Edward Highsmith and his colleague Timothy S UphofF from Mayo Clinic. Prenatal testing involves identification of gene alternations in the fetus for a specific genetic disease such as fragile X syndrome.
For cancer detection, molecular-based diagnosis has never been so close to reality in assisting physicians in detecting specific cancers or even in assisting in monitoring anti-cancer therapies. Dr Christopher Gocke from John Hopkins University provides specific information on molecular diagnosis and monitoring of hematological malignancies in the next issue (Winter 2006). Dr Gocke's article will provide detailed information on molecular diagnostics and monitoring of hematological malignancies.
Because of the genetic distinction of each individual, molecular-based testing can also be used for forensic or identity testing. Short tandem repeat (STR) assay has been used, for example, for paternity identification or criminal investigations. STR has also been implemented in the clinical setting to monitor efficacy of bone marrow transplantation of leukemia patients.
Altogether, gene-based molecular diagnostics provides us with tremendous power for clinical diagnosis of a broad range of diseases. With emergence of new and more powerful technologies, use of molecular diagnostics will only continue to grow. Implementation of more sensitive and specific tests with these new technologies in clinical diagnosis would allow us to continue improving patient care and thus saving more lives.
In this article, I will briefly describe principles of various gene-based amplification technologies including some of the most popular technologies such as Amplicor® (Roche), NucliSens® (OrganonTeknika), Quantiplex® (Bayer), as well as real-time PCR methods that are currently available in the market for clinical diagnostics. Other technologies such as LCR® (Abbott), Qâ-replicase® (Gene-Track), and SDA® (Becton Dickinson) will also be introduced. New emerging technologies such as immuno-PCR (IPCR), bio-barcode assay (BCA) and genomic/proteomic approaches, which have not yet been applied to clinical testing, but may prove to be even more powerful tools in molecular diagnostics, will be addressed.
Gene-based amplification typically consists of three major steps: primertemplate hybridization, synthesis, and amplification. The gene-based amplification methodologies may be categorized based on the means of amplification, i.e., 1) target-based amplification methods, which are designed to detect and amplify the target gene of interest; 2) probe-based amplification methods, which rely on amplification of the probes that are homologous to a specific gene target, and, 3) signal-based technologies that amplify the signal rather than the gene target sequence.
GENE-BASED AMPLIFICATION TECHNOLOGIES
The gene-based amplification technologies can be further divided into PCR-based or non-PCR based methods. PCR-based method is an artificial DNA amplification method that is performed at various temperatures using a thermocycler. In contrast, most of the non-PCR methods take advantage of the natural nucleic acid amplification processes. For example, ligase chain reaction (LCR) mimics the enzymatic ligation process; nucleic acid sequence based amplification (NASBA) mimics viral RNA reverse transcription and transcription; strand displacement assay (SDA) resembles the DNA excision repair process; and Qβ-replicase RNA amplification resembles bacteriophage replication. Another common feature of non-PCR-based assays is that these assays can be carried out at constant temperature without thermocycling.
In theory, a single molecule can be detected and amplified to 109 to 1012 molecules within a few hours of the amplification reaction. In clinical practice, however, a much lower efficiency is obtained due to impurities and other intrinsic factors within the clinical specimens that may affect the efficiency of the amplification. Nevertheless, 10 to 100 copies of the target nucleic acid sequences, for example, can normally be detected with high probability.
DETECTION OF AMPLIFIED GENE PRODUCTS
Typically the amplified gene products can be detected by using various labeled reporter molecules such as enzymes, antigenic substrates, radioisotopes, chemiluminescent moieties, or fluorescent labels (Table 1). The classical means of gene detection is the use of DNA probes labeled with radioactive ^sup 32^P. Binding of the probe to the amplified product (hybridization) enables visualization of the gene product either by autoradiography or liquid scintillation counting. In most of the current commercially available diagnostic kits, however, radioactive isotopes are replaced by enzymes, affinity labels, chemiluminescent molecules, or fluorescent reporters for the detection of the amplified products. For example, direct labeling of oligonucleotides with the enzymes alkaline phosphatase or horseradish peroxidase, is responsible for the signal amplification in the bDNA signal amplification assay. Addition of enzyme specific substrates such as dioxetane to the amplified product gives light emission that can be detected by luminometry. Affinity labels such as biotin and digoxigenin are incorporated into the primers in PCR-based assays by enzymatic (nick translation or random-priming techniques) or nonenzymatic, e.g., photobiotin methods. Streptavidin linked to an enzyme is used to detect the moiety attached to the primers, and the detection is completed through the use of colorimetric or chemiluminescent substrates for the enzyme. Chemiluminescent markers are chemical groups that release light when exposed to certain substrates after the hybridization reaction is complete. The light emitted can be detected with X-ray film or a luminometer. Such assays have sensitivity ranges equal to or greater than those of ^sup 32^P.
Chemiluminescent labels, such as acridinium esters, have been incorporated into many commercially available probe kits and are used in a format that is rapid and highly efficient. Fluorescent labels have now been used in real-time PCR and single nucleotide polymorphism (SNP) analyses for the detection of amplified gene products or gene mutations.
There are five commonly used fluorophores including FAM (SYBR Green I), JOE (VIC), TAMRA (NED or Cy3), ROX (Texas Red), and Cy5. Each of them has a different excitation and emission spectrum thus allowing detection of single or multiplex (up to five colors) amplicons with great assay versatility.
Typically a fluorescent dye molecule is covalently attached to either a primer or a probe. Upon incorporation of the primer into an amplicon during gene-amplification in real-time PCR, increase of the fluorescence of the dye molecule can be detected at a single molecular level which thus allows real-time quantification of gene amplification cycle-by-cycle. The most recent new label for the detection of biological molecules is the fluorescent semiconductor nanocrystals, also known as quantum dots or qdots.4 Evolved from electronic material science to the applications in molecular diagnostics, this new technology can monitor intracellular processes at the single molecular level with very high resolution. This extremely sensitive detecting label has far-reaching potential in improving sensitivity and specificity of future clinical diagnostic tests.
TARGET-BASED GENE AMPLIFICATION
Polymerase chain reaction (PCR)
PCR is a typical example of target-based amplification technology. For example, in the detection of a particular pathogen using PCR, a unique segment of DNA or RNA (rt-PCR), that represents a specific pathogen of interest, is selectively amplified and used to distinguish it from other organisms. Therefore, detection of a specific amplified gene sequence indicates the presence of a specific pathogen.
Protocols for detection of a vast variety of infective agents including viral, bacterial, fungal, and parasitic pathogens can be found in the literature. However, those 'in house' protocols are generally not adequate for immediate implementation in clinical testing unless, after proper assay validation, very restrictive QA/QC procedures are strictly enforced, and proper regulatory rules are followed. One limitation of the PCR-related techniques is that the blood sample has to be collected in tubes with anticoagulant such as ACD or EDTA. Heparin strongly inhibits the PCR reaction.
Cross-contamination is a major concern in PCR. However, an enzyme called uracil-N-glycosylase (UNG, commercially known as AmpErase®), which can break down pre-amplified amplicons, is incorporated in the Amplicor kits and works quite effectively in minimizing this potential problem. PCR-based technology for clinical diagnosis of various dis eases is commercially available under the commercial name Amplicor'M, through Roche Diagnostics Systems, Inc. These Amplicor tests include HIV, HCV, HBV, HPV, Clamydia trachomatis, and Neisseria gonorrhea.
Real-time PCR
PCR can also be used to quantify amplified gene sequences. However, the limitation associated with the traditional quantitative PCR is that the DNA copy numbers are calculated based on the final amplified gene products. Since DNA is amplified exponentially during PCR, a small variation in amplification efficiency early in the thermocycling process could potentially lead to a large variation in the final quantity of amplified products. Consequently, the intra- and inter-assay variability is often an issue to consider because the final accumulated product quantity may not necessarily be reflective of the initial copy number. Even though this limitation can be partially circumvented by adding an international quantification control, another shortcoming of the conventional PCRbased assays is that they generally have a narrow linear dynamic range of approximately 3 logs due to the nonlinear amplification of PCR. In contrast to conventional PCR, real-time PCR, which is also known as TaqMan(TM) or 5' exonuclease assay (Perkin-Elmer, Branchburg, NJ), quantifies PCR products cycle-by-cycle ('real-time') as they accumulate.5 Unlike conventional PCR, an internal probe is added to the detection process, which is an oligonucleotide with both a fluorescent reporter and a fluorescent quencher dye attached. If a target sequence is present, the probe anneals between the forward and reverse primers and is then digested by the 5' nuclease activity of the DNA polymerase as PCR proceeds (Figure 1). Digestion of the probe DNA separates the reporter dye from the quencher dye, making the reporter dye signal detectable. Detection of the resulting fluorescence collectively provides an immediate real-time quantification of the PCR process.
There are several advantages to real-time PCR. It does not rely on the final product at end of the PCR amplification for quantification as regular PCR does. DNA copy numbers are determined based on the threshold cycle (C^sub t^), which is directly proportional to the initial copy number. Thus, the measurement is highly accurate and reproducible. Since probe cleavage alone is responsible for increase of fluorescent signals, it is highly specific. For example, if the probe binds non-specifically to some other sequences that are not between the forward and reverse primers, it will not be cleaved or detected as part of the amplification. Conversely, non-specific primer binding and amplification will not be detected, because the probe is gene specific, hence does not bind to the same region. Since measurement of DNA copy number is directly proportional to the initial copy numbers, it allows much wider linear dynamic range of detection for quantification than conventional PCR. For an example of HIV-I proviral DNA quantification using the real-time PCR technology, see reference.6 Besides the quantificational power of real-time PCR, it can also be used for mutation detection or genotyping by using melting curve analysis of the amplified gene sequences. The rationale behind this capacity is based on the fact that every DNA fragment melts at a characteristic melting temperature (Tm). A mismatch between a mutated gene target and a fluorescent labeled wild type gene probe will result in a low Tm that can be readily detected by changes in fluorescent profile.
There are two types of probes used in real-time PCR: hydrolysis probes for real-time quantification and hybridization probes for single nucleotide polymorphisms (SNPs) and mutation detections. Examples of hydrolysis probes include TaqMan probes, molecular beacon probes, and scorpion primer-probes.7,8 The TaqMan probes present as linear oligonucleotides; oligonucleotides of molecular beacon probes are typically in a hairpin format labeled at one end with a quencher and at the other end with a fluorescent reporter. In the absence of gene targets, the fluorescence is quenched. However, when molecular beacons hybridize to their gene targets, the hairpin structures open and they emit intense fluorescent signals for real-time detections. Scorpion primer-probes incorporate both the primer and probe into oligonucleotides that exist in a hairpin loop structure. Similar to molecular beacons, the fluorescence of scorpion primer-probes is normally quenched. Upon primer-mediated DNA synthesis of the gene targets, the scorpion probes hybridize to the newly formed complementary sequences, separating the fluorescent reporters from the quenchers thus restoring the fluorescence. In principle, molecular beacons and scorpion probes provide better probetarget binding specificity than linear probes.
Hybridization probes have been used for detections of mutations and SNPs by combined use of melting curve analysis and sequence-specific fluorescence resonance energy transfer (FRET). In a FRET melting curve analysis, two hybridization probes that are complementary to a continuous region of the gene target are labeled with fluorescein or LC Red 640, respectively. When the two fluorescent labeled probes come together upon gene-specific hybridization, excitation of fluorescein causes an energy transfer, which subsequently results in excitation of the LC Red 640 molecule. Such a FRET allows detection of specific probe-gene hybridization. Melting curve analysis is based on the fact that each double strand DNA has its own unique melting temperature (Tm). A single change in nucleotide will result in change of Tm. Therefore, combined use of FRET for gene-specific hybridization with mutation-specific changes of Tm enables detection of specific gene mutations with high accuracy.
Nucleic acid sequence based amplification (NASBA)
NASBA is another target-based amplification method that is formerly known as 3SR (self-sustaining sequence replication). In contrast to PCR, however, this method is essentially an in vitro version of the natural replication of retroviral RNA. Therefore, this assay is useful only for detecting RNA targets such as HIV or HCV. A standard NASBA reaction contains T7 RNA polymerase, RNase H, avian myeloblastosis virus (AMV) reverse transcriptase, nucleoside triphosphates, two specific primers, and appropriate buffer contents. For quantification of HIV viral load, for example, primer 1 is about 45 bases in length with an average of 20 bases at the 3' end that are complementary to the 3' side of the target sequence. The 5' end of this primer contains a promoter sequence that is recognized by T7 RNA polymerase. Primer 2 is about 20 bases in length and is derived from the opposite (5' direction) side of the target sequence. The NASBA test involves repetitive reverse transcription from an RNA template by AMV reverse transcriptase and RNA amplification from cDNA by gene transcription viaT7 promoter. Approximately 40 copies of RNA can be made (versus two copies/cycle in PCR) in each cycle for each copy of the RNA target. Within a 90 minute reaction, approximately 1012 RNA molecules can be made starting with 10 copies of purified RNA molecules.
One advantage of using NASBA is that it can use any types of specimen, e.g., serum, plasma, cerebrospinal fluid, tissue, seminal plasma, or genital secretions. There is no specific requirement for anticoagulant. A drawback of this test is that it requires a separate RNA extraction step, making it more labor intensive. Consequently, a potential problem with NASBA is the significant risk of carry-over contamination between samples since much pipetting and tube opening must be performed for the isolation of viral RNA from plasma or serum specimens. The commercial name of NASBA amplification products is NucliSens(TM) through bioMerieux, Inc. Commercial tests currently are available include NucliSens CMVpp67, RSVA+B, Enterovirus, and HIV-I.
PROBE-BASED AMPLIFICATION
Ligase chain reaction (LCR)
In contrast to target-based amplification technology, probebased technique is designed to amplify the probe homologous to the target. LCR is a method designed to amplify the probes that are homologous to a specific target of interest. The rationale behind this method is that ligation is most efficient when two discrete probes hybridize to the target in a
head-to-tail fashion. Once the first pair of probes is ligated, it can in turn serve as a template for annealing and ligation of a second pair of probes complementary to its sequence. Recycled ligations between these two sets of ligated probes plus the original targets will result in a logarithmic accumulation of ligation products. Diagnostic tests using LCR are developed under the trademark name of LCx at Abbott Laboratories. A HIV-I LCx commercial test is available outside the United States.
Strand displacement amplification (SDA)
The key principle of SDA resembles DNA excision DNA repair.9 In the presence of a single strand nick on a double stranded DNA molecule, the nicked strand will be prejudicially displaced by a newly synthesized DNA strand. If it were possible to create a nick repeatedly at the same location, displaced DNA strands of the same size could then be produced continuously. To accomplish this goal, an endonuclease restriction enzyme Hindi or BsoBl is used, which only nicks DNA on one strand of its recognition site (5'-GTTGAC-3') when the opposite strand is hemiphosphorothiolated (DNA contains dATPαS instead of dATP) during DNA synthesis. The primers used in this method contain this particular recognition site and are designed in such a way that the size of the displaced strand will be the same as the target. Therefore, the displaced DNA strands can also be used as templates for subsequent reactions. Repetition of this nicking and displacement cycle will result in a geometric accumulation of the synthetic product with approximately a 10^sup 8^-fold amplification within two hours. Although this method has the potential to be used in diagnosis of many diseases such as HIV-I and Mycobacterium spp, no commercial tests have yet been marketed.
Qβ-replicase amplified probe assay
Qβ-replicase amplified probe assay is another probe-based amplification method. This method takes advantage of a unique feature of the bacteriophage Qβ-replicase, which replicates only those RNA substrates with a specific secondary structure. Therefore, by incorporating a target-specific probe into a Qβ-replicase substrate, not only does this probe-containing substrate hybridize to the gene target, but the Qβ-replicase specifically amplifies only the hybridized RNA substrates. Unhybridized probes will be removed upon RNaseIII treatment. Using this method, one copy of the target could be amplified into 10^sup 9^ copies with 30 minute incubation. The use of Qβ-replicase amplified probe assay has been described previously by Gene-Track Inc. for the detection of HIV, C. trachomatis, M. avium, and M. tuberculosis. However, no commercial kits are yet available using this technology.
SIGNAL-BASED AMPLIFICATION
Branched DNA (bDNA)
The bDNA method is a probe-based amplification assay developed by Chiron Diagnostics and currently owned by Bayer Inc. It may be used to detect both DNA and RNA targets. Several hybridization steps are incorporated in this method. After DNA or RNA extraction and denaturation of the target, the first hybridization step is to position the target using a capture probe attached to a solid surface. Once the target is captured, a second probe (extender probe) is used to hybridize to the target at an adjacent sequence in relation to the first hybridizing region. An amplification multimer (branched DNA) which is homologous to the extender probe will then attach to the extender. Alkaline phosphatase-labeled oligonucleotides will stick to these branches with 3,000 to 22,380 branch sites per target molecule. This branched tree type complex can be detected using chemiluminescence. This technique is advantageous in that the assay is simple to perform with a low inherent variability and limited carry-over contamination. Although a larger number of assays can be performed per day, the turn around time is significantly longer than PCR-based assays. This may be an important factor in situations where results are required quickly. The bDNA-based diagnostic tests are available under the trade marker of Quantiplex(TM) or Versant® through Bayer Inc. for the detection of various infections including HIV, HBV, HCV, and CMV
OTHER GENE AMPLIFICATION TECHNOLOGIES
There are a number of new emerging technologies that have not yet been applied to clinical testing, but may prove to be very useful tools in future gene diagnostics. Only two particular technologies are discussed in the following.
Immuno-PCR (IPCR)
Immuno-PCR is a new emerging technique that combines the versatility of the well-established ELISA methodology with the amplification power of real-time PCR.10,11 However, it detects proteins instead of nucleic acids. For example, IPCR has been used for quantification of HIV-I p24 antigenemia.12 In this assay, signal DNA molecules are attached to the antip24 antibody. While p24 antigens are detected by anti-p24 antibody using ELISA, the number of bound antigen-antibody complexes is quantified by real-time PCR amplification of the signal DNA molecules. Testing of patient samples by using this assay detected p24 antigen at the femtogram (fg) level, which is at least 10^sup 3^ more sensitive than conventional ELISA assays. Although IPCR could in principle become one of the most sensitive diagnostic tools, it is technically difficult to create the antibody-DNA conjugates. There are also increasing concerns about the substantial backgrounds it generates due to nonspecific binding of the antibody-DNA conjugates to the solid phases. Thus the actual utility of this methodology in clinical diagnostics is yet to be seen.
Bio-barcode assay (BCA)
Nanotechnology is making another wave of revolution in the diagnostics industry.13 The combination of nanotechnology and diagnostic biology creates an unprecedented and innovative way to detect biological molecules at an extreme low level, providing the potential for a generation of a variety of new and much more sensitive diagnostic tests. One of the nanotechnology-based techniques, known as bio-barcode amplification (BCA), can potentially detect multiple disease targets in a single clinical sample simultaneously.14 This new technology detects both protein and nucleic acids and is based on capture of protein or nucleic acids by magnetic gold nanoparticles.15 For the detection of a DNA gene target, for example, each magnetic gold nanoparticle (approximately 30 nanometers in diameter) is attached to hundreds to thousands of gene-specific oligonucleotides. These gene-specific nanoparticles can capture the gene of interest by sandwiching the DNA between two particles. The 'particle-DNA-particle' sandwich is then removed magnetically for final DNA recognition and quantification. Since each nanoparticle is coated with thousands of signal oligonucleotides, it thus automatically amplifies each of the DNA molecules by at least a thousand-fold. Because the DNA molecules are collected by magnetic enrichment, the BCA offers extreme high detection sensitivity with its limit at approximately 500 zeptomolar (zM) target DNA, i.e., less than 500 molecules per milliliter of solution.14 BCA has also been tested in the detection of amyloid-β-derived diffusible ligands (ADDLs), a protein marker that can be used to diagnose onset of Alzheimer's disease.16 Normally the ADDL concentration in brain or CSF is too low to be detected (
Genomics and proteomics in molecular diagnostics
Development of microarray technology now enables us to scan genome-wide genetic changes at the DNA, RNA, or protein levels. For example, DNA sequencing arrays are designed for simultaneous determination of multiple nucleotide sequences of interest. This approach is suitable for SNP detection of multiple genes, which could allow us to detect multiple mutations that contribute to a specific disease or predisposition of multiple diseases. Expression arrays are used for detection of changes at the gene transcriptional levels such as mRNA expressed in a tissue. Since tumorgenesis is typically die result of accumulating changes of gene expression or mutations, persistent changes in gene expression levels such as activation of oncogenes or loss of tumor suppressor gene expressions could be a strong indication of onset of cancerous cellular growth. Golub and colleagues were among the first to use gene expression profiling to distinguish acute myeloid leukemia (AML) from acute lymphoblastic leukemia (ALL).17 Similarly, comparison of protein abundance or searching for subsets of proteins linking to a specific disease (protein profiling) at the genome-wide scale offers additional power to evaluate potential pathological changes in a patient, e.g., onset of cancer. Typically, combined use of multiple techniques is needed to decipher the complex nature of these datasets generated by genomic or proteomic methods. For example, to identify protein biomarkers that link to a specifie disease, combined use of artificial-intelligence-based informatic algorithms for data mining and matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF-MS) for protein identification are needed. An increasing number of studies that utilize these strategies to identify subsets of genes or proteins as biomarkers for variety of cancers are available, such as melanoma, ovarian cancer, oral cancer, and colorectal cancer.18"21 Regardless of their high potential in molecular diagnostics, the use of genomic and proteomic biomarkers for earlier detection and risk assessment of genetic diseases has not reached the level of confidence required for clinical practice. There is an ongoing nation-wide effort coordinated by the National Cancer Institute's Early Detection Research Network (EDRN); its specific goal is to identify, validate, and implement specific cancer biomarkers for the earlier detection and risk assessment of cancers by using various genomic and proteomic approaches. It is hopeful that some of the future discoveries will soon lead to diagnostic tests that can be used in the clinic setting.
Single-cell diagnostics
Current diagnostic specimens such as blood or biopsy samples normally contain a mixture of cell types. Because many diseases such as cancers may initiate from a single cell type or even start with a single cellular event, early detection of cancer or monitoring anti-cancer therapy requires precise molecular diagnostics at the level of pure cell population or possibly in a single cell. However, procurement of a pure cell population from clinical specimens has been hampered by the lack of suitable technical tools. Development of the laser capture microdis section (LCM) technique now enables us to isolate a specific cell subtype or even a single cell under the microscope.22 Thus combining the analytic power of molecular-based testing and the LCM cell isolation technique, molecular diagnostics is now elevated to a whole different level. For example, by using the single-cell complementary DNA array and LCM, we are now capable of analyzing gene or protein profiles of two adjacent cell types within a single tissue such as a tumor. Even though molecular diagnosis at the single-cell level is not yet a reality in the clinical setting, analysis of single-cell genetic changes using the proven techniques should provide insights into the molecular pathology underlying many of the human diseases and thus promises more precise disease diagnosis. For more detailed reviews of this subject, see references.23,24
SUMMARY
In the last two decades, we have experienced explosive growth in the number and variety of new gene-based amplification and detection technologies, revolutionizing our ways of conducting clinical diagnosis and practicing medicine. However, as with any other new technologies, gene-based amplification and detection technologies have their own strengths and pitfalls. The obvious advantages of these technologies are that they are rapid, specific, and highly sensitive, involving direct detection from clinical specimens and avoiding the need for laboratory cultivation. As a result, the turn-around time is rapid. Even though the cost of these tests on a per test basis is relatively high at present, the quick turn-around time allows timely treatment for many life-threatening diseases. This minimizes the time of hospital stay and therefore reduces the overall cost.
The shortcomings of these new technologies, however, are potential false positives due to carry-over contamination or false negatives due to inhibitory effect on gene amplification. These potential technical errors could have significant impact on clinical care. Despite the obvious advantages and power the new gene diagnostic techniques can offer us, it would be a mistake to assume that they can replace the conventional diagnostic techniques. Rather than replacing the conventional methods of diagnostic testing such as classical microbiological methods, gene-based amplification technologies should serve as an adjunct to those methods and as a more rapid and less cumbersome alternative for clinical diagnosis. Overall, these new gene-based diagnostic technologies will undoubtedly significantly expand and expedite our ability in daily clinical diagnostics. Future implementation of genomic and proteomic approaches in clinical testing especially in pure cell type or at the single-cell level will undoubtedly expand our repertoires in clinical testing. Some of the current and future new diagnostic techniques will eventually become mainstream tools in clinical diagnostics and may very well replace some conventional diagnostic methods.
REFERENCES
1. Saiki RK, Scharf S, Faloona F, and others. Enzymatic amplification of beta-globin genomic sequences and restriction site analysis for diagnosis of sickle cell anemia. Sci 1985:230:1350-4.
2. Mild Y, Swensen J, Shattuck-Eidens D, and others. A strong candidate for the breast and ovarian cancer susceptibility gene BRCAl. Sci 1994:266:66-71.
3. Marx J. A second breast cancer susceptibility gene is found. Sci 1996:271:30-1.
4. Michalet X, Pinaud FF, Bentolila LA, and others. Quantum dots for live cells, in vivo imaging, and diagnostics. Sci 2005;307:538-44.
5. Holland P, Abramso R, Watson R, Gelfand D. Detection of specific polymerase chain reaction product by utilizating the 5' - 3' exonuclease activity of Thermus aquaticus DNA polymerase. Proc Natl Acad SciUSA. 1991:88:7276-80.
6. Zhao Y, Yu M, Miller JW, and others. Quantification of human immunodeficiency virus type 1 proviral DNA by using TaqMan technology. J Clin Microbiol 2002;40:675-8.
7. Tyagi S, Kramer FR. Molecular beacons: probes that fluoresce upon hybridization. Nat Biotechnol. 1996;14:303-8.
8. Thelwell N, Millington S, Solinas A, and others. Mode of action and application of Scorpion primers to mutation detection. Nucleic Acids Res. 2000;28:3752-61.
9. Walker GT, Fraiser MS, Schram JL, and others. Strand displacement amplification-an isothermal, in vitro DNA amplification technique. Nucleic Acids Res 1992;20:1691-6.
10. Sano T, Smith CL, Cantor CR. Immuno-PCR: very sensitive antigen detection by means of specific antibody-DNA conjugates. Sci 1992;258:120-2.
11. Niemeyer CM, Adler M, Blohm D. Fluorometric polymerase chain reaction (PCR) enzyme-linked immunosorbent assay for quantification of immuno-PCR products in microplates. Anal Biochem. 1997:246:140-5.
12. Barletta JM, Edelman DC, Constantine NT. Lowering the detection limits of HIV-I viral load using real-time immuno-PCR for HIV-I p24 antigen. Am J CHn Pathol. 2004;122:20-7.
13. Vo-Dinh T. Nanobiosensors: probing the sanctuary of individual living cells. J Cell Biochem Suppl. 2002:39:154-61.
14. Nam JM, Stoeva SI, Mirkin CA. Bio-bar-code-based DNA detection with PCR-like sensitivity. J Am Chem Soc. 2004;126:5932-3.
15. Taton TA1 Mirkin CA, Letsinger RL. Scanometric DNA array detection with nanoparticle probes. Sd 2000;289:1757-60.
16. Georganopoulou DG, Chang L, Nam JM, and others. Nanoparticle-based detection in cerebral spinal fluid of a soluble pathogenic biomarker for Alzheimer's disease. Proc Natl Acad Sci USA. 2005;102:2273-6.
17. Golub TR, Slonim DK, Tamayo P, and others. Molecular classification of cancer: class discovery and class prediction by gene expression monitoring. Sci 1999:286:531-7.
18. Clark EA, Golub TR, Lander ES, Hynes RO. Genomic analysis of metastasis reveals an essential role for RhoC. Nature. 2000;406:532-5.
19. Ismail RS, Baldwin RL, FangJ, and others. Differential gene expression between normal and tumor-derived ovarian epithelial cells. Cancer Res. 2000;60:6744-9.
20. Alevizos I, Mahadevappa M, Zhang X, and others. Oral cancer in vivo gene expression profiling assisted by laser capture microdissection and microarray analysis. Oncogene. 2001;20:6196-204.
21. Hegde P, Qi R, Gaspard R, and others. Identification of tumor markers in models of human colorectal cancer using a 19,200-element complementary DNA microarray. Cancer Res. 2001;61:7792-7.
22. Emmert-Buck MR, Bonner RF, Smith PD, and others. Laser capture microdissection. Sci 1996;274:998-1001.
23. Player A, Barrett JC, Kawasaki ES. Laser capture microdissection, microarrays and the precise definition of a cancer cell. Expert Rev MoI Diagn 2004;4:831-40.
24. Kawasaki ES. Microarrays and the gene expression profile of a single cell. Ann N Y Acad Sd 2004; 1020:92-100.
Richard Y Zhao PhD is an Associate Professor of Pathology, Microbiology-Immunology, and Human Virology; Division Head of Molecular Pathology; and Director, Molecular Diagnostics Laboratory, University of Maryland Medical Center, Baltimore MD,
Address for correspondence: Richard Y Zhao PhD, Department of Pathology, University of Maryland School of Medicine, 10 South Pine Street, MSTF 70OA, Baltimore MD 21201-1192. (410) 706-6301, (410) 706-6302 (fax). rzhao@som. umaryland.edu
Richard Y Zhao PhD is the Focus: Gene-based Diagnostics guest editor.
Focus Continuing Education Credit: see pages 280 to 283 for learning objectives, test questions, and application form.
Copyright American Society for Clinical Laboratory Science Fall 2005
Provided by ProQuest Information and Learning Company. All rights Reserved