Over the past 50 years, advances in the understanding of the pathophysiology and epidemiology of hypertension, in parallel with research by the pharmaceutical industry, have led to an explosion in cardiovascular pharmacology. Today, physicians can choose from six broad classes of antihypertensive agents grouped according to mechanism of action: diuretics, sympatholytics (including central and peripheral adrenergic receptor blockers), direct vasodilators, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors and the newest class, the angiotensin II receptor antagonists. Each of these drug classes contains several agents that, despite having a common basic mechanism, may differ enough in pharmacokinetics and ancillary properties to have a different pharmacologic profile in terms of indications, contraindications and side effects (Table 1).
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
The rationale for treating a virtually asymptomatic disease such as essential hypertension is to prevent its cardiovascular complications. The relationship between antihypertensive drug therapy and complication prevention was established by the landmark U.S. Veterans Administration studies conducted in the 1960s. Epidemiologic surveys have consistently demonstrated that optimal blood pressure control can significantly diminish the rate of most hypertensive complications, including stroke, renal failure, congestive heart failure and hypertensive retinopathy.
Less evidence is available to show a relationship between blood pressure control and a reduction in coronary artery disease.[1] After comparing the mechanisms involved in essential hypertension and ischemic heart disease, investigators have provided several possible explanations. According to one theory, both disorders evolve in parallel from a common etiology, so that treatment of one may not necessarily prevent the other unless a common pathogenic mechanism is affected. Alternatively, it is possible that therapeutic interventions against hypertension tend to aggravate some of the known coronary risk factors, partially offsetting the benefits of blood pressure reduction.
The goals of antihypertensive therapy are to lower blood pressure with minimal inconvenience to the patient and to maximize the chance of preventing the cardiovascular, cerebrovascular, renal and metabolic complications of hypertension. The choice of appropriate antihypertensive drug therapy is based on many considerations, including the patient's risk factors and coexisting diseases.
Diuretics
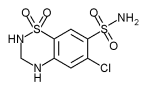
The diuretics class of antihypertensive agents includes the distal tubule diuretics such as thiazides and related drugs, including metolazone (Zaroxolyn) and indapamide (Lozol), and the loop diuretics such as furosemide (Lasix), bumetanide (Bumex) and ethacrynic acid (Edecrin).
Loop diuretics are used only in patients with congestive heart failure or renal failure, because these short-acting agents are less effective than other diuretics in controlling blood pressure and tend to produce abrupt shifts in the water and electrolyte balance. Recently, torsemide (Demadex) was added to the subclass of loop diuretics. Torsemide is a long-acting agent more useful for the treatment of chronic hypertension.
Thiazides were the first diuretic agents found to be suitable for smooth and dependable long-term blood pressure control. These diuretics, either alone or in combination with other agents, are still the most widely used antihypertensive drugs.
An important advantage of diuretics is that they cost less than the newer antihypertensive agents. Since diuretics were used in all of the initial trials that demonstrated diminished mortality with good blood pressure control, they have remained the gold standard against which the efficacies of all newer drugs are compared.
In low doses, such as 12.5 mg per day of hydrochlorothiazide (Esidrix, Hydrodiuril, Oretic, etc.) or an equivalent agent, thiazides can be effective as monotherapy in elderly patients and in patients with milder hypertension. Because of the small daily dose, such patients are unlikely to have significant side effects. Indeed, several multicenter trials[2,3] have shown that chronic low-dose diuretic therapy in elderly patients diminishes the rate of all cardiovascular complications, including coronary events.
In higher doses, thiazides are likely to cause adverse reactions such as hypokalemia, hyperuricemia, hyperglycemia, dyslipidemia and orthostatic intolerance. Therefore, patients receiving these drugs require close monitoring and remedial interventions. It is theorized that some of the metabolic effects and their consequences (e.g., arrhythmia,[4] diabetes mellitus,[5] etc.) may account for the fact that in various multicenter trials,[6] the incidence of coronary disease was not found to be significantly decreased with thiazide diuretics, despite good blood pressure control. Other hypertensive complications have, however, been favorably affected by treatment with these drugs.
The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V)[7] recommended diuretics and beta-adrenergic receptor blockers as the agents of first choice for initial antihypertensive drug therapy The rationale was that both diuretics and beta blockers are safe, effective and less costly than newer antihypertensive agents and that they were the only drugs shown to reduce morbidity and morality from hypertension in the placebo-controlled, prospective trials of the 1960s and 1970s.
Several authorities in the field took exception to the JNC V recommendation,[8] which touched off a still ongoing debate. These investigators pointed out that the reduced morbidity and mortality in the early trials was attributable to blood pressure lowering per se and not to effects of specific drugs. Since it would not be ethical to conduct placebo-controlled studies today, all subsequently developed drugs are compared with thiazides and are considered acceptable if they are found to be at least as effective as diuretics. The newer antihypertensive agents, however, possess metabolic advantages that theoretically may confer additional cardioprotection.
The present controversy will not be resolved until a study funded by the National Institutes of Health is completed in the year 2002. This study -- the Antihypertensive and Lipid Lowering Heart Attack Prevention Trial (ALLHAT) -- is prospectively comparing various classes of antihypertensive agents in 40,000 hypertensive patients over 55 years of age.
Nevertheless, diuretics are still generally accepted as first-choice drugs for the treatment of hypertension in black patients (because these patients do not respond well to monotherapy with a beta blocker or an ACE inhibitor), as well as in elderly patients and patients with mild hypertension, who, as mentioned previously, may respond to very low doses. Diuretics are also extremely useful as second- or third-line drugs given in combination with a beta blocker or with an ACE inhibitor and an angiotensin II antagonist. Since diuretics have additive effects with beta blockers and synergistic effects with ACE inhibitors and angiotensin II receptor antagonists, a smaller dose of each drug may be used. In contrast, the effect may be less than additive when a diuretic is given in combination with a calcium channel blocker.[9]
Sympatholytics
BETA-ADRENERGIC RECEPTOR BLOCKERS
Beta blockers, the most widely used sympatholytics, were part of the regimen used in several of the early multicenter trials that demonstrated the benefits of blood pressure lowering. Individual agents in this subclass may vary in potency, duration of action, lipophilicity or hydrophilicity, cardioselectivity, and the presence or absence of intrinsic sympathomimetic activity.
All beta blockers are effective as monotherapy in about 50 percent of unselected patients with mild to moderate hypertension, although they are somewhat less effective in black and elderly patients. In addition, these agents all share the basic pharmacodynamic characteristics of beta blockade, including, in addition to blood pressure lowering, a tendency to cause peripheral vasoconstriction (hence the potential for clammy extremities and precipitation of attacks of Raynaud's disease), negative inotropic and chronotropic action on the heart, bronchoconstriction, and accentuation of insulin resistance with the attendant metabolic consequences (i.e., tendency to develop hyperglycemia and dyslipidemia).
Beta blockers are particularly suited to the treatment of hypertension coexisting with angina, arrhythmias, migraine and other conditions that also benefit from beta blockade. Beta blockers, especially the ones that do not have intrinsic sympathomimetic activity, are indicated in patients following myocardial infarction, because these drugs have been shown to prevent recurrent infarction and sudden death.[10]
Treatment with beta blockers generally is not recommended for patients who are susceptible to bronchospasm, peripheral arterial insufficiency, congestive heart failure, brittle diabetes mellitus or bradyarrhythmia.
In selected cases, individual drug characteristics may make one beta blocker a better choice than another agent from the same subclass. For example, a beta blocker with intrinsic sympathomimetic activity may be better tolerated by a patient with sick sinus syndrome or a patient with a history of bronchial asthma but no current obstructive pulmonary disease. However, the same agent would be less effective in a patient with coronary artery disease, especially following myocardial infarction.
Beta blockers are also useful in combination with a diuretic, a dihydropyridine-type calcium channel blocker or an ACE inhibitor. For more severe cases, beta blockers may be given in a three-drug combination with a diuretic and a direct vasodilator. Because of significant negative inotropic and chronotropic effects, verapamil (Calan, Isoptin, Verelan) and other calcium channel blockers should be used with caution in combination with a beta blocker. This combination should be avoided in patients with compromised myocardial contractility or atrioventricular conduction.[11]
[ALPHA.sub.1]-ADRENERGIC RECEPTOR BLOCKERS
Drugs that block peripheral [alpha.sub.1]-adrenergic receptors are effective vasodilators with some bronchodilatory activity. They are metabolically neutral or, possibly, beneficial.[12] This sympatholytic subclass includes the short-acting agent prazosin (Minipress) and the long-acting agents terazosin (Hytrin) and doxazosin (Cardura).
Although not usually selected as first-line monotherapy, [alpha.sub.1]-adrenergic receptor blockers are a particularly good choice in patients with coexisting conditions that may benefit from alpha blockade, such as congestive heart failure, asthma, peripheral arterial obstructive disease, impotence and benign prostatic hypertrophy. The main limitation to their use is their tendency to cause orthostatic hypotension after the initial dose.
Since these medications do not interfere with the mechanism controlling norepinephrine release, they usually do not cause palpitations or tachycardia.[13] Because of their beneficial effect on serum lipid levels and their ability to reduce insulin resistance, [alpha.sub.1]-adrenergic receptor blockers may be useful in obese patients with hypertension.[14]
Labetalol (Normodyne, Trandate) is a unique drug that has both alpha- and beta-blocking properties. This agent may be effective as monotherapy when hypertension does not respond to either alpha blockade or beta blockade alone. In addition, labetalol can be administered parenterally in urgent or emergency situations related to hypertension or during surgical situations in which oral antihypertensive treatment is not feasible. Combined alpha and beta blockers may be preferred as first-line therapy in black patients with hypertension.
CENTRAL SYMPATHOLYTIC AGENTS
This subclass includes some of the earliest antihypertensive agents, such as reserpine (Serpasil), methyldopa (Aldomet) and clonidine (Catapres). These agents are no longer widely used because they depress the central nervous system, causing fatigue, lethargy, cognitive impairment and psychosocial problems. However, central sympatholytic agents may be useful in selected patients who do not respond to other antihypertensive drugs or are unable to tolerate them.
Clonidine, in particular, is helpful in patients with hypertension that has a large neurogenic component. Included in this group are patients prone to panic attacks, patients experiencing drug or alcohol withdrawal or hypoglycemic episodes, and patients subjected to various manipulations in intensive care (i.e., intubation, ventilation, suction, etc.). In such cases, inhibition of excessive central sympathetic outflow is desirable.[15] Clonidine patches for transdermal administration may be useful for patients with diabetes and gastroplegia, in whom oral drug absorption may be erratic. The patches may also be beneficial in hypertensive elderly patients evaluated weekly by a visiting nurse who monitors their medications.
Methyldopa is the drug of choice for hypertension associated with pregnancy. Since this drug is a category B medication (i.e., there is no evidence of risk in humans), it is considered safe for both mother and fetus.
Peripheral Arterial Dilators
Drugs that act directly on the arteriolar smooth muscle to produce vasorelaxation include hydralazine (Apresoline) and minoxidil (Loniten), as well as parenterally administered diazoxide (Hyperstat) and sodium nitroprusside (Nitropress). Although these agents are especially effective in decreasing diastolic blood pressure, they are not used as monotherapy because they tend to produce reflex stimulation of the sympathetic nervous system and the renin-angiotensin-aldosterone axis, causing both tachycardia and salt and fluid retention.
Peripheral arterial dilators are useful when they are given with a sympatholytic and a diuretic as part of three-drug combinations in patients with severe, resistant hypertension.[7] However, hydralazine in either oral or parenteral form is safe and suitable as monotherapy for toxemia of pregnancy, because reflex tachycardia is easily tolerated by young women who do not have coronary insufficiency. Hydralazine is considered a category C drug, which means that although risk cannot be ruled out, the benefits of therapy may justify the potential risks associated with treatment.
The parenterally administered combination of hydralazine and a beta blocker such as propranolol (Inderal) or metoprolol (Lopressor) is one of the preferred treatments for aortic dissection. Sodium nitroprusside combined with a beta blocker is another alternative for this condition, instead of the previously used trimethaphan (Arfonad), a ganglionic blocker that can cause complications from glaucoma, urinary retention and other disorders.
Sodium nitroprusside infusion in combination with a diuretic and a sympatholytic agent is still the treatment of choice for accelerated or malignant hypertension. This therapy permits the controlled lowering of blood pressure to the desired level.
Calcium Channel Blockers
The calcium channel blockers constitute one of the newer classes of antihypertensive drugs. These agents became popular because they lower blood pressure in all patients (regardless of age, race or sex). Furthermore, they have no metabolic side effects, and they are associated with relatively few adverse reactions (primarily constipation and dependent edema).
Verapamil and diltiazem (Cardizem, Dilacor XR, Tiazac) have a more pronounced negative inotropic and chronotropic effect, whereas the large subclass of dihydropyridine derivatives, including nifedipine (Adalat CC, Procardia XL), amlodipine (Norvasc) and felodipine (Plendil), are more "vasoselective" and act mostly as peripheral vasodilators.
The calcium channel blockers are particularly indicated in hypertensive patients with symptomatic coronary insufficiency, such as exertional angina or arrhythmias.[7] After myocardial infarction, however, the long-term results using these agents are favorable only in patients who have maintained good systolic myocardial capacity (as indicated by an ejection fraction of over 40 percent). Calcium channel blockers may also be suitable in patients with concurrent conditions, such as asthma, peripheral vascular insufficiency, diabetes mellitus or lipid disorders, that may preclude the use of other antihypertensive drugs.
Calcium channel blockers are metabolically neutral, and they may have an antiatherogenic action. However, these properties may not necessarily be sufficient to confer long-term cardioprotection. Indeed, it has recently been suggested that patients with no preexisting cardiac disease appear to be at higher risk for coronary events if they are treated with the combination of a calcium channel blocker and a diuretic than if they were treated with a diuretic alone or with the combination of a calcium channel blocker and a beta blocker or an ACE inhibitor.[16]
It should be noted that these were retrospective surveys involving patients who were taking mostly short-acting calcium channel blockers, which are contraindicated for the treatment of chronic hypertension. Until the controlled trials now in progress can provide further guidance, it is recommended that patients with indications for calcium channel blockers, such angina, continue taking these medications, although they should be given the long-acting forms or the newer dihydropyridines.
Ace Inhibitors
ACE inhibition results in suppression of the vasoconstrictor angiotensin II, as well as potentiation of the vasodilator bradykinin. This vasodilator, in turn, stimulates a number of "tissue hormones," including prostaglandins and nitric oxide. Angiotensin suppression results in vasodilation with preferentially enhanced perfusion of vital organs (kidneys, heart and brain) that have a vasculature which is more sensitive to angiotensin II, the suppression of aldosterone, the reversal of cardiac and vascular hypertrophy related to hemodynamic improvement, and the withdrawal of the growth-promoting properties of angiotensin.[17] Bradykin potentiation resulting from ACE inhibition causes enhanced insulin sensitivity, preferential renal and coronary vasodilation, and both antithrombotic and antiatherogenic effects attributable to the activation of various tissue mediators.[17]
These agents are effective as monotherapy in 50 to 60 percent of unselected patients and in 80 percent of patients after diuretics are added to the regimen.[18] Diuretics render the blood pressure more "renin-dependent." ACE inhibitors are particularly indicated in patients with various degrees of left ventricular dysfunction, ranging from subclinical diastolic dysfunction to chronic congestive heart failure caused by systolic dysfunction (as indicated by an ejection fraction of less than 40 percent). These agents are also strongly indicated in patients who have had a myocardial infarction. Several multicenter trials have shown that, in such patients, ACE inhibition exerts a cardioprotective action, thereby reducing cardiac morbidity and mortality.[19]
While animal and clinical experiments seem to indicate that ACE inhibitors have a primary cardioprotective action, this has not yet been proven in long-term studies comparing these agents with other antihypertensive drugs. Nevertheless, in patients with left ventricular dysfunction, ACE inhibitors appear to lower the rate of heart attacks by about 25 percent.[20]
ACE inhibitors have been shown to slow the onset or progression of nephropathy in patients with type I diabetes mellitus.[21] These agents are equally effective in younger and older patients.[22] ACE inhibitors are less effective as monotherapy in black patients with hypertension, but they become more effective when they are given as combined therapy with a diuretic.[22] However, when used in this combination, ACE inhibitors tend to attenuate the metabolic side effects of thiazides, including hypokalemia, hyperuricemia and hyperglycemia. While fixed ACE inhibitor-thiazide combinations are convenient to use in many patients, the dose of each agent must be titrated appropriately and separately first.
The ACE inhibitors generally have a favorable side effect profile. In contrast to the recommendations of the JNC V, some authorities believe that, in the absence of specific indications for another agent, ACE inhibitors are a good choice for the initiation of antihypertensive therapy in unselected patients.[8] The most common reason patients cannot tolerate ACE inhibitors is that they cause a ticklish dry cough, which is thought to be a bradykinin-mediated effect.[17] The incidence of cough ranges from 5 to 20 percent, varying with the patient population. Cough related to ACE inhibitors occurs more frequently in older, female, white or Oriental patients and in patients with congestive heart failure. Infrequently, ACE inhibitors may cause hyperkalemia (especially in older patients with renal insufficiency) and, extremely rarely, angioedema. All of these side effects are likely to recur if the patient is given another drug from the class. However, side effects such as rashes, allergic reactions or blood dyscrasias are not likely to recur if a patient is switched from one ACE inhibitor to a different agent in that class.
No pharmacologic characteristics make one ACE inhibitor clearly preferable to another in clinical practice, so drug selection is based on the physician's experience with the various ACE inhibitors, the convenience of administration (e.g., number of daily doses) and the cost of therapy. Theoretically, fosinopril (Monopril) may be preferable in patients with chronic renal failure, because it is eliminated in part by the biliary route. However, these patients can be given another ACE inhibitor as long as the dose is appropriately lowered to prevent excessive drug accumulation.
Captopril (Capoten), the only short-acting ACE inhibitor, is useful for initial titration when the physician does not know if ACE inhibition can be tolerated by a patient with, for example, congestive heart failure or renal artery stenosis. For chronic maintenance therapy, the patient can then be switched to one of the long-acting ACE inhibitors, which are suitable for once-daily dosing.
Angiotensin II Receptor Antagonists
In the early 1970s, polypeptide analogs of angiotensin were used extensively in clinical trials on the treatment of hypertension and congestive heart failure. With analogs such as saralasin, it was first demonstrated that the inhibition of angiotensin II has beneficial hemodynamic effects in both congestive heart failure and hypertension.[23,24] However, because these analogs were extremely short-acting, they had to be administered in a continuous intravenous infusion, which made them impractical for clinical use.
Orally administered long-acting nonpeptide inhibitors of angiotensin II have recently become available.[25] The first member of this class, losartan (Cozaar), was approved by the U.S. Food and Drug Administration in 1995. Other such agents should be approved in the near future. These drugs selectively block the angiotensin type 1 receptors of angiotensin II and inhibit the actions of the hormone. Their systemic hemodynamic effects are similar to those of ACE inhibitors, meaning that they are effective in lowering peripheral vascular resistance while preferentially maintaining or increasing perfusion of the vital organs, which are particularly sensitive to the vasoconstrictive action of angiotensin.[26]
Early clinical experience with losartan has demonstrated its efficacy in the treatment of hypertension and congestive heart failure.[27,28] Experimental and clinical studies have confirmed that, in both of these conditions, losartan and ACE inhibitors induce a similar pattern of systemic hemodynamic responses.[26,29] As with ACE inhibitors, the antihypertensive effect of angiotensin II antagonists is markedly potentiated when they are administered with a diuretic. The main advantage of angiotensin II antagonists over ACE inhibitors is the lack of undesirable side effects attributed to the potentiation of bradykinin, specifically, cough[17] and angioedema. Accordingly, drugs in this class should be able to confer the long-term cardioprotective and renoprotective benefits of chronic angiotensin blockade, and they should be better tolerated than ACE inhibitors.
Final Comment
Any one drug started as monotherapy is likely to control blood pressure in 50 to 60 percent of patients with mild to moderate hypertension. The majority of these patients are likely to continue on the same treatment for many years (often, for life). Therefore, the choice of the most appropriate initial treatment for a particular patient should be made by matching the pharmacologic properties of drugs with the short-term and long-term goals of antihypertensive therapy as defined by the patient's individual characteristics. This is the so-called "tailored approach," as opposed to the standardized "step-care" approach advocated in the past.
When there are no special indications for a particular agent, the JNC V recommends initiating therapy with either a diuretic or a beta blocker. Additional drugs are introduced, if necessary, to achieve optimal blood pressure control, keeping in mind that the best combinations are those with synergistic actions or with the capacity to offset one another's adverse effects.
REFERENCES
[1.] Herbert PR, Moser M, Mayer J, Glynn RJ, Hennekens CH, et al. Recent evidence on drug therapy of mild to moderate hypertension and decreased risk of coronary heart disease. Arch Intern Med 1993;153:578-81.
[2.] Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991;265:3255-64.
[3.] Dahlof B, Lindholm LH, Hansson L, Schersten B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet 1991;338:1281-5.
[4.] Siscovick DS, Raghunathan TE, Psaty BM, Koepsell TD, Wicklund KG, Lin X, et al. Diuretic therapy for hypertension and the risk of primary cardiac arrest. N Engl J Med 1994;330:1852-7.
[5.] Pollare T, Lithell H, Berne C. A comparison of the effects of hydrochlorothiazide and captopril on glucose and lipid metabolism in patients with hypertension. N Engl J Med 1989;321:868-73.
[6.] MacMahon SW, Cutler JA, Furberg CD, Payne GH. The effects of drug treatment for hypertension on morbidity and mortality from cardiovascular disease: a review of randomized controlled trials. Progr Cardiovasc Dis 1986;29(3 Suppl 1):99-118.
[7.] The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1993;153:154-83.
[8.] Tobian L, Brunner HR, Cohn JN, Gavras H, Laragh JH, Materson BJ, et al. Modern strategies to prevent coronary sequelae and stroke in hypertensive patients differ from the JNC V Consensus Guidelines. Am J Hypertens 1994;7(10 Pt 1):859-72.
[9.] Muller FB, Bolli P, Linder L, Kiowski W, Erne P, Buhler FR. Calcium antagonists and the second drug for hypertensive therapy. Am J Med 1986; 81(6A):25-9.
[10.] Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 1985;27:335-71.
[11.] Packer M, Meller J, Medina N, Yushak M, Smith H, Holt J, et al Hemodynamic consequences of combined beta-adrenergic and slow calcium channel blockade in man. Circulation 1982;65:660-8.
[12.] Grimm RH Jr. Alpha 1-antagonists in the treatment of hypertension. Hypertension 1989;13(5 Suppl):131-6.
[13.] Kaplan NM, Gifford RW. Choice of initial therapy for hypertension. JAMA 1996;275:1577-80.
[14.] Maheux P, Facchini F, Jeppesen J, et al. Changes in glucose, insulin, lipid, lipoprotein and apoprotein concentrations and insulin-action in doxazosin-treated patients with hypertension: comparison between non-diabetic individuals and patients with non-insulin-dependent diabetes mellitus. Am J Hypertens 1994;7:416-24.
[15.] Onesti G, Schwartz AB, Kim KE, Swartz C, Brest AN. Pharmacodynamic effects of a new antihypertensive drug, Catapres (ST-155). Circulation 1969;39:219-28.
[16.] Psaty BM, Heckbert SR, Koepsell TD, Siscovick DS, Raghunathan TE, Weiss NS, et al. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA 1995;274:620-5.
[17.] Gavras I. Bradykinin-mediated effects of ACE inhibition. Kidney Int 1992;42:1020-9.
[18.] Gavras H. A multicenter trial of enalapril in the treatment of essential hypertension. Clin Ther 1986;9(Suppl 1):24-38.
[19.] Gavras H, Gavras I. Cardioprotective potential of angiotensin converting enzyme inhibitors [Editorial]. J Hypertens 1991;9:385-92.
[20.] Yusuf S, Pepine CJ, Garces C, Pouleur H, Salem D, Kostis J, et al. Effect of enalapril on myocardial infarction and unstable angina in patients with low ejection fractions. Lancet 1992;340:1173-8.
[21.] Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med 1993;329:1456-62 [Published erratum appears in N Engl J Med 1993;330:152].
[22.] Mulinari R, Gavras I, Gavras H. Efficacy and tolerability of enalapril monotherapy in mild-to-moderate hypertension in older patients compared to younger patients. Clin Ther 1987;9:678-89.
[23.] Brunner HR, Gavras H, Laragh JH. Specific inhibition of the renin-angiotensin system: a key to understanding blood pressure regulation. Prog Cardiovasc Dis 1974;17:87-98.
[24.] Gavras H, Flessas A, Ryan TJ, Brunner HR, Faxon DP, Gavras I. Angiotensin II inhibition. Treatment of congestive cardiac failure in a high-renin hypertension. JAMA 1977;238:880-2.
[25.] Timmermans PB, Wong PC, Chiu AT, Herblin WF, Benfield P, Carini DJ, et al. Angiotensin II receptors and angiotensin II receptor antagonists. Pharmacol Rev 1993;45:205-51.
[26.] Wang YX, Gavras I, Wierzba T, Gavras H. Comparison of systemic and regional hemodynamic effects of a diuretic, an angiotensin II receptor antagonist, and an angiotensin-converting enzyme inhibitor in conscious renovascular hypertensive rats. J Lab Clin Med 1992;119:267-72.
[27.] MacFadyen RJ, Reid JL. Angiotensin receptor antagonists as a treatment for hypertension [Editorial]. J Hypertens 1994;12:1333-8.
[28.] Gottlieb SS, Dickstein K, Fleck E, Kostis J, Levine TB, LeJemtel T, et al. Hemodynamic and neurohormonal effects of the angiotensin II antagonist losartan in patients with congestive heart failure. Circulation 1993;88(4 Pt 1):1602-9.
[29.] Goldberg MR, Bradstreet TE, McWilliams EJ, Tanaka WK, Lipert S, Bjornsson TD, et al. Biochemical effects of losartan, a nonpeptide angiotensin II receptor antagonist, on the renin-angiotensin-aldosterone system in hypertensive patients. Hypertension 1995;25:37-46.
The Authors
IRENE GAVRAS, m.d. is clinical professor of medicine at Boston University School of Medicine and attending physician at Boston Medical Center. Dr. Gavras received her medical degree from the Athens University School of Medicine and completed postgraduate training at the Evangelismos Hospital, Athens, Greece, and the Royal Infirmary, Glasgow, Scotland.
ATHANASIOS MANOLIS, m.d. is director of the hypertension clinic at Tzanion Hospital, Piraeus, Greece. A graduate of Athens University School of Medicine, Dr. Manolis completed a residency in cardiology at Tzanion Hospital and a clinical fellowship in hypertension at Boston University School of Medicine.
HARALAMBOS GAVRAS, m.d. is professor of medicine at Boston University School of Medicine, chief of the hypertension and atherosclerosis section at Boston Medical Center and director of a specialized center of research in the molecular genetics of hypertension. Dr. Gavras received his medical degree from Athens University School of Medicine and completed postgraduate training at the Western Infirmary, Glasgow, Scotland.
COPYRIGHT 1997 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group