Lipid Abnormalities and Diuretics
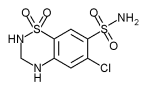
Diuretic-based treatment regimens for hypertension have consistently reduced blood pressure and the morbidity and mortality due to stroke and overall cardiovascular disease. Studies have been less consistent in showing a beneficial effect on morbidity and mortality from coronary heart disease. However, speculations that possible adverse effects of diuretics on lipids may have contributed to the lack of a consistent beneficial effect on coronary heart disease are not substantiated by long-term clinical trials. Thiazide diuretics are the most commonly prescribed drugs for the treatment of hypertension and have been recommended as possible first-step therapy by all four Joint National Committees on Detection, Evaluation and Treatment of High Blood Pressure.[1-4] Thiazide diuretics have been used as initial therapy or in combination therapy in all of the major clinical trials that have assessed the effects of blood pressure reduction on mortality and morbidity due to hypertension. The use of these agents results in consistently lower blood pressure and a reduction in overall cardiovascular morbidity and mortality.[5-11]
Trials of diuretic antihypertensive therapy have not consistently shown a beneficial effect on morbidity and mortality due to coronary heart disease. A trend toward a reduction in cardiac events has been noted in some studies.[5,8] In two studies that compared treatment groups with groups receiving placebo or less vigorous treatment,[6,7] deaths from ischemic heart disease were reported to decrease by 15 and 38 percent, respectively, in treated subjects.
The lack of consistent evidence for a reduction in cardiovascular morbidity and mortality raises several questions. Do the study results relate to the type of population studied? For example, was benefit difficult to establish in some studies because subjects were low-risk patients, as in the Australian Trial[5] and the Medical Research Council Study?[8] Or was benefit not demonstrated because the study was of too short duration? Could blood pressure reduction alone have been insufficient to delay or reverse the multifactorial atherogenic process? Were patients enrolled in the study too late in the course of their disease--that is, after vascular damage had occurred?
These questions have been discussed elsewhere,[12] but satisfactory answers have not yet been provided. One possible explanation for the lack of a consistent therapeutic effect on coronary heart disease is that the adverse effects of diuretics on lipid levels may blunt the beneficial effects of blood pressure lowering.[13] This conclusion is difficult to accept. A careful review of the literature fails to find a single long-term (more than one year) diuretic-based clinical trial in which serum cholesterol levels were significantly higher in the treated group at the end of the trial than they were at the beginning. The evidence relating to both short-and long-term effects of diuretics on lipid levels needs to be put in perspective.
Diuretic Therapy and Serum Cholesterol
Diuretic-induced elevations in serum cholesterol levels were first noted almost 25 years ago. Schoenfeld and Goldberger[14] investigated six patients with congestive heart failure who received a thiazide diuretic during a four-week period. Serum cholesterol levels increased independently from the effect on hemoconcentration and returned to baseline values following thiazide withdrawal.
SHORT-TERM STUDIES
A number of short-term studies (one year or less)[15-26] have reported the effects of thiazide diuretics on serum cholesterol concentrations (Table 1). Because lipid fractionation results were not consistently reported in many of these studies, data on total serum cholesterol concentrations are presented.
In a review of 14 short-term studies, Weidmann and colleagues[27] found that cholesterol concentrations increased an average of 7 percent when diuretic antihypertensive therapy was used. Most of these studies were of four to eight weeks duration and involved between 12 and 40 subjects.
Ames[28] reviewed 18 short-term studies of 25 or fewer patients who received either hydrochlorothiazide (Hydro DIURIL, Esidrix, Oretic, etc.) or chlorthalidone (Hygroton, Hylidone, Thalitone). High-density lipoprotein (HDL) concentrations increased in one study and decreased in two; seven studies showed a significant increase in total serum cholesterol concentrations, and three revealed an increase in low-density lipoprotein (LDL) cholesterol. Seven short-term treatment trials involving more than 25 patients showed an average increase of 5 percent in total serum cholesterol concentrations during diuretic therapy. However, in the four studies that reported HDL levels, the investigators found no change in HDL levels with thiazide diuretic therapy. These reports suggest a trend toward increased serum cholesterol concentrations following the short-term use of thiazide diuretics.
The variability of these results might be explained by the limited number of patients involved and the short duration of the trials. Serum lipid levels are known to vary considerably from week to week in the same person. The concomitant use of lipid-lowering diets and physical fitness programs during some of the study periods may also have influenced outcome. The clinical significance of the short-term, modest increase in serum cholesterol levels must be questioned.
LONG-TERM STUDIES
Numerous studies have demonstrated that significant elevations in serum cholesterol concentrations are not observed after long-term use (more than one year) of thiazide diuretics.[6,8,29-38] In the Veterans Administration Feasibility Study,[21] cholesterol levels were increased in diuretic-treated patients at one year. However, data from all of the major hypertension treatment trials that used diuretics as initial monotherapy indicate that serum cholesterol concentrations either remain the same or decrease below baseline values after one year of therapy (Table 2).
These studies, ranging from more than one year to six years, include the European Working Party on Hypertension in the Elderly (EWPHE),[7,29] the Medical Research Council (MRC),[8,38] the Veterans Administration Study,[30] the Goteborg Study,[39] the Hypertension Detection and Follow-Up Program (HDFP),[6] the Oslo Study,[9,34] the Heart Attack Primary Prevention in Hypertension (HAPPHY) Trial[40] and the Multiple Risk Factor Intervention Trials (MRFIT).[35-37]
Serum triglyceride concentrations decreased slightly but not significantly in the Veterans Administration Study[30] and in the Oslo Study.[9] The MRFIT study [35-37] showed decreases in LDL and total serum cholesterol concentrations, an increase in serum triglyceride concentrations and only minimal changes in HDL levels.
In two clinical trials (MRC and MRFIT), changes in serum cholesterol levels in the diuretic-treated subjects differed from those in nontreated subjects.[8,35-38] For example, in the MRC trial, the mean serum cholesterol level decreased from 244 to 239 mg per dL (6.32 to 6.18 mmol per L) in men in the placebo group but remained the same at 246 mg per dL (6.35 mmol per L) in men treated with high-dose diuretic therapy (equivalent to 100 mg per day of either chlorthalidone or hydrochlorothiazide).[8,38] The difference between the two groups was 7 mg per dL (0.17 mmol per L). Serum cholesterol levels in women decreased from 261 to 257 mg per dL (6.74 to 6.64 mmol per L) during treatment with placebo and from 262 to 261 mg per dL (6.77 to 6.75 mmol per L) during diuretic treatment. The difference between the two groups was 4.0 mg per dL (0.11 mmol per L). It is difficult, however, to assess the clinical relevance of these changes.
In the MRFIT study,[35-37] serum cholesterol levels decreased to a greater degree in subjects who were not receiving antihypertensive drug therapy (usually diuretics) at six years than in those who were receiving treatment. This suggests that the use of medication may have blunted the effect of the low saturated fat, low-cholesterol diet that was used in both special intervention groups.
The study involved high-risk men who had one or more risk factors, including hypertension, elevated lipid levels and cigarette smoking. In the study, those patients who were not receiving therapy at six years were either not hypertensive on initial evaluation or only mildly hypertensive at baseline (Table 3). If they were also nonsmokers, many (497 subjects) were admitted to the trial primarily because of elevated serum cholesterol concentrations.
It was in this group of subjects--nonsmokers who were not receiving antihypertensive therapy--that the greatest difference was noted in cholesterol concentrations. Significantly, this group also experienced the greatest weight loss and had higher baseline serum cholesterol concentrations than other groups. Nonsmokers were more adherent to the dietary regimen, which may explain their better lipid levels and their greater weight loss. One explanation for the difference in outcome might be that the patients and the investigators initially expended more effort in trying to correct a single major risk factor, elevated cholesterol level.
In the smokers, a difference of 6 mg per dL (0.15 mmol per L) was noted between those who received diuretics and those who did not. Baseline serum cholesterol levels were also higher in the group not receiving treatment at six years. This is the only long-term study to suggest what may be a clinically significant difference between control groups and treatment groups with respect to the effect of antihypertensive drug therapy on lipid levels--and it may have been changes in weight rather than medication that accounted for the difference.
Discussion
Although investigators have speculated that the modest elevation in serum cholesterol levels following the short-term use of diuretics may negate the benefits associated with blood pressure lowering, there is little evidence to support this premise. In the long-term studies, the rise in serum cholesterol levels did not persist. It is difficult to conclude that short-term changes in the serum cholesterol concentration, of the magnitude reported (5 to 7 percent), play a role in the development or progression of atherosclerosis.
The suggestion that a 1 percent decrease in cholesterol levels results in a 2 percent decrease in coronary heart disease deaths is based on data from the Lipid Research Clinics Study,[41] in which middle-aged high-risk men who entered the trial were treated only after laboratory evaluation revealed persistent cholesterol levels of more than 265 mg per dL (6.85 mmol per L). It may not be appropriate to extrapolate these data to the general population of men and women, especially those with lower pretreatment cholesterol levels.
In two studies that included patients who were either at high risk or elderly and whose percentage of cardiovascular events and deaths was higher than that in other studies of mild hypertension, the investigators reported a difference in ischemic heart disease events between the treated and untreated groups.[6,7] The results suggest that long-term diuretic-based therapy has a beneficial effect not only on overall cardiovascular events but specifically on coronary heart disease mortality.
In a five-year study,[6] mortality from all causes was 17 percent lower for patients in a stepped-care antihypertensive treatment program than for patients allocated to a referred-care group, who were less vigorously treated. Initial monotherapy in the stepped-care group consisted of thiazide diuretic therapy. In patients with mild hypertension, defined as a diastolic blood pressure between 90 and 104 mm Hg, mortality in the stepped-care group was 20 percent lower than that in the referred-care group. The number of deaths from cerebrovascular disease was nearly 45 percent lower in the stepped-care group than in the referred-care group, and there were 26 percent fewer deaths due to acute myocardial infarction. For all coronary heart diseases, the stepped-care group had 15 percent fewer deaths than the referred-care group.
Over 50 percent of the patients who participated in the EWPHE trial,[7] whose average age was 71 years, achieved good blood pressure control with one capsule daily of hydrochlorothiazide and triamterene. Compared with patients in the placebo group, patients who received therapy showed a 27 percent decrease in cardiovascular mortality. A recent evaluation of this study suggests that combination therapy with potassium-sparing diuretics accounted for the favorable outcome. Results could not be explained by the addition of methyldopa (Aldomet) in 42 percent of the patients.[42]
Final Comment
Repeated emphasis on the short-term effects of thiazide diuretics on serum cholesterol levels and confusion about the long-term effects have led some physicians to limit or abandon the use of these agents as initial monotherapy or in combination with other agents. This may be a mistake.[43] Data from the long-term clinical trials appear to refute the argument that diuretic-induced elevations in serum cholesterol levels account for the lack of reduction in coronary events in some of the clinical trials. Serum cholesterol levels in diuretic-treated patients were essentially the same or lower-not higher--at the end of each of the long-term clinical trials discussed in this review. Furthermore, overall cardiovascular mortality was reduced in the rigorously treated patients compared with those who were treated with placebo or a less controlled regimen. A more likely explanation for the lack of consistent reductions in coronary heart disease mortality may relate to factors in the study designs, such as inadequate population size or study duration, infrequent events in both the treated and the control groups, or patient selection bias.[44]
The MRFIT study[35-37] is often cited as having demonstrated an adverse effect of diuretic therapy on serum cholesterol levels, but it should be noted that these levels actually decreased over time in patients who continued to receive diuretic therapy. The possibility that diuretic therapy may have blunted the beneficial effects of a low saturated fat, low-cholesterol diet has also been considered in the MRFIT study, but the study design may have exaggerated any possible drug effects. The subset of the population that seemed to show a definite difference in cholesterol lowering was the group that showed the greatest difference in weight--the nonsmoking patients who were not on therapy at six years, many of whom presumably entered the trial with lipid abnormalities as their major risk factor. An analysis of a group of 33 men who were treated with hydrochlorothiazide and followed for 42 months is cited as demonstrating a long-term adverse effect on cholesterol levels.[45] It is important to note that only 22, 14 and seven subjects were evaluated at 24, 36 and 42 months, respectively, and that, for example, the final cholesterol levels varied considerably in this small group of subjects. Data of this type should not be used to draw conclusions about therapeutic options.
There is little evidence that diuretic-based therapy adversely affects serum lipids in clinical trials of three to six years duration, and other reasons for the trial results should be considered. Diuretics are not ideal agents for use in all hypertensive patients. However, favorable data regarding the reduction of overall cardiovascular mortality in the long-term clinical trials suggest that they should remain initial monotherapy for many hypertensive patients.
REFERENCES [1]Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. A cooperative study. JAMA 1977;237:255-61. [2]The 1980 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1980; 140:1280-5. [3]The 1984 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1984;144:1045-57. [4]The 1988 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1988;148:1023-38. [5]The Australian therapeutic trial in mild hypertension. Lancet 1980;1(8181): 1261-7. [6]Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA 1979; 242:2562-71. [7]Amery A, Birkenhager W, Brixko P, et al. Mortality and morbidity results from the European Working Party on High Blood Pressure in the Elderly trial. Lancet 1985;1(8442):1349-54. [8]Medical Research Council Working Party. MRC trial of treatment of mild hypertension: principal results. Br Med J [Clin Res] 1985;291(6488):97-104. [9]Helgeland A. Treatment of mild hypertension: a five year controlled drug trial. The Oslo study. Am J Med 1980;69:725-32. [10]Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA 1970;213:1143-52. [11]Smith WM. Treatment of mild hypertension: results of a ten-year intervention trial. Circ Res 1977;40(5 Suppl 1):198-105. [12]Robertson JI. Hypertension and coronary risk: possible adverse effects of antihypertensive drugs. Am Heart J 1987;114(4 Pt 2):1051-4. [13]Ames RP. The influence of non-beta-blocking drugs on the lipid profile: are diuretics out-classed as initial therapy for hypertension? Am Heart J 1987;114(4 Pt 2):998-1006. [14]Schoenfeld MR, Goldberger E. Hypercholesterolemia induced by thiazides: a pilot study. Curr Ther Res 1964;6(3):180-5. [15]Ames RP, Hill P. Increase in serum lipids during treatment of hypertension with chlorthalidone. Lancet 1976;1(7962):721-3. [16]Chrysant SG, Neller GK, Dillard B, et al. Effects of diuretics on lipid metabolism in patients with essential hypertension. Angiology 1976;27:707-11. [17]Ames RP, Hill P. Raised serum lipid concentrations during diuretic treatment of hypertension: a study of predictive indexes. Clin Sci Mol Med 1978;55(Suppl 4):311s-4s. [18]Gluck Z, Baumgartner G, Weidmann P, et al. Increased ratio between serum beta- and alpha-lipoproteins during diuretic therapy: an adverse effect? Clin Sci Mol Med 1978;55(Suppl 4):325s-8s. [19]Crisp AJ, Kennedy PG, Hoffbrand BI, Ebbutt AF, Carruthers M. Lipids and lipoprotein fractions after cyclopenthiazide and oxprenolol: a double-blind crossover study. Curr Med Res Opin 1980;7(2):101-3. [20]Gluck Z, Weidmann P, Mordasini R, et al. Increased serum low-density lipoprotein cholesterol in men treated short-term with the diuretic chlorthalidone. Metabolism 1980;29:240-5. [21]Goldman AI, Steele BW, Schnaper HW, Fitz AE, Frohlich ED, Perry HM Jr. Serum lipoprotein levels during chlorthalidone therapy. A Veterans Administration-National Heart, Lung, and Blood Institute cooperative study on anti-hypertensive therapy: mild hypertension. JAMA 1980;244:1691-5. [22]Joos C, Kewitz H, Reinhold-Kourniati D. Effects of diuretics on plasma lipoproteins in healthy men. Eur J Clin Pharmacol 1980;17:251-7. [23]Bauer JH, Brooks CS, Weinstein I, et al. Effects of diuretic and propranolol on plasma lipoprotein lipids. Clin Pharmacol Ther 1981;30(1):35-43. [24]Grimm RH Jr, Leon AS, Hunninghake DB, Lenz K, Hannan P, Blackburn H. Effects of thiazide diuretics on plasma lipids and lipoproteins in mildly hypertensive patients. Ann Intern Med 1981;94:7-11. [25]Johnson BF. The emerging problem of plasma lipid changes during antihypertensive therapy. J Cardiovasc Pharmacol 1982;4(Suppl 2):S213-21. [26]Boehringer K, Weidmann P, Mordasini R, Schiffl H, Bachmann C, Riesen W. Menopause-dependent plasma lipoprotein alterations in diuretic-treated women. Ann Intern Med 1982;97:206-9. [27]Weidmann P, Gerber A, Mordasini R. Effects of antihypertensive therapy on serum lipoproteins. Hypertension 1983;5(5 Pt 2):III120-31. [28]Ames RP. The effects of antihypertensive drugs on serum lipids and lipoproteins. I. Diuretics. Drugs 1986;32:260-78. [29]Amery A, Birkenhager W, Bulpitt C, et al. Influence of anti-hypertensive therapy on serum cholesterol in elderly hypertensive patients. Results of trial by the European Working Party on High Blood Pressure in the Elderly (EWPHE). Acta Cardiol [Brux] 1982;37:235-44. [30]Veterans Administration Cooperative Study Group on Antihypertensive Agents. Comparison of propranolol and hydrochlorothiazide for the initial treatment of hypertension. II. Results of long-term therapy. JAMA 1982;248:2004-11. [31]Berglund G, Andersson O. Beta-blockers or diuretics in hypertension? A six year follow-up of blood pressure and metabolic side effects. Lancet 1981;1(8223):744-7. [32]Hulley SB, Furberg CD, Gurland B, et al. Systolic hypertension in the elderly program (SHEP): antihypertensive efficacy of chlorthalidone. Am J Cardiol 1985;56:913-20. [33]Heyden S, Borhani NO, Tyroler HA, et al. The relationship of weight change to changes in blood pressure, serum uric acid, cholesterol and glucose in the treatment of hypertension. J Chronic Dis 1985;38:281-8. [34]Helgeland A, Hjermann I, Leren P, Enger S, Holme I. High-density lipoprotein cholesterol and antihypertensive drugs: the Oslo study. Br Med J 1978;2(6134):403. [35]Lasser NL, Grandits G, Caggiula AW, et al. Effects of antihypertensive therapy on plasma lipids and lipoproteins in the Multiple Risk Factor Intervention Trial. Am J Med 1984;76(2A):52-66. [36]Multiple Risk Factor Intervention Trial Research Group. Risk factor changes and mortality results. JAMA 1982;248:1465-77. [37]Shekelle RB, Cagguilo AW, Grimm RH. Diuretic treatment of hypertension and changes in plasma lipids over 6 years in the Multiple Risk Factor Intervention Trial. Atherosclerosis 1984;12:113-27. [38]Greenberg G, Brennan PJ, Miall WE. Effects of diuretic and beta-blocker therapy in the Medical Research Council Trial. Am J Med 1984;76(2A):45-51. [39]Samuelsson O, Wilhelmsen L, Andersson OK, Pennert K, Berglund G. Cardiovascular morbidity in relation to change in blood pressure and serum cholesterol levels in treated hypertension. Results from the Primary Prevention Trial in Goteborg, Sweden. JAMA 1987;258:1768-76. [40]Wilhelmsen L, Berglund G, Elmfeldt D, et al. Beta-blockers versus diuretics in hypertensive men: main results from the HAPPHY trial. J Hypertens 1987;5:561-74. [41]The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart disease. JAMA 1984;251:351-64. [42]Amery A, Birkenhager W, Bulpitt C, et al. Diuretics--a risk in the long-term treatment of hypertensive patients? J Hypertens 1988;6:925-30. [43]Moser M. In defense of traditional antihypertensive therapy. Hypertension 1988;12:324-6. [44]Moser M. Implications of the clinical trials on the management of hypertension. Hypertension 1987;9(6 Pt 2):III80-5. [45]Middehe M, Weisweiler P, Schwandt P, Holzgreve H. Serum lipoproteins during antihypertensive therapy with beta blockers and diuretics. Clin Cardiol 1987;10(2):94-8. [Tabular Data 1 to 3 Omitted]
MARVIN MOSER, M.D. is clinical professor of medicine at Yale University School of Medicine, New Haven, Conn., and the senior medical consultant for the National High Blood Pressure Education Program. Dr. Moser is emeritus chief of the cardiology department at the White Plains (N.Y.) Hospital Center.
COPYRIGHT 1989 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group