ABSTRACT. Background: To restore intestinal integrity after starvation and trauma, luminal nutrients are essential. Specific nutrients such as glutamine support mucosal proliferation and energy metabolism. The aim of this study was to compare effects of enteral formula vs specific amino acids on ornithine decarboxylase (ODC) activity and adenine nucleotide metabolism in jejunal mucosa. Methods: Male Wistar rats (240 to 280 g) were starved for 48 hours and subjected to intestinal transection, gastrotomy, and jejunal instillation of 5-mL nutrient solution. In the first experiment, standard enteral formula (EF) was compared with isonitrogenous formula supplemented with the glutamine precursor, alpha-ketoglutarate (alpha-KG). In a second experiment, 2% glutamine was compared with isonitrogenous ornithine alpha-KG, arginine alpha-KG, glycine and diluted standard enteral formula (EF), or saline. The ODC activity, adenosine triphosphates (ATP), and
RNA and protein in the jejunal mucosa were analyzed 2 hours after surgery. Results: The ODC peak in jejunal mucosa in animals treated with EF was higher than when supplemented with alpha-KG (p
Regeneration of intestinal mucosa after starvation or trauma is initiated by an early peak of ornithine decarboxylase (ODC) activity.l2 ODC is the enzyme that starts the production of the polyamines putrescine, spermidine, and spermine. This enzyme is found in all eucaryotic cells and the levels of its polyamine products are highly regulated.3 They have an important role in the initiation of cell proliferation and in mitochondrial function. Increased ODC activity after trophic stimulation or during tissue regeneration has been observed in different types of tissues. This increase precedes the initiation of DNA and protein synthesis.
We have previously demonstrated that refeeding with enteral formula (EF) initiates a 30-fold increase of mucosal ODC activity 2 hours after surgery in rats starved for 48 hours. Specific components of the diet may play a crucial role in the stimulation of ODC activity. In in vitro studies, amino acids transported by sodium-dependent transport systems have been proposed to be of special importance to stimulate the ODC activity. Among the amino acids tested, glutamine (GLN), arginine, and ornithine have emerged as particularly potent to the maintenance of intestinal integrity.5-7 A number of studies suggest that GLN is conditionally essential for gut metabolism, structure, and function in the stressed animal.8-11
Glutamine is produced from both alpha-ketoglutarate (alpha-KG) and ornithine via glutamate, which is converted into GLN by the action of glutamine synthetase. The rapid metabolism of alpha-KG into glutamate and GLN has been highlighted in a study by Stoll et al,12 showing that alpha-KG enters the mitochondrial tricarboxylic acid (TCA)-cycle directly and therefore could act both as an energy source and a glutamine precursor. Due to a metabolic interaction between ornithine and alpha-KG in the splanchnic area, ornithine-ketoglutarate (OKG) is regarded as a very potent precursor of glutamine when given by the oral or enteral route.l314 Also, OKG is a precursor of arginine that plays an important role in intestinal function through the nitric oxide pathway.l5
Exposure of the gut to luminal nutrients stimulates ODC activity, and single amino acids have been shown to increase ODC activity.17 The aims of this study were to determine if rat intestinal ODC activity would be induced by a diet supplemented with alpha-KG or by single amino acid refeeding after surgery, and also to determine if there were any effects on the intestinal energy metabolism after supplying a-KG or specific amino acids by the enteral route in the early postoperative period.
MATERIALS AND METHODS
Study Design
Animals that had been starved for 48 hours were submitted to intestinal transection. At the end of the surgery, an infusion of enteral nutrients was administered by a jejunal catheter. In the first experiment, standard formula was compared with a formula supplemented with alpha-KG (n = 16). In the second experiment, separate amino acids-glycine (GLY), GLN, OKG, and arginine-ketoglutarate (AKG)-were compared with isonitrogenous whole-protein-based enteral formula (EF) and saline (SAL) (total n = 48). Rats that had been fed normally provided normal values (n = 5). Samples for analysis of ODC activity and phosphate-rich nucleotides were taken 2 hours after surgery in both experiments. ODC activity was related to protein content, and total RNA content was used to evaluate initiation of mucosal proliferation during this time period. Considering the circadian rhythm of ODC activity, the experiments in this study were confined to daytime before 12:00 PM.15
Animals and Experimental Model
Male Wistar rats (B 38 K Universal AB, Stockholm, Sweden), weighing 240 to 280 g were used. The rats were housed in pairs in a room maintained at 23degC, under a 12-hour day/night cycle throughout all the experiments and were fed a normal diet with no restriction on food or water supply for 2 weeks.
Before surgery, animals underwent food restriction with free access to water for 48 hours, and were weighed. Anesthesia with ketamine [Ketalar (80 mg/kg)] and xylazine [Rompun (8 mg/kg)] was given intraperitoneally. The abdomen was opened under sterile conditions by a full-length midline incision. The distal part of the ileum was transected and reanastomosed with interrupted stitches of resorbable suture (Vicryl). Gastrotomy in antrum was opened by a 2-mm incision to insert an infant-feeding catheter into the proximal jejunum for infusion of 5 mL of study substances. The abdomen was closed in layers. Postoperatively, 5 mL of physiologic saline was given subcutaneously. Normally fed rats without prior surgery were used as controls (n = 5).
Nutrients
Experiment I. The standard EF supplemented with alpha-KG group (0.79 g per 100 mL) was compared with isonitrogenous EF based on whole-protein composition. The formula (Naturell) was obtained from Semper AB, Sweden. The main components of 100 mL EF compared with a-KG: protein 4.9 g vs 4.9 g; carbohydrates 15.8 g vs 0.14.6 g; fat 4.3 vs 4.5 g. The energy content was 123 kcal per 100 mL vs 119 kcal per 100 mL in the alpha-KGsupplemented formula.
Experiment II. Two percent GLN was compared with isonitrogenous compositions of OKG, AKG, GLY, diluted (3:2) standard EF, and SAL.
One hundred milliliters of the different solutions contained: GLN, 2 g L-glutamine; OKG, 2.3 g L-ornithine + 1.0 g alpha-KG; AKG, 1.2 g L-arginine + 1.0 g alpha-KG; GLY, 2.1 g L-glycine. OKG, AKG, and Gln were provided by Gramineer AB in Sweden.
Sampling
The animals were anesthetized 2 hours postoperatively. The abdomen was opened, and 5 cm of proximal part of jejunum was stripped from mesentery and immediately frozen in the liquid nitrogen for adenosine triphosphate (ATP), adenosine diphosphate (ADP), and adenosine monophosphate (AMP) analysis. An additional 15 cm of the proximal part of jejunum was stripped from mesentery, cut, opened and rinsed in ice-cold phosphate-buffered saline (PBS). The mucosa was scraped from the smooth muscle layer with a microscope slide on ice, and weighed for the ODC, protein, and RNA analysis. Samples were put into liquid nitrogen and stored at -70degC. The animals were killed by heart cut.
ODC Activity in Proximal Jejunal Mucosa
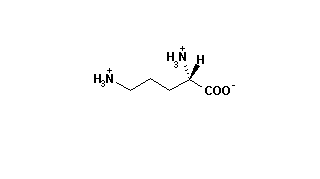
The ODC activity was measured enzymatically using ^sup 14^C-labeled ornithine as substrate and measuring the incorporation of 14C in C0^sub 2^, using a modified method that has previously been described.19 Briefly, mucosal scrapings were homogenized in 6-mL sodium phosphate buffer containing 100 U/mL penicillin-streptomycin, 0.25 M sucrose, and 10 uM DTT, using a Polytron homogenizer. A portion of this homogenate was saved at -20degC for analysis of protein and RNA. The remaining homogenate was centrifuged at 30,000 g at 4degC for 30 minutes, and the supernate was frozen at -70C pending ODC activity assay, which was done within 2 weeks. ODC activity was measured by incubating a 500 aliquote of the mucosa homogenate for 15 minutes at 37oC in the presence of 250 wL, 34 lM L-^sup 14^C-ornithine and 500 FL, 39 nM Tris-buffer containing 20 FM pyridoxal-phosphate, 1.4 mmol/L DTT, and 10 lM aminooxyacetic acid. The liberated ^sup 14^CO^sub 2^ from the decarboxylation of ornithine was trapped on a piece of filter paper with 20 lL 2 M NaOH, which was suspended in a center well above the reaction mixture. The reaction was stopped with 500 lL 6 M HCL and the samples were incubated again for 30 minutes. The filter papers were then taken out and put in 10-mL Hionic Fluor and measured in a liquid scintillation counter. Enzymatic activity was expressed a picomole ^sup 14^C0^sub 2^ per hour per milligram of protein.
^sup 14^C-labeled ornithine was purchased from Du Pont NEN Company, Boston, MA.
ATP, ADP, and AMP in Proximal Jejunal Mucosa
Samples were stored at - 70degC until they were freeze dried. Mucosa was dissected free of connective tissue under a microscope and grounded to a homogenous powder. ATP, ADP, and AMP were extracted from 2.5 mg of freeze-dried mucosa powder using 1 M perchloric acid containing 1 mmol/L EDTA. The extracts were neutralized with 2.2 M KHCO^sup 3^ and stored at -70degC until analysis. Analyses were performed with enzymatic fluorometry using methods modified from Harris et al.20 Energy charge (EC) was calculated according to the formula by Atkinson [EC=(ATP + 0.5ADP)/(AMP + ADP + ATP)].21 Total adenosine nucleotide levels were calculated as AMP + ADP + ATP. The contents of adenosine nucleotide were expressed a micromole per gram dry mucosa powder.
RNA and Protein in Proximal Jejunal Mucosa
RNA was determined by spectrophotometry using a modified Schmidt-Tannhauser method as described by Munro and Fleck.22 RNA results are expressed in milligram per gram wet weight mucosa. Protein was analyzed according to the method of Lowry.23
Statistics
Data are presented as means +/- SEM. Comparison between groups was done with the Mann-Whitney U test. Differences were considered significant at the p
Ethics
The study was approved by the Animal Ethics Committee of the Faculty of Health Sciences, Link*ping University.
RESULTS
ODC Activity
Experiment LI. When standard formula based on whole protein was supplemented with alpha-KG (a-KG group), the ODC activity 2 hours after surgery and refeeding in rats fasted for 48 hours was significantly lower than in the diet without alpha-KG (EF group; 50.23 10.26 pmol CO^sub 2^/h/mg protein vs 15.07 3.17 pmol in the alpha-KG group) (Fig. 1). There was an 8.4-fold increase in mucosal ODC activity in EF group compared with controls (6.02 0.62 pmol CO^sub 2^/h/mg protein).
Experiment II. The ODC activity increased in the EF group and was significantly higher than any other group (p
Energy Metabolism
Experiment I. There were no statistically significant differences in the measurements of adenine nucleotide contents and energy charge between the EF group and alpha-KG group (Table I).
Experiment II. The ATP content in the OKG group jejunal mucosa was numerically highest among the seven groups, but the differences between groups were not statistically significant. ADP contents in all six groups were below controls (4.94 0.45 [,mol/g dry mucosa), but there were no statistically significant differences. Interestingly, AMP contents were lower in both the EF and saline groups compared with controls (1.76 0.12 (mu)mol/g dry mucosa). In addition, EC was not significantly different between these groups nor compared with control value (0.66 0.07 pmol/g dry mucosa) (Table II).
RNA and Protein
No significant differences were seen in protein or RNA (range, 4.16 0.49 in GLY group to 4.55 + 0.26 mg/g wet weight in AKG group) contents in the jejunal mucosa among the groups.
DISCUSSION
Early enteral nutrition has been suggested to be of importance to maintain intestinal integrity after trauma and abdominal surgery. In the study presented, whole-protein-based EF was more effective in stimulating ODC activity than isonitrogenous administration of specific nutrients or the same formula supplemented with a-KG. Furthermore, nutrients did not have any significant effect on mucosal ATP content at this early time point, ie, 2 hours after surgery. The ODC results differ somewhat from previous reports on refeeding with amino acids.16,l7
The effects of fasting and refeeding on ODC activity of normal gastrointestinal mucosa have been studied extensively.24,25 Fasting reduces intestinal mucosal ODC activity to 20% of that found in fed animals.26 Refeeding by the oral route or by gavage have resulted in 15-fold to 40-fold increases in mucosal ODC activity after 2 to 4 hours.25 Minami et al17 reported that single amino acids mixed in a diet in intragastric feeding induce the ODC activity response in rats fasted for 12 hours. Compared with starvation, casein or an amino acid mix gave a 5-fold increase but single glycine or alanine mixed in a nonprotein diet resulted in a 10-fold increase. They found a dose-dependent increase in ODC by GLY that started at 100 mg, peaked at 200 mg but was stable up to 400 mg. They also examined the changes with time and found the first ODC activity peak at 2 hours and only a slight increase in ODC activity between 2 and 4 hours. The difference in results from the study presented here may be due to the starvation period, which was only 12 hours, the lack of trauma, a higher total amino acid dose (250 to 500 mg vs 100 mg), a higher amino acid dose related to body weight (2.5 to 5 g vs 0.5 g/kg body weight), longer time from feeding to sampling (4 hours vs 2 hours), or the combination of the single amino acids with a diet. Also, gastric feeding starts a hormone release from the stomach, and gastrin and cholecystokinin have been shown to enhance the activity of intestinal ODC.27 However, the lack of surgical trauma in the study by Minami et a17 makes comparisons less interesting.
The addition of surgical trauma in this context is crucial to develop an understanding of how to improve perioperative nutrition in relation to intestinal integrity. To our knowledge, we report the first attempt to elucidate the early ODC activity response to abdominal surgery and simultaneous refeeding in rats. In this model: (1) the gastrointestinal condition is similar to the malnourished patient undergoing abdominal surgery; (2) nutrients are infused directly into jejunum, admitting immediate jejunal mucosa exposure to the substrate of interest; and (3) no segmentation or exclusion of parts of the intestine is used, allowing a physiologic setting. This experimental model has been used in a previous study where we found that surgery combined with refeeding after 48 hours of starvation elicits a sharp 30-fold rise in ODC activity in jejunal mucosa, which is highest at 2 hours after surgery when the first 6 hours were studied.4 In the first experiment ct-KG was added to improve energy and glutamine availability. Contrary to this hypothesis, ODC activity decreased and ATP was numerically lower. To examine whether the ODC response was stimulated by amino acids as suggested by Minami,17 the second experiment was designed. Recently, Kandil et al showed that glutamine was one of the only nutrients to stimulate ODC activity in an in vitro study, where glutamine stimulated ODC activity in a dose- and time-dependent manner in porcine jejunal enterocyte line cells.28 We chose a 2% glutamine solution, which has been demonstrated to be effective in stimulating proliferation,29 and compared this to isonitrogenous amounts of the other specific nutrients and EF.
The only study we are aware of where single amino acids solution without diet has been used to study the induction of intestinal ODC response in rats after surgery was performed by Jain et al.16 ODC activity increased significantly, peaked after 2 hours, and declined after 4 hours after injection of GLY or L-asparagine into isolated intestinal segments in rats that had fasted for 48 hours. As in the study presented here, ODC activity was measured in the proximal 15 cm of small intestine. Fasting period, sampling time, and area were therefore the same in these two studies. Jain16 found a maximal response to glycine at 0.6 M. The difference in experimental design, ie, Jain et alls used closed segments of 5 cm for 2 hours and we gave the solution into the jejunum without any closed loops, is probably responsible for the difference in results. Due to this difference, doses given in relation to the mucosal area that was exposed are difficult to compare. However, Jain et all>; could activate ODC significantly by as little as 0.05 M glycine, corresponding to 0.025 mmol per 5-cm segment, which is comparable to our study in dose/cm. The fact that we could not reproduce their results could be due to the more expensive surgical trauma and anesthesia in our model or related to the time factor, ie, the time the mucosa was exposed in a closed segment vs the nonoccluded intestine. No residual solution was found in the intestinal segments sampled in our experiment.
The variability in ODC response in different experimental models could depend on dose of nutrient, time interval studied, differences in gastric emptying time, and intestinal motility with consequences for exposure time of the amino acid to the mucosa. Standard EF based on whole protein at a concentration used in human feeding strongly stimulates the induction of ODC activity in the study presented here. The diluted standard EF diet in the second experiment did also stimulate ODC activity but reached values that were only one third of the nondiluted. Therefore, the enteral diet concentration is a factor influencing the ODC activity. Future experimentation should evaluate the dose-response curve for putative effects of nutrients on ODC activity in this experimental setting. Not only amino acids but glucose and other compounds that are actively transported are equally interesting. It has been shown that 4-carbon amino acids were ineffective in stimulating ODC and it has also been demonstrated that the D-form of amino acids is effective, despite the fact that they cannot be metabolized.17
Why did the formula stimulate ODC more than the amino acids that have been demonstrated to be of particular importance to ODC? The fact that whole protein in the formula was compared with single amino acids probably does not explain the differences because it has been shown that an amino acid mixture is as effective as casein.17 Carbohydrates, fat, fibers, lectins, and retinoids could stimulate ODC.30 There is also a possibility that single amino acids in solution interact with other nutrient factors to stimulate the intestinal ODC response. However, the addition of glutamine to a diet with a normal glutamine content has not been shown to be beneficial to intestinal growth in any experiments using short bowel syndrome.cl Interestingly, we found that when standard EF based on whole protein was supplemented with the glutamine-precursor, a-KG, the ODC activity was significantly lower than in standard EF, although the two groups were isonitrogenous and very close to being isocaloric ( 123 vs 119 kcal/100 mL). There are reports that polyamines regulate mitochondrial function.as The lack of expected positive effects on ATP content in the mucosa when supplementing with alpha-KG in this experiment could be linked to the decrease in ODC activity but the mechanisms responsible for this decrease in ODC activity are obscure. The reduction by 7% in carbohydrate content to compensate for the extra alpha-KG (15.8 g vs 14.6 g per 100 mL) could also be of importance.
Adenine nucleotide levels are thought to represent a sensitive viability indicator of the intestine, and ATP depletion has been reported to affect tight junctions and paracellular permeability.33 We have found a constant decrease in ATP content during a 6 hour period after surgery that was not affected by administration of EF.4 However, this decrease was not significant after 2 hours. In the study presented here, there were no significant differences in ATP contents in jejunal mucosa among the six groups and no decrease by the long starvation period, demonstrating a stability of ATP content in the enterocytes. These results demonstrate the ability of the intestine to switch to vascular supply of nutrients in the absence of luminal nutrients. Early enteral nutrition did not seem to affect the ATP content of intestinal mucosa during the first 2 hours after surgery, an effect that could be due to energydemanding uptake of nutrients or trauma-induced cytokine release affecting the energy status.
Immediate postoperative enteral feeding by wholeprotein-based EF resulted in a increase of ODC activity 2 hours after surgery. This response was not found when using single amino acids in solution. Supplementing the EF with a-KG reduced the stimulation of the intestinal ODC activity. In order to optimize enteral nutrition it is of interest to elucidate the impact of different nutrient components on ODC activity and on gut integrity.
ACKNOWLEDGMENTS
The technical expertise of Ylva Braf Wiktorsson is gratefully acknowledged.
Hua Yang is a postdoctoral fellow from Department of Surgery, Xinqiao Hospital, Chongqing 630037, Peoples Republic of China.
This study was supported in part by the Medical Research Council (10402), and grants from County Council of Ostergotland, and Semper AB.
REFERENCES
1. Luk GD, Yang P: Distribution of polyamines and their biosynthetic enzymes in intestinal adaptation. Am J Physiol 254: G194-200, 1988
2. Fujimoto K, Neil Granger D, Tso P, et al: Ornithine decarboxylase is involved in repair of small intestine after ischemia-reperfusion in rats. Am J Physiol 261:G523-529, 1991 3. Tabor CW, Tabor H: Polyamine. Ann Rev Biochem 53:749-790, 1984
4. Yang H, Wiren M, Larsson J, et al: Early response of ornithine decarboxylase activity and energy metabolism to postsurgery refeeding in rat small intestine. Clin Nutr 18:41-45, 1999 5. Barber AE, Jones WG, Minei JP, et al: Glutamine or fiber supplementation of a defined formula diet: Impact on bacterial translocation, tissue composition, and response to endotoxin. JPEN 14:335-343, 1990
6. Cynober L: Can arginine and ornithine support gut functions?
Gut 15:29-33, 1994
7. Kalfarentzos F, Spiliotis J, Melachrinow M: Oral ornithine a-ketoglutarate accelerates healing of the small intestine and reduces bacterial translocation after abdominal radiation. Clin Nutr 15:29-33, 1996
8. Souba WW: Intestinal glutamine metabolism and nutrition. J
Nutr Biochem 4:2-9, 1993
9. Souba WW, Strebel FR, Bull JM, et al: Interorgan glutamine metabolism in the tumor-bearing rat. J Surg Res 44:720-726, 1988
10. Windmueller HG, Spaeth AE: Uptake and metabolism of plasma glutamine by the small intestine. J Biol Chem 249:5070-5079, 1974
11. Windmueller HG, Spaeth AE: Identification of ketone bodies and glutamine as the major respiratory fuel in vivo for post absorptive rat small intestine. J Biol Chem 253:69-76, 1978
12. Stoll B, Haussinger D: Functional hepatocyte heterogeneity: Vascular 2-oxoglutarate is almost exclusively taken up by perivenous, glutamine synthetase-containing hepatocytes. Eur J Biochem 181:709, 1989
13. Cynober L: Metabolic interaction between ornithine and a-ketoglutarate as a basis for the action of ornithine a-ketoglutarate. Clin Nutr 12:54-56, 1993
14. Payne-James J, Grimble G, Cahill E: Enteral administration of ornithine-oxoglutarate (OKG) in man: Effects on hormone profiles and nitrogen (N) metabolism. JPEN 13:36, 1989 15. Cynober L: Ornithine alpha-ketoglutarate. IN Amino Acid Metabolism and Therapy In Health And Nutritional Disease, Cynober L (ed). CRC Press, Boca Raton, 1995, pp 385-395 16. Jain R, Eikenburg BE, Johnson LR: Stimulation of ornithine decarboxylase activity in digestive tract mucosa. Am J Physiol 253:G303-307, 1987
17. Minami H, Miyamoto Y, Fujii Y: Induction of intestinal ornithine decarboxylase by single amino acid feeding. J Biochem 98:133139, 1985
18. Fujimoto K, Granger N, Johnson LR, et al: Circadian rhythm of ornithine decarboxylase activity in small intestine of fasted rats. Proc Soc Exp Biol Med 200:409-413,1992 19. Luk GD, Baylin SB: Polyamines and intestinal growth-increased polyamine biosynthesis after jejunectomy. Am J Physiol 245: G656-660, 1983
20. Harris RC, Hultman E, Nordesjo LO: Glycogen, glycolytic intermediates and high-energy phosphates determines in biopsy samples of musculus quadriceps femoris of man at rest. Methods and variance of values. Scand J Clin Lab Invest 33:109-120, 1974 21. Atkinson DE: The energy charge of the adenylate pool as a regulatory parameter, interaction with feedback modifiers. Biochemistry 7:4030-4034, 1968
22. Munnro HN, Fleck A: Analysis of tissues and body fluids for nitrigenous constiuents; IN Mammalian Protein Metabolism,
Munro HN (ed). New York, Academic Press, 1969, pp 465483
23. Lowry OH, Rosebrough NJ, Farr AL: Protein measurement with the folin phenol reagent. J Biol Chem 193:265-275, 1951 24. Maudsley DV, Leif J, Kobayashi Y: Ornithine decarboxylase in rat small intestine: stimulation with food or insulin. Am J Physiol 231:1557-1561, 1976
25. Tabata K, Johnson LR: Mechanism of induction of mucosal orni
thine devarboxylase by food. Am J Physiol 251:G370-374, 1986 26. Tabata K, Johnson LR: Ornithine decarboxylase and mucosal growth in response to feeding. Am J Physiol 251:G270-274, 1986 27. Fujimoto M, Kanaya A, Nakabou Y, et al: Circadian rhythm in the ornithine decarboxylase activity of rat small intestine. J Biochem 83:237-242, 1978
28. Kandil HM, Argenzio RA, Chen W: L-glutamine and L-asparagin stimulates ODC activity and proliferation in a porcine jejunal enterocyte line. Am J Physiol 269:G591-G599, 1995 29. Wiren M, Skullman S, Larsson J, et al: Intraluminal glutamine refeeding supports mucosal growth in rat jejunum. Transplant Proc 26:1460-1463, 1994
30. Otani S, Matsui-Yuasa I, Mimura Y, et al: Potentiation by retinoic acid of ornithine decarboxylase induction by phytohemagglutinin or phorbol 12-myristate 13-acetate in guinea pig lymphocytes. J Biochem (Tokyo) 99:1789-1797, 1986 31. Vanderhoof JA, Blackwood DJ, Mohammadpour H, et al: Effects of oral supplementation of glutamine on small intestinal mucosa mass following resection. J Am Coll Nutr 11:223-227,1992 32. Madsen KL, Brockway PD, Johnson LR, et al: Role of ornithine decarboxylase in enterocyte mitochondrial function and integrity. Am J Physiol 33:G789-797, 1996
33. Mandel LJ, Bacallao R, Zampighi G: Uncoupling of the molecular 'fence' and paracellular 'gate' functions in epithelial tight junctions. Nature 361:552-555, 1993
Hua Yang, MD ; Mikael Wiren, MD, PhD ; Jorgen Larsson, MD, PhD^; and Johan Permert, MD, PhD^
From the Department of Surgery and Clinical Research Center, Faculty of Health Science, Linkoping University, Sweden, and ?Department of Surgery, Karolinska Institute at Huddinge University Hospital, Stockholm, Sweden
Received for publication, February 11,1999.
Accepted for publication, March 12, 1999.
Correspondence: Mikael Wiren, MD, PhD, Department of Surgery, University Hospital, S-58185 Linkoping, Sweden.
Copyright American Society for Parenteral and Enteral Nutrition Jul/Aug 1999
Provided by ProQuest Information and Learning Company. All rights Reserved