Summary
In a double-blind trial, 194 ambulatory elderly patients (mean age, 74 [+ or -] 8 years) recovering from acute illnesses were randomly assigned to receive either ornithine oxoglutarate (OGO) or a placebo. Nine subjects withdrew during the study, six in the OGO group and three in the placebo group.
OGO and the placebo were administered once daily at a dose of 10 g after lunch for 2 months; the patients were monitored for a total of 4 months. Efficacy was evaluated in terms of nutritional variables, quality of life and total cost of medical treatment.
The analysis involved a total of 185 patients (93 in the placebo group and 92 in the OGO group). The two groups were comparable at inclusion. After 30 and 60 days of treatment, there was a significant improvement in the following variables in the OGO group relative to the placebo group: appetite (p<0.001), body weight (p<0.001) and independence (p<0.01). Two months after the end of treatment, there was still a significant improvement in the quality-of-life index (p<0.001) and the medical-cost index (p<0.03) in the OGO group, with an overall cost saving of 37%. We conclude that OGO seems to be a cost-effective nutritional supplement for elderly convalescent patients.
Introduction
Malnutrition affects between 40 and 70% of elderly patients in hospitals and institutional care, and 5-10% of free-living subjects over the age of 70 years(1)(2). The medical consequences (anaemia, recurrent infections, falls, loss of independence, bed sores and excess mortality) and socio-economic impact (increased length of hospital stay, increased care requirements) of malnutrition in elderly people have been widely studied, but there have been few reports on the potentially beneficial effects of preventive measures.
We therefore evaluated the medical and economic benefits of ornithine oxoglutarate (OGO) in independently living patients recovering from acute illnesses.
Patients and Methods
This randomized, double-blind, two-centre trial (Nice and Toulouse, France) involved convalescent, ambulatory, elderly subjects. The two geriatric units co-ordinated a group of 22 independent general practitioners. The patients were required to give their informed verbal consent before inclusion.
Inclusion and non-inclusion criteria: Patients eligible for inclusion were independently living subjects over 65 years of age, who were eating without assistance and who were recovering from respiratory, infectious or malignant diseases, or surgery.
Patients not eligible for inclusion were: subjects who refused to give their informed consent, and those who could not be followed-up for the whole 4-month study period; hospital patients and subjects aged less than 65 years; patients with serious diseases and/or a life expectancy of less than one year; patients with cancers requiring radiation therapy, chemotherapy or surgery within 4 months; patients taking medication likely to interfere with the evaluation of efficacy (anabolic drugs, appetite stimulants, vitamins, hormones, corticosteroids and dietary supplements).
Treatment: OGO and the placebo were taken at the end of the midday meal. They were presented in the form of two 5-g sachets to be dispersed in 200 ml of flavoured solution, or with yoghurt, a milk-based dessert or stewed fruit. The placebo was indistinguishable from OGO: the placebo was a maltodextrine with the same engergy content as OGO. Each 10 g of OGO contained 1.30 g of nitrogen.
The blinding was only lifted at the end of the study, and all the evaluation criteria were assessed blindly. The treatments were given for 2 months and the patients were then followed for another 2 months.
Evaluation criteria: The main judgement criteria were asthenia, appetite, bodyweight, muscle cricumference, quality of life and medical costs. Asthenia and appetite were evaluated subjectively using a validated 100-point visual rating scale. (Comparisons between scores given by the various practitioners could not be made because each treated only 10 patients.) Nutritional status was estimated on the basis of variables that were simple to measure in community practices. Changes in body weight were monitored over a 2-month period. Brachial circumference was measured in the upper third of the non-dominant arm. Serum albumin concentration was measured immediately before and after treatment (days 0 and 60); each practitioner was free to choose the laboratory that carried out the assay. Nutritional status was judged subjectively by the patient's practitioner, as poor (score 0), average (1) or good (2).
Costs of treatment were based on the Caisse Nationale d'Assurance Maladie statistics (1989, no. 47) for the following pragmatically chosen items: number of medical visits (to the practitioner or by the practitioner) + number of prescriptions + number of drugs + number of days spent in hospital, nursing care and physiotherapy.
None of the cost items was excluded with hindsight. The medical cost index was evaluated on days 0, 30, 60 and 120 (2 months after the end of treatment).
The quality of life index was defined as the sum of the following: asthenia + unaided dressing + visits to the shops, etc. + outside activities + number of consecutive days spent without leaving home + number of days with a body temperature of 38.5[degrees]C or less; it assessed on days 0, 30 and 60.
Statistical analysis: The required number of subjects was estimated on the basis of previous double-blind, randomized trials. Treatment was allocated using a computer program (Random), which stratified and balanced the randomization per practitioner. It was intended that 24 practitioners would each recruit ten patients.
The following covariables were taken into account when comparing the two groups at inclusion and for the efficacy analysis: age, sex, nature of the acute illness, initial body weight and weight loss during the month preceding inclusion.
Differences were sought using Student's t test and the Mann-Whitney nonparametric U test when the distribution was non-gaussian.
Before combining the data from the two centres, results were checked for comparability. Analysis following adjustment for the centre effect did not affect the outcome.
All the practitioners participating in the trial were informed of the methodology by the co-ordinator in each centre and by the statistician.
Results
One hundred and ninety-four patients recruited by 22 general practitioners were randomly assigned to receive either OGO or the placebo. Twenty-six patients withdrew from the study. Nine patients were excluded during the study: six in the OGO group, five because of diarrhoea and one because of pruritus; three in the placebo group, two because of diarrhoea and one because of nausea. The statistical analysis therefore concerned 185 patients, 93 in the placebo group and 92 in the OGO group. The mean age was 74 [+ or -] 8 years. There were no significant differences between the two groups at inclusion (Tables I and II).
Table I. Comparison of the two groups at inclusion
Nutritional status (0 = good, 2 = bad) 0.5 [+ or -] 0.6 0.6 [+ or -] 0.5
Appetite (0-100)
[TABULAR DATA OMITTED]
Nutritional status and appetite: Between day 0 and day 30, there was a significant improvement in several variables in the OGO group relative to the change in the placebo group: appetite for meat (p < 0.001), overall appetite score (visual rating scale: 44 [+ or -] 18 versus 38 [+ or -] 21, p < 0.001), and weight gain (1230 [+ or -] 1600 g versus 493 [+ or -] 1119 g, p < 0.001). Changes in the serum albumin concentration could not be analysed because too many data were lacking.
There were similar improvements in the OGO group at day 60, as follows: nutritional status (1.7 [+ or -] 0.5 versus 1.2 [+ or -] 0.7, p < 0.001), appetite (62 [+ or -] 19 versus 47 [+ or -] 23, p < 0.001), appetite for meat (p < 0.001), and weight gain (2172 [+ or -] 1912 g versus 925 [+ or -] 1652 g, p < 0.01). There was no significant improvement in brachial circumference (25 [+ or -] 4 cm versus 24 [+ or -] 5 cm, p = 0.07).
Medical-cost and quality-of-life indexes: The quality-of-life index (Figure 1) showed a significantly stronger improvement at day 60 in the OGO group (51.2 [+ or -] 28.8) than in the placebo group (32.5 [+ or -] 37.9) (p < 0.001). There was no significant difference between the improvements in the two groups at day 30. The individual items that accounted for the improvement were asthenia (p < 0.001), and indices of independence, such as dressing unaided (p < 0.01), visits to the shops, etc. (p < 0.01) and outside activities (p < 0.05).
[CHART OMITTED]
The medical-cost index showed no difference between days 0 and 60, but was significantly lower at day 120 in the OGO group than in the placebo group (Figure 2). In terms of actual cost, medical care represented 2586 French francs ([pound]290) per patient in the OGO group and 4089 FF ([pound]455) in the placebo group (p < 0.05), giving an overall cost saving of 37%. This reduction was essentially due to three factors: home visits by nurses (p < 0.01), home visits by doctors (p < 0.05), and the mean cost of prescriptions (p < 0.05).
[CHART OMITTED]
Discussion
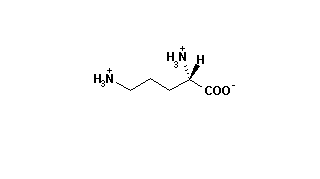
Ornithine oxoglutarate was originally used to treat cirrhotic patients, with the aim of reducing blood ammonia levels, as hyperammonaemia was thought to be the main cause of hepatic encephalopathy(3). It was during such treatment that Tremolieres et al.(4) first noticed that OGO improved nutritional status. This observation led to numerous studies aimed at determining the efficacy of ornithine salts in nutrition, particularly for elderly patients suffering from protein-energy malnutrition.
The risk of nutritional decompensation in the independently living elderly subject with intercurrent illnesses is less well known to physicians than the risk of dehydration. However, the anorexia that is always associated with a reduced awareness of thirst decompensates the precarious nutritional equilibrium, leading to asthenia, increasing the time spent immobile and thereby prolonging the convalescence period. This latter effect increases the risk of complications such as bedsores, thromboembolism, infections, loss of independence, and the need for medical and paramedical care. Unfortunately, artificial nutrition is expensive, poorly accepted by elderly patients and difficult to administer in the community.
We therefore tested a simple and rational approach to this problem, by administering OGO, which improves appetite and reduces the risk of complications in the hospital environment(5)(6)(7)(8)(9). This trial had two original features: (a) it was a two-centre study conducted by gerontologists and community practitioners in conditions of day-to-day medical practice and involving convalescent elderly patients; (b) we analysed the economic impact of this strategy.
OGO was effective in preventing secondary malnutrition following intercurrent illnesses in this population of independently living elderly subjects. The effect was seen rapidly, appearing within 1 month and reaching a high degree of statistical significance after 60 days of treatment. The improvements concerned not only subjective indices (appetite and nutritional status), but also objective nutritional markers such as weight gain. The improvement in brachial circumference, which did not reach the threshold of statistical significance (p = 0.07), is known to change slowly in elderly people. The OGO effects are not dependent on the nitrogen administered. In this study, the food intake was unknown but the quantity of nitrogen may be the important factor in the effect on appetite.
The positive effect of OGO on nutritional status was accompanied by an improvement in the conditions and quality of life. All the indicators of independence (dressing unaided, visits to the shops, etc. and participation in outside activities) showed highly significant improvements at day 60, and continued to do so over the 2 months following treatment. There was a highly significant difference in favour of OGO in terms of the 'number of days without leaving home' (p < 0.001).
The shorter convalescence period was also responsible for the reduction in the cost of medical care. The main element was a reduction in nursing care, which reflects the patients' independence. There were also significant differences in drug consumption and the number of visits by the practitioners to the patients' homes. This confirms the improvement in the conditions of convalescence among the OGO-treated patients relative to those receiving the placebo.
We used a daily OGO dosage of 10 g, which has been shown to have beneficial effects on both biological(10), and clinical indices in elderly malnourished hospital patients(11).
The mode of action of OGO has been extensively studied. It involves the individual metabolic effects of oxoglutarate and ornithine, and the fact that the two constituents follow a common metabolic pathway. It has been proposed that OGO acts by stimulating hormone secretion (insulin and growth factor), and by promoting anabolism by endogenous synthesis of key molecules in protein formation in the liver and fibroblasts(12)(13). Recently, Wernerman et al.(14) found that OGO supplementation in post-surgery parenteral nutrition improved the nitrogen balance, had a partial preventive effect on free-glutamine depletion in muscle tissue, and maintained polyribosome aggregation.
With regard to health costs and the quality of life, Cynober(15) retrospectively studied 136 burn patients treated with OGO and found a tendency towards a shorter hospital stay (36.6 [+ or -] 46.6 versus 51.8 [+ or -] 60.2 days in the control group), as well as a large but nonsignificant reduction in fatality (27.1% versus 39%; p = 0.09).
There was also a 37% reduction in the cost of medical care relative to the patients treated with the placebo in our trial. The maximum benefit was noted during the 2 months that followed the 2-month treatment period, suggesting a long-term effect of OGO. These results also showed that medical care requirements fell in both groups, confirming that the overall population was indeed 'convalescent'. The largest part of the medical care costs was situated in the pre-inclusion period and was due to hospital admission. During treatment and the subsequent 2-month follow-up period, the cost reduction was accounted for by a reduced need for nursing care at home, visits by the practitioner to the patient's home and the mean cost of prescriptions. The most marked saving concerned nursing care, and may have been due to improved healing of bedsores, reduced infectious complications and greater independence.
One important point in this study was the fact that the benefit of OGO only became apparent after the end of the treatment period. In addition, our results show the importance of acting preventively on nutritional status during convalescence.
Acknowledgements
We thank the Laboratoires LOGEAIS and all the practitioners for their support.
This paper was presented in part at the Second European Congress of Gerontology in Madrid in 1991.
References
(1.)Brocker P, Brignole-Baudouin F, Lods JC. Evaluation nutritionnelle du sujet age: interet du dosage de la T3 totale. Semin Hop Paris 1988;64:1943-52.
(2.)Vellas B, Albarede JL. Nutrition et vieillissement. Paris: Ed. Maloine, 1988.
(3.)Paris J, Merveille P, Molimard R. L'alphacetoglutarate d'ornithine dans les encephalopathies hepatiques. Nouv Presse Med 1970;1:1367-8.
(4.)Tremolieres J, Scheggia E, Flament CI. Effets de l'alphacetoglutarate sur le bilan azote et sur la vitesse d'oxydation de l'ethanol. Cah Nutr Diet 1972;7:2-7.
(5.)Le Petitcorps AM, Bernard PF. Alphacetoglutarate d'ornithine en nutrition enterale exclusive. Med Chir Dig 1985;14:441-5.
(6.)Cynober L, Lioret N, Coudray-Lucas C, et al. Action of alphaketoglutarate on protein metabolism in burn patients. Nutrition 1987;3:187-91.
(7.)Vesterberg K, Vinnards E, Leander U, Furst P. Nitrogen sparing effects of Ornicetil in the immediate postoperative state: plasma and muscle amino-acids. Clin Nutr 1987; 6:213-19.
(8.)Nicolas F, Rodineau P. Essai controle de l'alphacetoglutarate d'ornithine en alimentation enterale. Ouest Med 1982;35:711-13.
(9.)Demarcq JM, Delbas M, Trochu G, Crignon JJ. Effets de l'alphacetoglutarate d'ornithine sur l'etat nutritionnel des malades de reanimation. Cah Anesthesiol 1984;32:36.
(10.)Cynober L, Vaubourdolle M, Dore A, Giboudeau J. Kinetics and metabolic effects of orally administered ornithine alphaketoglutarate in healthy subjects fed with a standardized regimen. Am [pound] Clin Nutr 1984;39:514-19.
(11.)Brocker P, Sassard F, Lods JC. Influence de l'alphacetoglutarate d'ornithine sur l'albuminemie et la transferrinemie des sujets ages denutris. Rev Geriatrie 1985;10:233-6.
(12.)Lescoat G, Theze N, Fraslin JM, Pasdeloup N, Kneip B, Guegen-Guillouzo C. Influence of ornithin on albumin synthesis by fetal and neonatal hepatocytes maintained in culture. Cell Differ 1987;21:21-9.
(13.)Vaubourdolle M, Salvucci M, Coudray-Lucas C, Agneray J, Cynober L, Ekindjian OG. Action of ornithine alphaketoglutarate on DNA synthesis by human fibroblasts. In Vitro 1990;26:187-92.
(14.)Wernerman J, Hammarqvist F, Vinnars E. Alphaketoglutarate and postoperative muscle catabolism. Lancet 1990; 335:701-3.
(15.)Cynober L. Aminoacid metabolism in thermal burns. [pound]PEN 1989;13:196-205.
Authors' addresses
P. Brocker
CHU Nice, Hopital de Cantaron, 254 Chemin de la Lauvette, 0634 La Trinite, France
B. Vellas, J-L. Albarede
Centre de Medecine Geriatrique, CPU Purpan, Toulouse
T. Poynard
Service d'Hepato-Gastroenterologie, CHU Antoine Beclere, Clamart
Received in revised form 7 December 1993
COPYRIGHT 1994 Oxford University Press
COPYRIGHT 2004 Gale Group