Dear Dr. SerVaas,
My 20-year-old grandson developed epilepsy, having his first grand mal 3/23/01 when he was 17. Three years previous to that, there were times for a brief moment he did not communicate, but he never fell and was soon normal.
He is the sweetest, kindest, most generous young man you'd ever want to know.
The doctors said it is the worst case of epilepsy they have seen.
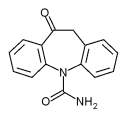
I have heard there are some trial tests of implanting something that would stop a seizure. Any information you could give me or any help where to turn would be deeply appreciated. The medicines he is on are: Depakote, 1 twice a day, and Keppra, 2 twice a day.
Thank you for listening and any help you can give.
Shirley Kirton
Tampa, Florida
You are probably referring to the vagus nerve stimulator (VNS)--a treatment option sometimes called a "pacemaker for the brain." The relatively new therapy utilizes a small generator implanted under the skin in the upper left chest and connected to electrodes coiled around the vagus nerve (cranial nerve 10) in the neck. When activated, the system delivers mild electrical impulses to the brain via the key nerve to block seizures in people with epilepsy.
VNS therapy was approved in 1997 for treating seizures that begin in one limited area of the brain. In clinical trials, about one third of people treated with VNS experienced a major improvement in seizure control, according to the Epilepsy Foundation. One third showed some improvement, while one third continued to have seizures as before.
Doctors now report that the therapy may also help some people with seizures resulting from a widespread electrical discharge involving both sides of the brain at once.
"Several centers, including our own, have implanted vagus nerve stimulators in patients with generalized epilepsy and reported that the results are similar to those obtained in patients with partial-onset seizures," explains Dr. Orrin Devinsky, director of the New York University Epilepsy Center, one of the country's largest epilepsy programs.
While the vagus nerve stimulator (VNS) can improve seizure control in many patients with difficult-to-control seizures, it is important to have realistic expectations, adds Dr. Devinsky, who is also a New York University School of Medicine professor of neurology, neurosurgery and psychiatry.
"It is very rare (less than 2 percent of cases, in my experience) that patients with seizures that are not controlled with medications come under full control after treatment with the vagus nerve stimulator," he says. "A very good result would be a 50 percent reduction in seizure frequency, which might be expected in 15 to 40 percent of cases. For someone who is having severe or frequent seizures, this would be a very meaningful improvement in their health.
"Other potential options include such medications as lamotrigine, zonisamide, topiramate, acetazolamide, oxcarbazepine, and carbamazepine. Finally, one can often improve seizure control through modifications in lifestyle: avoiding sleep deprivation, limiting or avoiding alcohol consumption, and reducing stress. For more information, epilepsy.com is an excellent source."
A final thought: If my grandson had seizures, I would make sure that he avoided foods and drinks containing the low-calorie sweetener aspartame. Although considered safe by the American Medical Association and the American Diabetes Association, there have been anecdotal reports linking aspartame to seizures and other neurological problems. Dr. Myron Roberts of West Palm Beach, Florida, is an advocate of avoiding aspartame in any form to prevent seizures in his patients with epilepsy.
COPYRIGHT 2005 Saturday Evening Post Society
COPYRIGHT 2005 Gale Group