BRECKENRIDGE, COLO. -- Antiepileptic drug usage by older women sharply increases their rate of bone mineral loss, with phenytoin being a particular offender, according to recent data from a landmark American study.
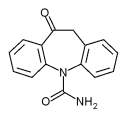
This is a disturbing finding in light of the fact that phenytoin remains the most frequently prescribed antiepileptic drug (AED) in this country, including among older patients, Jose F. Cavazos, M.D., said at a conference on epilepsy syndromes sponsored by the University of Texas at San Antonio.
"If you start a 70-year-old woman on phenytoin and her life expectancy is 15 years, you're going to considerably increase her likelihood of having a hip fracture, compared with women using other anticonvulsants," added Dr. Cavazos of the university's South Texas Comprehensive Epilepsy Center.
Dr. Cavazos noted that a fuller understanding of the scope of the fracture risk associated with specific AEDs was recently provided by an enormous population-based case-control study led by Peter Vestergaard, M.D., of Aarhus (Denmark) University. The investigators compared rates of AED use in 124,655 patients with any fracture and 373,962 controls.
In an unadjusted analysis, all AEDs--both traditional and newer ones--were associated with increased risk of fracture. However, after adjustment for history of corticosteroid use, prior fractures, diagnosis of epilepsy, comorbid conditions, and other potential confounders, the list of AEDs associated with a significantly increased fracture risk was narrowed to phenobarbital, with a 79% increased risk; clonazepam, 27%; carbamazepine, 18%; valproate, 15%; and oxcarbazepine, 14%.
While phenytoin and topiramate were associated with increased fracture rates of 20% and 39%, respectively, these didn't reach significance (Epilepsia 2004;45:1330-7).
The most encouraging finding in this impressive study, according to Dr. Cavazos, was that several newer AEDs emerged as being very unlikely to increase fracture risk. These included tiagabine, with an associated 25% reduced risk of any fracture, compared with non-AED users; vigabatrin, with a 7% decreased risk; and lamotrigine, with a nonsignificant 4% increased risk.
In discussing the overall osteoporosis risk in older women associated with AED use, Dr. Cavazos cited data from the Study of Osteoporotic Fractures (SOF), a National Institutes of Health-sponsored prospective study involving 9,704 elderly community-dwelling women.
In a recent secondary analysis of SOF data, Kristine E. Ensrud, M.D., of the University of Minnesota, Minneapolis, and her associates classified the women either as continuous users of AEDs during the study period, intermittent users, or nonusers. Serial measurements showed an adjusted average annual rate of decline in total hip bone mineral density of 0.70% in the nonusers, 0.87% in intermittent users, and 1.16% in continuous AED users.
The same highly significant pattern of increased bone loss with continuous use of AEDs was repeated at the calcaneus.
Extrapolating from the bone mineral density findings, Dr. Ensrud and her colleagues estimated that without intervention, continuous use of AEDs by women aged 65 years and older would increase their risk of hip fracture by 29% over 5 years (Neurology 2004;62:2051-7).
The SOF analysis also demonstrated that continuous use of phenytoin was associated with an adjusted 1.8-fold greater rate of bone loss at the calcaneus and a 1.7-fold greater bone loss at the hip, compared with non-AED users.
ARTICLES BY BRUCE JANCIN
Denver Bureau
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group