Relief of pain, whether post-traumatic or postoperative, is a prerequisite for the prevention of its deleterious effects on the whole organism. Unalleviated pain also increases the victim's or patient's anxiety and apprehension, which in turn increase the intensity of the pain. In the management of pain, opiates have maintained their position as the most common form of analgesic therapy despite the many side effects associated with their use. This double-blind study compared the analgesic effects of low doses of racemic ketamine and the morphine derivative oxycodone on postoperative pain after elective tonsillectomy. Also, the suitability of oxycodone for field use was evaluated with respect to ketamine. Plethysmographic pulse-- wave amplitude changes were compared with the pain visual analogue scale scores as measures of postoperative pain. The results of this study did not reveal any significant differences between the analgesic potencies of the studied drugs and clearly demonstrate that even suboptimal doses of both ketamine and oxycodone can provide appreciable relief of pain.
Introduction
Post-traumatic and postoperative pain are, depending on the type, localization, and extent of the injury or surgery, for the most part inevitable. If allowed to persist, pain in these instances is deleterious to the whole organism, even more so in the critical patient. Unalleviated pain is associated with increased anxiety and apprehension, which in turn increase the intensity of pain.
Parenteral administration of analgesic drugs, nonsteroidal anti-inflammatory agents, opioids, and especially ketamine in field medicine is an integral part in the post-traumatic or postoperative patients treatment. Parenteral administration is preferred to provide not only potent but also rapid pain relief.
In common practice, opioids are still the major agents of pain relief, but they are also accompanied by many side effects that limit their usefulness. Hence, methods to avoid their narcotic-- associated side effects are still being sought.1
The aims of this investigation were to compare the analgesic effects of low doses of racemic ketamine (Ketalar, Parke-Davis) and the morphine derivative oxycodone (Oxanest, Leiras, Turku, Finland], administered as intravenous bolus injections, and especially to evaluate the applicability of oxycodone for field use with respect to ketamine. A primary study of the plethysmographic pulse-wave amplitude as an objective measure of postoperative pain was also performed.
Postoperative pain after elective tonsillectomy was used as the model of pain.
Patients and Methods
Patients
Forty tonsillectomized male conscripts aged 21 to 28 years were randomized to receive either ketamine or oxycodone as the postoperative analgesic. Informed consent was obtained from all patients before their inclusion in the study.
Methods
Anesthesia
All patients received the same standard anesthesia. Induction was with thiopentone 4 to 5 mg IV in combination with alfentanil 1 mg IV and glycopyrronium bromide 0.2 mg IV. Rocuronium bromide 0.6 to 0.8 mg/kg was used for muscle relaxation and supplemented with 10- to 15-mg bolus doses, as indicated by the muscle Relaxograph (Datex Instrumentarium, Helsinki, Finland). After intubation, anesthesia was maintained with 5% desflurane in O^sub 2^/NO^sub 2^ (1:2).
One milliliter of a mixture containing glycopyrronium bromide 0.5 mg and neostigmine methylsulfate 2.5 mg was administered at the end of anesthesia for reversal of muscle relaxation.
The ventilatory volume (7-8 L/min) was adjusted to maintain 5% end-tidal CO^sub 2^. No premedication was used for any of the patients in either group. Glycopyrronium bromide and alfentanil were administered immediately before induction with thiopentone.
Patient Monitoring
The patients' electrocardiograms, blood pressure, pulse rate, oxygen saturation, respiratory rate, and muscle relaxation were monitored during anesthesia. Blood pressure, pulse rate, respiratory rate, and oxygen saturation were monitored in the recovery room.
Additionally, a pulse-wave oximeter (Satlitetrans, Datex Instrumentarium) with a finger probe was used to monitor changes occurring in the relative pulse-wave amplitude during the recovery room period. Pulse-wave amplitude, a relative measure, reflects the changes occurring in the vascular bed, i.e., its increase indicates vasodilation and its decrease indicates vasoconstriction, controlled by local autoregulation and systemic neural and humoral effects. The Satlitetrans oximeter is also provided with an additional feature that displays the pulse wave graphically simultaneously with numerical display of arterial oxygen saturation and pulse rate. Changes in pulse-wave trend were stored in memory as 10-second averages for later computer analyses with the Excel 5.0 program and as printouts for each individual patient.
Sedation, Anxiety, and Awareness
Visual analogue scales with a range from 0 to 10 were used to assess both sedation and anxiety: 0 denoted fully awake or relaxed and 10 denoted asleep or extremely anxious. Sedation and anxiety were assessed both before induction and in the recovery room at 0, 90, and 180 minutes.
Awareness was assessed in the recovery room at 0, 90, and 180 minutes on a scale from 0 to 4, with 0 denoting insensibility and 4 denoting full responsiveness. Sedation, anxiety, and awareness were evaluated by a single trained and experienced nurse for all patients.
Pain
Postoperative pain was assessed at 15-minute intervals on a 10-point visual analogue scale (VAS) with 0 denoting no pain and 10 denoting the worst pain imaginable. No attempts were made to differentiate between rest pain and pain induced by swallowing or coughing.
Changes in the averaged relative pulse-wave amplitude (as 10-second averages) trends were compared with the concomitant pain VAS scores (at 15-minute intervals).
Postoperative Analgesia
After having sufficiently recovered from anesthesia, the patients were transferred to the recovery room, where they received for postoperative pain a 0.2-mL bolus injection containing either 10 mg of ketamine or 2 mg of oxycodone in identical syringes coded and labeled with patient numbers to maintain a double-blind experimental design. The doses used were considered equally analgesic. The patients received the analgesic at their own request or according to the VAS score.
After the recovery room period, the patients were transferred to the ward, where they received ketoprofen 100 mg IV every 8 hours as the standard analgesic. At the patient's request, additional pain relief was provided by administering oxycodone 10 mg IM.
Statistics
At the end of the study, the codes were opened and the data were tabulated and subjected to statistical analyses (t test, regression). Analgesic efficacy was determined by comparing the pain intensity and the difference in pain intensity relief (initial pain intensity score minus subsequent VAS pain intensity scores).2 The differences in pain intensity relief were also calculated as percentages of the initial VAS score.
Results
No statistically significant differences were found between the two groups in the demographic data (Table I) or in the duration of anesthesia, recovery room time, or number of required analgesic doses (Table II). Neither were any statistically significant differences found between the groups in the hemodynamic baseline parameters or in preinduction sedation or anxiety.
Postoperative Analgesia
The mean initial recovery room pain VAS score was 6.0 in the ketamine group and 6.2 in the oxycodone group. The difference is not statistically significant.
A statistically significant difference was found in the pain intensity scores between the two groups in favor of ketamine at 165 and 180 minutes (p
Pain VAS Score and Plethysmographic
Pulse-Wave Amplitude
Regression analysis of the coincident mean pain VAS scores and the registered averaged relative pulse-wave amplitude changes showed an inverse correlation between the two parameters. An increase in the VAS score was reflected as a decrease and a decrease in the VAS score was reflected as an increase in the relative pulse-wave amplitude in both groups (ketamine group, r = -0.8637, p
Effects on Hemodynamics
Throughout the recovery room period, the mean systolic and diastolic blood pressures remained at higher levels in the ketamine group than in the oxycodone group (p
The mean systolic pressure in the ketamine group was 128.6 mm Hg at baseline (range, 101-163 mm Hg) and 135.7 mm Hg at 180 minutes (range, 109-183 mm Hg); in the oxycodone group, the values were 129.5 mm Hg at baseline (range, 118-- 145 mm Hg) and 126.5 mm Hg at 180 minutes (range, 105-155 mm Hg). In the ketamine group, the mean diastolic pressure was 65.8 mm Hg at baseline (range, 51-81 mm Hg) and 69.9 mm Hg at 180 minutes (range, 57-92 mm Hg); in the oxycodone group, the values were 68.0 mm Hg at baseline (range, 54-76 mm Hg) and 64.9 mm Hg at 180 minutes (range, 51-84 mm Hg).
The mean pulse rate was constantly higher in the ketamine group (range, 49-118 beats/min; mean at baseline, 63 beats/ min; mean at 180 minutes, 75 beats/min) than in the oxycodone group (range, 40-113 beats/min; mean at baseline, 60 beats/min; mean at 180 minutes, 65 beats/min) (Fig. 4). Nevertheless, the differences were not statistically significant.
Also, the pooled mean pulse pressure (systolic minus diastolic pressure) was constantly higher in the ketamine group (mean, 64.3 mm Hg; range, 61.4-68.7 mm Hg; baseline, 62.8 mm Hg; range, 50-87 mm Hg) than in the oxycodone group (mean, 60.5 mm Hg; range, 58.4-67.2 mm Hg; baseline, 61.4 mm Hg; range, 49-70 mm Hg). The difference was statistically significant (p
Effects on Respiration
Oxygen Saturation
During the recovery room period, the mean oxygen saturation was 97.46% (range, 94.0-99.0%) in the ketamine group and 96.72% (range, 92.0-99.0%) in the oxycodone group (Fig. 5). None of the patients in either group required supplementary oxygen.
Respiratory Rate
The mean respiratory rate was higher in the ketamine group than in the oxycodone group throughout the recovery room period. The respiratory rate varied between 14 +/- 2.3 and 16 +/-- 2.6 breaths/min (range, 10-22 breaths/min) in the ketamine group and between 13 +/- 1.8 and 15 +/- 3.3 breaths/min (range, 8-18 breaths/min) in the oxycodone group (Fig. 5).
Sedation, Anxiety, and Awareness
At the end of the recovery room period (180 minutes), the patients in the oxycodone group were more sedated than the patients in the ketamine group (Table III). The mean VAS scores were 6.8 vs. 5.1, respectively (p
Side Effects and Patient Acceptance
Nausea occurred in three patients (15%) in the ketamine group, although it was not associated with the drug, and in two patients (10%) in the oxycodone group. One severe case of vomiting, not associated with the analgesic used, and two cases of itching (10%), one mild and one severe, occurred in the oxycodone group. In the patients with nausea and vomiting not attributable to the drugs, the causes were swallowing of blood and postoperative pharyngeal irritation. Pruritus was reported by two patients in the oxycodone group.
Mild central nervous system side effects were registered in 12 patients (60%) in the ketamine group. Unreal dreams were experienced by 3 patients (15%), two mild and one severe, as were hallucinations (all moderate). Two patients had nightmares (one mild, one moderate), and 4 patients were slightly confused or agitated. Only 1 patient in the oxycodone group was slightly agitated.
Patient acceptance of the analgesic used was higher in the ketamine group than in the oxycodone group. Only one patient (5%) in the ketamine group and three patients (15%) in the oxycodone group were dissatisfied with the pain relief provided by the administered drug.
Discussion
Ketamine, which is chemically related to phencyclidine and cycloheximide, is widely accepted as the first-choice analgesic/ anesthetic in field and disaster medicine. It is also the drug of choice for providing analgesia in entrapments.3
Ketamine has many therapeutic indications and possesses amnestic, sedative, anesthetic, analgesic, and, paradoxically, anticonvulsant properties. It also has a stimulatory effect on circulation, and respiratory depression is extremely rare. Its stimulatory effects on circulation depend on endogenous catecholamine release, whereas in catecholamine-depleted patients it can exert negative inotropic effects. Narcotics commonly used for postoperative analgesia (e.g., oxycodone) may release histamine and cause bronchospasm in asthmatics. Ketamine provides the additional advantage of preventing and relieving bronchospasm.4 Furthermore, ketamine has satisfactory local anesthetic properties.5
In addition to conventional intravenous and intramuscular administration, ketamine can also be given rectally, orally, intranasally, epidurally, and intrathecally.
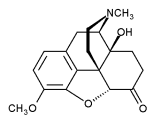
In Finland, oxycodone, an opioid derived from thebaine, one of the phenanthrene alkaloids of opium, is the most frequently used parenteral opioid for premeditation, sedation, and treatment of postoperative pain.6 It is suitable for oral, intramuscular, intravenous, subcutaneous, and rectal administration. It is somewhat more potent than morphine when administered intravenously in equal doses.
In contrast to morphine, oxycodone's antinociceptive effects have a rapid onset of maximum effect (approximately 5-7 minutes vs. 30-45 minutes for morphine) but are of a relatively short duration (approximately 90 minutes vs. approximately 180 minutes for morphine).7 New data also suggest that these effects are mediated by rc-opioid receptors, in contrast to morphine, which interacts primarily with (mu)-opioid receptors.8
Oxycodone liberates less histamine and causes hallucinations less frequently than morphine, but in other respects its side effects are similar to those of morphine.7 The half life of oxycodone is somewhat longer than that of morphine. Oxycodone is considered at least as toxic as other opioids, and its abuse potential is equivalent to that of morphine.7,9
Although the analgesic properties of both racemic ketamine and oxycodone have been studied separately, there are apparently no previous studies comparing these drugs with each other.
It has been shown that low-dose ketamine added to general anesthesia before surgical stimulation decreases postoperative pain, as indicated by the longer time after the end of surgery until the first request for an analgesic and the reduced dose requirements of analgesic.10 The use of low to anesthetic doses of ketamine as an analgesic during transportation of patients in pain has also been found feasible.11,12
The administration of weak opioids, mixed agonist/antagonist drugs, and/or partial agonists is not considered useful in the field of emergency medical rescue work. In the case of severe myocardial infarction pain, the use of a strong opioid (e.g., morphine, oxycodone) is recommended, and in the case of traumatic pain, fentanyl or ketamine is recommended.13
Monitoring of the plethysmographic pulse wave is a less frequently used method of patient surveillance.14,15 The pulse-wave amplitude, which is a relative measure, is an informative indicator of changes occurring in the vascular bed circulation and depicts the blood volume arriving with each heartbeat at the peripheral measuring point and changes in intravascular blood volume. Vasodilation increases the wave amplitude, whereas vasoconstriction decreases it. These alterations are regulated by the tone of the vascular musculature controlled by local autoregulation and by nervous and humoral hormonal effects. During anesthesia, especially when it is light, and during the recovery room period, several typical variations can be observed in the pulse-wave amplitude.15 Preinduction anxiety and fear cause relative vasoconstriction, resulting in a low amplitude that increases significantly as the patient becomes relaxed and loses consciousness. Both intubation and the skin incision are strong stimuli inducing instant vasoconstriction and an abrupt decrease in amplitude. During the postoperative period especially, pain is evident as a decrease in the pulse-wave amplitude.
In the present study, the patients' averaged relative pulse-- wave amplitude changes were compared with the corresponding concomitant pain VAS scores at 15-minute intervals. In both groups, regression analysis indicated a linear inverse correlation between the pulse-wave amplitude and the concomitant pain VAS score. The lesser sensitivity of the pulse-wave amplitude in the ketamine group could partly depend on ketamine's stabilizing effects on circulation and hemodynamics. These results warrant further, more detailed studies.
By releasing histamine, opioids can induce a decrease in the systemic blood pressure, but this can also be attributed to their alleviating effect on pain and decreased sympathetic output. In one patient in the oxycodone group, systolic blood pressure decreased 40 mm Hg, from 152 mm Hg at 0 minutes to 112 mm Hg at 15 minutes. The corresponding decrease in pulse pressure was also 40 mm Hg, from 69 mm Hg at 0 minutes to 29 mm Hg at 15 minutes. If this was caused by oxycodone, this one case demonstrates the potential risk of opioid-associated blood pressure decrease even with suboptimal doses.
Trauma patients frequently suffer from loss of blood and hemorrhagic shock. This should to be taken into consideration, especially in field conditions, because ketamine's stimulatory effects on the circulation have a preventive and/or ameliorating influence on the systemic effects of blood pressure decrease and thus counteract shock, whereas opioids have a pronounced decreasing effect on blood pressure.
Oxycodone has been found to cause significant respiratory depression, as reflected by increases in the inspiratory-expiratory oxygen difference and end-tidal CO^sub 2^ concentration and by decreases in both the minute volume of ventilation and respiratory rate, compared with both tramadol and placebo.16 Oxycodone (0.1 mg/kg) appears to cause greater ventilatory depression than comparable analgesic doses of other opioids.17 In the present study, the respiratory rate was statistically significantly lower in the oxycodone group than in the ketamine group (p
Sedation of the patients was more pronounced in the oxycodone group, and they were less anxious and less aware. Lesser sedation and higher anxiety and awareness scores in the ketamine group can be considered advantageous in ensuring maintenance of good patient cooperation.
The two cases of pruritus in the oxycodone group can be attributed to receptor effects, which are typical of morphine and structurally similar opioids.
The central nervous system side effects occurring in the ketamine group could be anticipated, because no preventive premedication (e.g., a benzodiazepine or droperidol) was administered before ketamine.
Notwithstanding the high incidence (60%) of central nervous system side effects in the ketamine group, patient acceptance was better than in the oxycodone group (95 vs. 85%). The only logical explanation for this inconsistency is the amnestic effect of ketamine. Moreover, all side effects were very mild and were reported only when questioned.
Conclusions
Notwithstanding the statistically significant differences between the two study groups, this investigation failed to reveal any practically significant differences between the analgesic potencies of ketamine and oxycodone. On the other hand, it definitely demonstrates that even suboptimal doses can provide appreciable relief of pain without causing undue confusion of the patient, which, in turn, would result in diminished or poor patient cooperation.
Compared with ketamine, oxycodone or any other opioid cannot be recommended as an analgesic for field use or for trauma patients when monitoring of vital patient parameters is in any respect deficient or has to be compromised.
Acknowledgments
Appreciation is extended to associate professor Matti A.K. Manila, MD PhD, for his guidance and interpretation of the plethysmographic pulse-- wave registrations, to research scientist Harry M. I,arni for his technical assistance, and to Juha-Pekka Vesanen, RN, for collecting the patient data. This investigation was approved by the Ethical Committee of the Medical Section of the Defense Staff, Finnish Defense Forces.
References
1. Wang CS, Cheng CH, Ho ST: Clinical applications of excitatory amino acid antagonists in pain management. Acta Anaesthesiol Sin 1995: 33: 227-32.
2. Lippmann M, Mok MS, Steen SN, Lane AZ, Caruso Torrance FS: Analgesic onset time of iv butorphanol in postsurgical patients. In Disaster Medicine: Resuscitation and Life Support, Relief of Pain and Suffering. Vol 2, pp 81-7. Edited by Frey R, Safar P. Berlin. Springer-Verlag, 1980.
3. Cottingham R, Thomson K: Use of ketamine in prolonged entrapment. J Accid Emerg Med 1994; 11: 189-91.
4. Jahangir SM, Islam F, Aziz L: Ketamine infusion for postoperative analgesia in asthmatics: a comparison with intermittent meperidine. Anesth Analg 1993; 76: 45-9.
5. arni HM, Saarelainen IO, Levanen J, Kiistala U, Pohjola J: Suction blistering applied to testing local analgo-anesthetic effect of ketamine. Ann Med Milit Fenn 1995; 70: 77-81.
6. Poyhia Ic Opioids in anaesthesia: a questionnaire survey in Finland. Eur J Anaesthesiol 1994; 11: 221-30.
7. Poyhia R, Vainio A, Kalso E: A review of oxycodone's clinical pharmacokinetics and pharmacodynamics. J Pain Symptom Manage 1993; 8: 63-7.
8. Ross FB, Smith MT: The intrinsic antinociceptive effects of oxycodone appear to be kappa-opioid receptor mediated. Pain 1997; 73: 151-7.
9. Drummer OH, Syrjanen ML, Phelan M, Cordner S: A study of deaths involving oxycodone. J Forensic Sci 1994; 39: 1069-75.
10. Roytblat L. Korotkoruchko A, Katz J, Glazer M. Greenberg L, Fisher A: Postoperative pain: the effect of low-dose ketamine in addition to general anesthetics. Anesth Analg 1993; 77: 1161-5.
11. Ansem RP, Hartman JA, Foudraine JF, van Loenen E, Rutten FL: Analgetic ketamine feasible in ambulance emergency care. Ned Tijdschr Geneeskd 1994; 138: 2301-4.
12. Notcutt WG: Transporting patients with overwhelming pain. Anaesthesia 1994; 49: 145-7.
13. Sittl R, Griessinger N, Risack D: Schmerztherapie im Rettungsdienst: Behandlungskonzepte fur Trauma- and Heczinfarktpatienten. [Management of pain in the medical rescue service: management concepts for trauma and myocardial infarction patients.] Notfallmedizin 1994; 20: 412-8.
14. Johnstone M: Digital vasodilatation: a sign of anaesthesia. Br J Anaesth 1985; 57: 524.
15. Manila MAK: Pulse wave oximetry and capnography in monitoring depth of anaesthesia. In Memory and Awareness in Anaesthesia. Edited by Bonke B, Fitch W, Millar K. Amsterdam/Lisse. Swewts & Zeitlinger, 1990.
16. Tarkkila P, Tuominen M, Lindgren L: Comparison of tramadol and oxycodone. J Clin Anesth 1997; 9: 582-5.
17. Olkkola KT, Hamunen K, Seppala T, Maunuksela EL: Pharmacokinetics and ventilatory effects of intravenous oxycodone in postoperative children. Br J Clin Pharmacol 1994; 38: 71-6.
Guarantor: Lt Col Jaakko Levanen, FDF
Contributor: Lt Col Jaakko Levanen, FDF
Department of Anesthesiology, Military Central Hospital, Mannerheimintie 164, 00300 Helsinki, Finland.
Presented in part at the 32nd International Congress on Military Medicine, April 19-24, 1998, Vienna, Austria.
This manuscript was received for review in July 1998. The revised manuscript was accepted for publication in January 1999.
Copyright Association of Military Surgeons of the United States Jun 2000
Provided by ProQuest Information and Learning Company. All rights Reserved