A persistent or recurring ache or pain that strikes between your navel and crotch can be more difficult to diagnose than most women would ever guess. While ovarian cancer may be the first thing to leap to your mind (and not entirely without reason; it ranks as the fourth-leading cause of cancer death among U.S. women), the more likely scenario is one of the more common, but still potentially dangerous, gyno woes that follow.
It can, however, be frustrating and difficult to pinpoint the specific source of gynecological pain, because so many organs--the uterus, the ovaries, the fallopian tubes, the bladder and the rectum--share a relatively compact space, notes Kathleen Fitzgerald, M.D., a clinical assistant professor of obstetrics and gynecology at Brown Medical School in Providence, R.I. "Separating them [as pain sources] isn't easy for patients or physicians."
If it's just a mild twinge, you might be tempted to shrug it off or pop an over-the-counter pain reliever. "Unfortunately, the level of pain does not necessarily correlate with the cause," Fitzgerald says. "Some people with a high pain threshold won't be doubled over." So if the discomfort becomes persistent, it's essential to learn how to name your pain, pinpoint the source and effectively communicate those details to your gynecologist.
Here's what you need to know about types of pain and what they might mean.
The pain: an intense ache in the lower pelvis
* If the pain is sharp or there's tenderness around the navel or on the right side of the abdomen, it could indicate appendicitis (in which case you'd probably have a slight fever too), but it may also be a sign of a ruptured ovarian cyst or ovarian torsion.
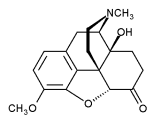
* Ovarian cysts, like cysts elsewhere, are closed sacs, usually filled with fluid or semisolid material. If the cyst ruptures, pain medication--a nonsteroidal anti-inflammatory drug (NSAID) for mild pain, codeine or oxycodone for more severe pain--may be necessary until the hurt subsides and the lesion heals, according to Gerson Weiss, M.D., a professor and the chair of the department of obstetrics, gynecology and women's health at the University of Medicine and Dentistry of New Jersey-New Jersey Medical School in Newark.
* Ovarian torsions (twisting) are most common when the fallopian tube on the side that's painful has been removed or when the cyst present is a dermoid cyst. These result when cells in the ovary develop into mature tissues and structures such as hair, bone and teeth. A twisted ovary may have its blood supply blocked. If that doesn't cause the ovary to die, it can be untwisted surgically to save the organ.
The pain: a sharp ache in the abdomen with vaginal bleeding
* When experienced along with weakness or dizziness, such symptoms can signal an ectopic pregnancy, a potentially life-threatening condition in which a fertilized egg grows in the fallopian tube instead of in the uterus. Such a pregnancy must be terminated either with medication, with laparoscopic surgery (the insertion of a telescopic probing device into the abdomen) or with an open laparotomy (full abdominal surgery), according to David Foster, M.D., an associate professor of obstetrics and gynecology at the University of Rochester School of Medicine and Dentistry in Rochester, N.Y.
The pain: sharp cramps seemingly unrelated to your period
* More than 50 percent of women suffer from pain during their periods, something doctors call dysmenorrhea. But only about 20 percent experience Mittelschmerz, German for "middle pain," which occurs 14-16 days before menstruation begins, when an egg is released by the ovary. Depending on how pain-sensitive a woman is, she may feel this as mild to moderately severe discomfort that lasts a few hours or a day before fading.
* Premenstrual cramps, on the other hand, which typically occur five to 11 days before menstruation, can be severe enough to interfere with daily routines and activities for 30-40 percent of women. A common symptom of premenstrual syndrome (PMS), which affects 70-90 percent of women, the cramping is brought on by the release of prostaglandins, fatty acids made by the body that act as messengers and can stimulate muscle contractions, including that of the uterus. An NSAID such as ibuprofen or naproxen can relieve this type of cramping; so can applying a hot-water bottle to the lower abdomen, Fitzgerald says.
* Noncyclical cramping experienced for at least six months in the pelvis, lower back or buttocks may be diagnosed as chronic pelvic pain. (See "What Is Chronic Pelvic Pain?" on page 117 for more information about this condition, which affects nearly one-quarter of women ages 18-49.)
The pain: A burning or "cutting" sensation during sex
Sex is supposed to be one of the most pleasurable activities on the planet, so when penetration and thrusting hurt, it can be both physically and emotionally traumatic. Nearly two out of three women will experience painful sex, known as dyspareunia, at some point, according to the American College of Obstetricians and Gynecologists. If sex is only occasionally painful, the cause may be nothing more than inadequate lubrication. If it's more frequent, other conditions may be to blame:
* If you feel a persistent burning sensation at the opening to the vagina, you may have an undiagnosed vaginal infection (such as trichomoniasis or bacterial vaginosis); your doctor will probably need to do a wet-mount smear (in which salt or an alkaline solution is added to a vaginal culture before it's examined under a microscope) to reveal the culprit. Medications will cure most of these infections.
* If the pain is stinging or feels like a knife stab in the vaginal opening during sex or even exercise, it could stem from vulvodynia, inflammation of the nerve endings in the vulva, one of the most common causes of painful intercourse among premenopausal women, says David Foster.
A recent survey by researchers at the University of Michigan Center for Vulvar Diseases in Ann Arbor found that 28 percent of women have experienced vulvar pain and 3 percent have been chronic sufferers. Vulvodynia's cause is unknown, and the inflammation occurs in the absence of infection or genital skin diseases. It's usually diagnosed during touch testing--pressing on different areas with a cotton swab and measuring response to pain. Various treatments include applying topical anesthetics to numb the labia, prescribing tricyclic antidepressants to increase tolerance to pain, and/or assigning physical therapy to relax the muscles around the vulva and reduce sensitivity.
* Pain deep inside the pelvis during sex could be an infection, an ovarian cyst, endometriosis (a condition in which pieces of the uterine lining attach to and grow in other areas of the pelvis), or other conditions such as fibroids (abnormal growths on or within the uterine wall) or scar tissue. These conditions are usually diagnosed through a pelvic examination, ultrasound and/or laparoscopy and can be treated with prescription medications such as GnRH agonists, oral contraceptives or anti-inflammatory drugs. Your doctor may recommend surgery to remove the tissue, depending on your age and whether you ever want to have children or want more children.
* Pelvic inflammatory disease (PID), an infection of the lining of the uterus, fallopian tubes and ovaries that often occurs as a result of an infection from a sexually transmitted disease like chlamydia or gonorrhea, typically causes intense pain in the lower pelvis (often during sex) and is usually accompanied by fever, chills, and a foul-smelling, thin, yellowish-to-grayish-white vaginal discharge. PID is usually treated with antibiotics.
The pain: stinging or burning during urination
* While not strictly speaking a gynecological problem, urinary tract infections (UTI) are responsible for a lot of below-the-belt misery. Characterized by a burning sensation during urination, a strong desire or need to use the bathroom frequently and, sometimes, blood in the urine, UTIs will afflict one in five women at some point in their lives, and an unfortunate 30-50 percent of those women will have more than one occurrence. A urine culture will confirm the presence of a UTI, and taking an antibiotic for a few days will clear up the infection.
RELATED ARTICLE: naming the pain
To work with your gynecologist in diagnosing the cause of your pain, you have to be able to clearly communicate what's happening to you. Physicians recommend keeping a pain journal for more than one cycle in which you note the following:
When the pain occurs in your menstrual cycle This allows your doctor to differentiate menstrual cramping from other, more serious conditions. You should also record the time of day and what you were doing at the time--whether the pain struck while you were eating, going to the bathroom, having sex, sleeping, exercising, etc.
A detailed description of the pain Note how long it lasts: Is it a sharp stab or a dull ache, a throbbing pain or a steady one? Identify the location and the intensity of the pain as precisely as you can.
Anything else you think may be important Are you running a fever? If the pain affects visible tissue, describe whether the tissue is red and/or swollen. Additionally, note the color and consistency of vaginal discharge and whether you've been experiencing bloating.
RELATED ARTICLE: what is chronic pelvic pain?
Researchers at the University of Oxford in the U.K. found that 24 percent of women between the ages of 18-49 have what's called chronic pelvic pain (CPP): recurrent or constant pelvic pain that lasts six months or longer and isn't related to their periods.
For many of these women, relief--not to mention an accurate diagnosis--can be maddeningly elusive. One reason: Conditions that cause CPP often don't show up as abnormalities on diagnostic tools like ultrasound or magnetic resonance imaging (MRI), says John F. Steege, M.D., director of the Pelvic Pain Clinic at the University of North Carolina at Chapel Hill and lead author and editor of Chronic Pelvic Pain: An Integrated Approach (W.B. Saunders, 1998).
Among the most common causes of CPP are endometriosis, pelvic adhesions (scar tissue that develops after infection or surgery), a chronic pelvic infection, pelvic-floor muscular disorders (affecting the bladder, uterus and rectum), interstitial cystitis (inflammation in the lining of the bladder as well as recurring discomfort, pressure, tenderness or intense pain in the bladder and surrounding pelvic region) and uterine fibroids.
Complicating matters, there's frequently a piggyback element at work. "There's often not just one cause or organ system that's to blame," Steege explains. "A chronic pain state may develop starting out with, say, endometriosis, and over time the surrounding organs start 'talking' to each other and develop pain. As the pain continues, the muscles of the pelvic floor can become involved and [they] become part of the chronic pain condition too." These far-reaching effects may partly explain why pelvic pain is one of the leading reasons for hysterectomy in the United States.
So, if chronic pain persists after you've been diagnosed and treated for one condition, it may be that the condition presumed to be the cause was either misdiagnosed in the first place or that another condition exists that also needs to be treated. "Chronic pain is complicated," Steege says, "so don't put all your faith in one diagnosis."--S.C.
Stacey Colino is co-author of Taking Back the Month: A Personalized Solution for Managing PMS and Enhancing Your Health (Perigee, 2002).
COPYRIGHT 2004 Weider Publications
COPYRIGHT 2004 Gale Group