Abstract
The in vitro performance of extemporaneously compounded morphine sulfate and oxycodone hydrochloride slow-release capsules was evaluated. Capsules containing varying amounts of morphine sulfate (15, 60, 200 mg) or oxycodone hydrochloride (10, 80, 200 mg) were prepared and provided by a Phoenix, Arizona, pharmacy. The capsules also contained 40% Methocel E4M Premium to slow the release of their active ingredient and sufficient lactose to fill the capsules. Three batches of each capsule strength were prepared, and replicates from each batch were evaluated using United States Pharmacopeia dissolution apparatus II. Samples were taken at regular time intervals over 24 hours. After 1 hour the pH of the dissolution medium was adjusted from 1.2 to 4.0, and after 2 hours the pH was adjusted to 6.8. The amount of drug released at each time point was determined spectrophotometrically. The compounded capsules released 14% to 23%, 67% to 85% and 93% to 98% of their active ingredient after 0.5, 4 and 12 hours, respectively. The relative standard deviations between the replicates from each batch were less than 10% for most time points. The percent of drug released over the first 4 hours was linear (r^sup 2^ = 0.9409-0.9999) when plotted versus time^sup 1/2^, indicating adherence to the simplified Higuchi model. Statistical analysis of the Higuchi dissolution constants indicated a significant difference (P
Introduction
Over the past 20 years, the practice of pharmaceutical compounding has re-emerged, with the US Food and Drug Administration (FDA) estimating that in 2002 approximately 1% to 8% of all prescription medications were compounded.1 Home health care, total parenteral nutrition and pain management in hospice care appear to be the major factors contributing to the increasing demand for compounded preparations.1 Owing to the high cost of drug product development, the pharmaceutical industry cannot provide medications to meet all patient needs at all times, especially for small patient populations and rare diseases.1 In addition, drugs that are in short supply, that are not yet available in the United States, and that cannot be patented often require compounding to be made available to patients.1-3 Needs for compounding also include preparing dosages and delivery systems that are not commercially manufactured, removing excipients that may cause allergic reactions, improving taste and making preparations of drugs that are too unstable for the development of manufactured products.14 Pharmaceutical compounding plays an integral role in ensuring successful pharmaceutical care by enabling individualized therapy and providing necessary medications when manufactured drug products are not available.2
Unfortunately, many compounded preparations have little, if any, research or regulatory basis for their safe and effective use.1 This increases the potential risk to patients, as indicated by several recent injuries and deaths resulting from improperly compounded preparations, particularly parenteral dosage forms.5-9 Most states do not require pharmacies to report the adverse events associated with compounded preparations to state or federal agencies.' As a result, a true indication of the frequency of such events is not available. However, the FDA has documented at least 71 adverse events involving compounded preparations since 1990.10 Some reports have attributed such incidents to a lack of proper training.1,2,10
Pharmaceutical compounding is a very small part of the curriculum in many schools of pharmacy, and most states do not ensure competency through practical skills testing or completion of certification programs. In addition, many individuals have not implemented adequate quality-control measures in their pharmacies.2,6,11,12 Many pharmacists also participate in pharmaceutical compounding for purely economic reasons instead of genuine medical needs.10 A pharmacy may he undermining the FDA's drug-approval process by distributing large quantities of compounded preparations or copying readily available commercial products.10,13
The occurrence of compounding errors and pharmacies acting as manufacturers under the guise of compounding has reflected negatively upon the compounding profession and has heightened governmental concern regarding the safety and quality of compounded preparations.10 In 1997, Congress enacted the Food and Drug Administration Modernization Act (FDAMA), which included a section clarifying the status of pharmacy compounding under federal law.14 However, the Supreme Court affirmed the 9th Circuit Court of Appeals' decision that found the section unconstitutional based upon violations of free speech.14,15 Therefore, pharmaceutical compounding is currently regulated primarily by state boards of pharmacy, which have limited resources.1,10 In response, the FDA has established a Compliancy Polity Guide for Pharmacy Compounding, which provides guidance on how the FDA intends to address pharmacy compounding after the invalidation of the compounding section in FDAMA.13,14 In addition, the Pharmacy Compounding Accreditation Board (PCAB) was recently established to help raise awareness and improve the quality of pharmaceutical compounding. The PCAB is a coalition of leading pharmacy-related professional and regulatory organizations that will create a voluntary accreditation program for compounding pharmacies. These organizations also provide numerous guidelines and references for compounding pharmacists, which help to improve the quality and standards of compounding practice and ensure patient safety.2,16,17
One type of product being compounded frequently is slow-release (SR) capsules.18-22 Such capsules are intended to prolong drug release over several hours, which decreases dosing frequency, and to lower fluctuations in blood levels, which reduces side effects and improves clinical results.20 Slow-release capsules typically employ controlled-release grades of Methocel E4M or KlOOM hypromellose to form a hydrophilic gel matrix, effectively trapping the active ingredient and slowing its release.21-23 Hypromellose is a water-soluble cellulose ether consisting of various amounts of methyl and hydroxypropyl substitutions and is widely used to control the release of active ingredients from manufactured tablets.24 Adequate control of drug release from such systems is dependent upon many variables, including the amount, purity, particle size, solubility and hydration rate of the cellulose polymer; the active ingredient; and any additional excipients.23 In addition, the manufacturer of Methocel (Dow Chemical Company, Midland, Michigan) does not provide any recommendations regarding its use in preparing SR capsules.24 Therefore, such preparations should be compounded only in special circumstances.25
Slow-release capsules are commonly prepared to deliver active ingredients for the treatment of chronic pain, which is a major health issue that significantly affects a person's quality of life and causes a substantial social burden.26 The Agency for Health Care Policy and Research guidelines recommend using the least invasive treatment methods and simplest dosing schedules when treating pain.26 Therefore, oral controlled-release (CR) dosage forms have been particularly important in optimizing pain management therapy.27 Oral administration is the most patient-preferred route of administration; and around-the-clock therapy lowers dosing frequency, improves compliance, provides more effective analgesia, reduces breakthrough pain, improves sleep and decreases side effects.26-28 Optimal pain management also requires the flexibility of prescribing the most appropriate active ingredients in the most appropriate doses.29 Opioids have played a very important role in the treatment of pain, with morphine sulfate setting the standard for years.27-29 However, morphine sulfate has a very short elimination half-life, and the most effective close for treating cancer pain ranges from 90 to 330 mg/day.26 As a result, several oral CR products containing morphine sulfate in a variety of dosages are currently available. In addition, oral CR oxycodone hydrochloride products have been shown to be equivalent to similar morphine sulfate products and provide an alternative for patients unable to tolerate morphine.29,30
Even with a large number of available manufactured products, the growth of specialized pain management and palliative care services has increased the need for individualized preparations to optimize patient therapy.21,22,31 Therefore, SR capsules containing morphine sulfate or oxycodone hydrochloride are frequently compounded. Due to the numerous factors influencing drug release from these preparations, pharmacists need to be cautious when preparing such formulations.21-23 Unfortunately, a literature search of Medline (1966-2004) and International Pharmaceutical Abstracts (1970-2004) revealed only two reports studying the release of morphine sulfate from SR capsules and none studying the release of oxycodone hydrochloride. Webster et al22 evaluated 30-mg morphine sulfate SR capsules compounded by 15 different pharmacies. The study compared the in vitro release of these preparations with manufactured immediate-release and CR products and evaluated the variability in the compounded preparations. Bogner et al21 tested 300-mg morphine sulfate SR capsules and evaluated the effect of formulation ingredients and preparation techniques upon their in vitro release characteristics.
This study evaluated the in vitro performance of morphine sulfate and oxycodone hydrochloride SR capsules that are currently being compounded by a local Phoenix, Arizona, pharmacy. The objectives of the study were (1) to determine the intrabatch and interbatch variation between the in rifro dissolution characteristics of the capsules, (2) to compare the dissolution characteristics of the capsules to those of equivalent-strength manufactured products and (3) to compare the release characteristics of different-strength capsules. The results of this study also provide pharmacists with additional information regarding the preparation of suitable SR capsules.
Materials and Methods
Materials
Morphine Sulfate Penta hydra te USP (Lot 2pms50006/c) and Oxycodone Hydrochloride USP (Lot 02oxy0027/a) were purchased from Medisca, Inc. (Plattsburgh, New York). Methocel FAM Premium CR-Grade (Lot C100847) and blue opaque No.1 gelatin capsule shells (Lot 92032) were purchased from Professional Compounding Centers of America, Inc. (PCCA) (Houston, Texas). Anhydrous Lactose NF (Lot rj1117) was purchased from Spectrum (Gardena, California). FD&C Blue No. 1 and No. 2 lake (Lot 966), FD&C Yellow No. 5 and No. 6 lake (Lot 443), brown food coloring No. 18 (Lot 13420), and green food coloring No. 18 (Lot 13210) were purchased from Kalchem International, Inc. (Lindsay, Oklahoma). White/clear No.l (Lot PH03011607), white/clear No. 3 (Lot PH02102206), and red/clear No. 3 (Lot PH03013005) capsule shells were purchased from Hawkins, Inc. (Minneapolis, Minnesota). Morphine Sulfate Extended-release (ER) Tablets (15 trig, Lot TK903A; 60 mg, Lot TJ747A; 200 mg, Lot TJ761 A) were purchased from Endo Pharmaceuticals (Chadds Ford, Pennsylvania), and Oxycontin tablets (10 mg, Lot WH621; 80 mg, Lot WJ531) were purchased from Purclue Pharma, L.P. (Stamford, Connecticut); the tablets had a weight variation of 1.5% to 2.4%. Hydrochloric acid (Lot 020024), glacial acetic acid (Lot 023960) and sodium hydroxide (Lot 041522) were purchased from Fisher Scientific (Pittsburgh, Pennsylvania). Phosphoric acid (Lot 03849PN) was purchased from Aldrich Chemical Company, Inc. (Milwaukee, Wisconsin). Water was purified using a Culligan Aqua-Summa II reagent-grade water system (Model 00401233) from Culligan International (Northbrook, Illinois).
Morphine sulfate (15, 60 and 200 mg) and oxycodone hydrochloride (10, 80 and 200 mg) SR capsules were compounded and provided by a local Phoenix, Arizona, pharmacy. The capsules contained 40% Methocel E4M Premium CR to slow the release of the active ingredient (Table 1). Three batches of each capsule preparation (100 capsules each) were compounded using a Janssun capsule-filling machine (Model 35-1673, PCCA). The capsules had a weight variation of 2.0 to 2.4%.
Methods
The in vitro dissolution of the compounded SR capsules and manufactured CR tablets was evaluated over 24 hours using United States Pharmacopeia (USP) dissolution apparatus II (Model VK7000, VanKel, Gary, North Carolina) at 37°C ± 0.5°C. Each vessel was filled with 900 mL of dissolution medium consisting of 0.05 M hydrochloride, 0.05 M phosphoric acid and 0.05 M glacial acetic acid at pH 1.2.22 The capsules were wrapped in USP-grade stainless steel wire (VanKel) to ensure their sinkability. Ten-milliliter samples were taken through a seventy-micrometer full-flow filter (Varian, Inc., Gary, North Carolina) at 0, 0.5, 1,2,3, 4, 6, 8, 12 and 24 hours. The sample volumes were replaced with fresh dissolution medium at the appropriate pH to maintain a constant volume. After 1 hour the pH of the dissolution medium was adjusted from 1.2 to 4.0, and after 2 hours the pH was adjusted to 6.8 using 30 mL and 20 mL of 4 M sodium hydroxide, respectively, to mimic the gastrointestinal (GI) environment. After 12 hours the paddle speed was increased from 50 to 100 rpm to ensure complete dissolution.
The amount of morphine sulfate and oxycodone hydrochloride in the release samples was determined spectrophotometrically at 285 and 280 nm, respectively, using a Perkin-Elmer Lambda EZ210 spectrophotometer (Model EZ210, Perkin-Elmer, Boston, Massachusetts). Reproducible calibration curves (2.5 x 10^sup -3^ to 2.5 x 10^sup -1^ mg/mL) for each active ingredient were prepared and showed linear relationships (r^sup 2^ = 0.996-0.999). The molar absorptivities of morphine sulfate and oxycodone hydrochloride were independent of pH, and the excipients showed no significant interference with the spectrophotometric analysis at 285 or 280 nm. The amount of morphine sulfate and oxycodone hydrochloride released after 24 hours was used to calculate percentage release, and the data were evaluated using the simplified Higiichi model: % release = (kt^sup 1/2^) × 100; k = Higuchi dissolution constant and t = time), which describes the release of water-soluble drugs from hydrophilic polymer matrices.32 The Higuchi dissolution constants were compared using one-way ANOVA and Tukey's Honestly Significantly Different tests at a significance level of α = 0.05.
Results and Discussion
Compounded morphine sulfate and oxycodone hydrochloride SR capsules were provided by a local Phoenix, Arizona, pharmacy to evaluate their in vitro dissolution characteristics. The capsules were prepared using 40% Methocel E4M to form a matrix system and to control the rate of drug release.24 Upon the patient's ingestion of the capsules, the gelatin shell begins to dissolve and water should hydrate the hydrophilic Methocel matrix, causing it to swell and form a viscous gel layer. Gel-layer formation must occur quickly to prevent disintegration of the capsule contents. The gel layer then controls the diffusion of water into the powder formulation. Over time, the outer gel layer begins to break down and dissolve. As this occurs, water penetrates deeper into the formulation, which forms a new viscous gel layer. This continues until the entire hydrophilic matrix has dissolved. Therefore, drug release may occur by two mechanisms: (1) diffusion out of the gel layer or (2) erosion of the gel matrix itself.23 Hydrophilic drugs, such as morphine sulfate and oxycodone hydrochloride, may be released by both processes, whereas hydrophobic drugs are only released by the erosion process. The ability of Methocel to control drug release depends upon several factors, including the amount, purity, particle size, solubility and hydration rate of the cellulose polymer; the active ingredient; and any additional excipients.23
The dissolution profiles for the morphine sulfate and oxycodone hydrochloride SR capsules showed a slow release of drug over time, as 100% release was not achieved prior to 12 hours (Figures IA & 2A). After 0.5 hours the SR capsules released 14% to 21% and 19% to 23% of morphine sulfate and oxycodone hydrochloride, respectively, indicating no dose dumping. After 4 to 5 hours the SR capsules released 67% to 76% of morphine sulfate and 71% to 85% of oxycodone hydrochloride, and after 11 to 12 hours, almost the entire amount of drug was released, with 83% to 97% of morphine sulfate and 93% to 98% oxycodone hydrochloride being released. Drug release from the SR capsules was also independent of pH, which was adjusted after 1 and 2 hours to mimic the GI environment. These results demonstrate that using 40% Methocel E4M Premium may be a viable method for preparing morphine sulfate and oxycodone hydrochloride SR capsules. The release characteristics of these capsules were also comparable to those of previously reported morphine sulfate SR capsules.21,22
Webster et al22 showed approximately 23%, 86% and 100% release of morphine sulfate by 0.5, 4 and 12 hours, respectively, when using 30% Methocel E4M. The lower percent release values in the present study may be attributed to using a greater amount of Methocel E4M. Bogner et al21 showed that as the level of Methocel was increased from 11% to 36%, the amount of morphine sulfate released after 0.5 hours decreased from ~16% to ~12%, and after 4 hours, the release decreased from ~98% to ~74%. It should be noted that Bogner et al21 used Methocel KlOOM instead of Methocel E4M. Both types are commonly used; however, the K form has a higher hydroxypropyl methyl substitution ratio.24 The hydroxypropyl groups are more hydrophilic and hydrate faster, which is important for rapid gel-layer formation and the slowing of drug release.
Several kinetic models have been used to describe drug dissolution from modified-release dosage forms." Using such mathematical equations, which describe drug release as a function of some parameter related to the dosage form, allows for quantitative interpretation of the values obtained from dissolution assays.32 The Higuchi model [% release = (kt^sup 1/2^) × 100] describes the release of water-soluble dugs from hydrophilic matrix systems. Such release is a diffusion process based upon Fick's Law, where the gelled polymer matrix acts as the diffusion medium.31,32 The morphine sulfate and oxycodone hydrochloride SR capsules contain water-soluble active ingredients within a hydrophilic matrix. Therefore, the percent of drug released from the capsules and equivalent-strength manufactured CR tablets was plotted versus t^sup 1/2^ (Figure 3). The linearity of these plots over the first 4 hours (r^sup 2^ = 0.9409-0.9999) suggests that during this time period the capsules and tablets released their active ingredient in accordance with the Higuchi model, indicating a diffusion-controlled process. The lack of linearity after 4 hours (Figure 3) may be due to substantial erosion of the polymer matrix; therefore, drug release would be occurring by a combination of mechanisms. It was observed during the study that upon dissolution of the capsule shell, the SR capsule formulations swelled but retained a capsule shape, indicating successful formation of a viscous gel layer. However, after approximately 4 to 6 hours, many of the formulations began showing signs of disintegration; and most were completely dissolved after 12 to 24 hours. Webster et al22 and Bogner et al21 quantified morphine sulfate release using a zero-order release model and the t^sub 30%^ - t^sub 80%^ interval, respectively. As a result, comparisons with their data cannot easily be made.
A majority of the dissolution time points for each morphine sulfate and oxycodone hydrochloride SR capsule batch resulted in relative standard deviation values of
The strengths of the morphine sulfate and oxycodone hydrochloride SR capsules used in this study were chosen to compare the dissolution characteristics of the capsules to those of CR tablets. However, compounding these strengths may not be appropriate because they have equivalent-strength manufactured products. The release profiles for the capsules were comparable to equivalentstrength tablets, but slight deviations were observed (Figures 1 and 2). After 0.5 hours the Oxycontin tablets showed a higher percent release compared with the SR capsules and morphine sulfate CR tablets. This may be explained by their biphasic drug-release mechanism, which consists of an immediate-release coating and a non-soluble extended-release matrix system. It was observed during the dissolution testing that the Oxycontin tablets quickly lost their coating; however, the tablet cores remained intact for the duration of the study. Like the SR capsules, the Morphine Sulfate ER tablets use a hydrophilic matrix system. Similar to the capsules, the tablets initially swelled and began showing signs of erosion after 4 to 6 hours, with complete disintegration occurring after 12 to 24 hours. Although the compounded SR capsules and manufactured CR tablets showed similar dissolution profiles (Figures 1 and 2), comparison of their Higuchi dissolution constants indicated that most of the SR capsules have a faster drug release than equivalent strength CR tablets (P
The dissolution profiles for the different-strength morphine sulfate and oxycodone hydrochloride SR capsules were comparable, but slight deviations were observed (Figures IA & 2A). Comparison of the Higuchi dissolution constants for the capsules showed statistical differences between the 15-mg and 200-mg morphine sulfate SR capsules and between all of oxycodone hydrochloride SR capsules (P
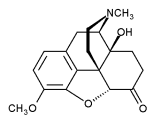
Formulation ingredients may also affect the hydration rate of the Methocel polymer, thereby altering dissolution characteristics.20 Hydrophilic active ingredients and excipients compete with the polymer for water and prevent proper gel-layer formation, which increases the rate of drug release.23 The SR capsules used in this study, as well as those used in previous studies,21,22 contained varying active ingredient:lactose:Methocel ratios. Since the amounts of these formulation ingredients and the net capsule weights are not independent of each other, it is difficult to determine the effect of each variable upon drug release. However, it has been recommended that the active ingredient:excipient:polymer ratio should remain constant, regardless of capsule size, to achieve similar release rates, provided there is some degree of compression within the capsule shell.23 Drug release from the 200-mg morphine sulfate and oxycodone hydrochloride SR capsules was not statistically different (P >0.05); therefore, it appears that the type of active ingredient in this case does not influence drug release. This is not unexpected because morphine and oxycodone have very similar chemical structures. However, because of all the factors mentioned previously, it cannot be expected that one SR capsule formulation will be applicable to all active ingredients.23
Conclusion
Pharmaceutical compounding has re-emerged in recent years as an important component of pharmaceutical care. However, much controversy exists concerning whether pharmacists can reliably compound safe and high-quality preparations. This study evaluated the in vitro dissolution characteristics of morphine sulfate and oxycodone hydrochloride SR capsules compounded and provided by a local Phoenix, Arizona, pharmacy. The results of the study indicate that using 40% Methocel E4M slows the release of morphine sulfate and oxycodone hydrochloride from compounded capsules. The in vitro dissolution characteristics of the SR capsules also showed little intrabatch and interbatch variation, even among different compounders, indicating reproducible and robust formulations. The dissolution profiles for the SR capsules and CR tablets were similar, but their Higuchi dissolution constants were statistically different. In vitro dissolution testing does not guarantee a correlation with in vivo results. Therefore, further studies are needed to determine whether these differences are clinically significant and to guarantee the safety and efficacy of these preparations. This study provides important information regarding these frequently compounded preparations that should help pharmacists prepare suitable formulations.
Acknowledgment
The authors would like to acknowledge Aline Cornelissen, MS, and Bianca Mendez, PharmD, for their technical support.
References
1. Coyne PJ, Hansen L, Watson A. Compounded drugs: Are customized prescription drugs a salvation, snake oil, or both? Am J Nurs 2003; 103(5): 78-85.
2. Allen LV Jr. Contemporary pharmaceutical compounding. Ann Pharmacother 2003; 37(10): 1526-1528.
3. Cabaleiro J. The compounding pharmacist: A home care and hospice partner. Home Healthc Nurse 2002; 20(6): 359-362.
4. Donnelly E. Our right to compound. Keeposted 2001; 26(Mar-Apr): 4-6.
5. [No author listed.] From the Centers for Disease Control and Prevention. Exophiala infection from contaminated injectable steroids prepared by a compounding pharmacy-United States, July-November 2002. JAMA 2003; 289(3):291-293.
6. Kastango ES. The cost of quality in pharmacy. J Pharm Technol2003; 19:49-53.
7. Suchard JR, Graeme KA. Pediatrie clonidine poisoning as a result of pharmacy compounding error. Pediatr Emerg Care 2002; 18(4): 295-296.
8. Romano MJ, Dinh A. A 1000-fold overdose of clonidine caused by a compounding error in a 5-year-old child with attention-deficit/hyperactivity disorder. Pediatrics 2001; 108(2): 471-472.
9. Seifert SA, Jacobitz K. Pharmacy prescription dispensing errors reported to a regional poison control center. J Toxicol CHn Toxicol2002; 40(7): 919-923.
10. Young D. Senate mulls oversight of pharmacy compounding. Am J Health Syst Pharm 2003; 60(23): 2402-2403.
11.Trissel L. Compounding our problems-again. Am J Health Syst Pharm 2003; 60(5): 432.
12.Kupiec TC. Ensuring compounding excellence: Quality control or quality assurance IJPC 2002; 6(2): 160.
13.Smith LK. Regulatory and operational issues of founding a compounding pharmacy. UPC2002; 6(6): 434-437.
14. [No author listed.] Compliance Policy Guide on Chapter 4 Human Drugs: section 460.200 pharmacy compounding. J Pain Palliat Care Pharmacother 2003; 17(1 ):99-106.
15. Vivian JC. Compounding and the Supreme Court. US Pharmacist 2002; 27(7): 70-77.
16. Newton DW. Compounding paradox: Taught less and practiced more. IJPC 2003; 7(5): 399-400.
17.Bormel G, Valentino JG, Williams RL. Application of USP-NF standards to pharmacy compounding. IJPC2003; 7(5): 361-363.
18.Smal J, Haapala O, Marvola M et al. Prolonged-release hard gelatin capsules of furosemide for the treatment of dogs. J Vet Pharmacol Ther 1995; 18(1):17-23.
19. Marvola M, Hannula AM, Klinge E et al. Effect of some cellulose derivatives as diluents on the bioavailability of ibuprofen capsules in man. Acta PharmaceutFenn WSl; 100(3): 211-218.
20.Timmons ED, Timmons SP Custom-compounded micronized hormones in a slow-release capsule matrix. IJPC20Q2; 6(5): 378-379.
21. Bogner RH, Szwejkowski J, Houston A. Release of morphine sulfate from compounded slow-release capsules: The effect of formulation on release. UPC2001; 5(5): 401-405.
22. Webster KD, AI-Achi A, Greenwood R. In vitro studies on the release of morphine sulfate from compounded slow-release morphine-sulfate capsules. IJPC1999; 3(5): 409-411.
23. Mullin S. Guidelines for compounding safe and uniform sustained release capsules. J Pharm Care Pain Sympt Control 1998; 6(2): 57-65.
24.[No author listed.] Using Methocel Cellulose Ethers for Controlled Release of Drugs in Hydrophilic Matrix Systems. Midland, Ml: The Dow Chemical Company; 2002. Form no. 198-02075-0702.
25. Alien LV Jr. The Art, Science, and Technology of Pharmaceutical Compounding. 2nd ed. Washington, DC: American Pharmaceutical Association; 2002:146.
26.Vallerand AH. The use of long-acting opioids in chronic pain management. Nurs Clin North Am 2003; 38(3): 435-445.
27.Reder RF. Opioid formulations: Tailoring to the needs in chronic pain. Eur J Pain 2001;5(SuppA):109-111.
28.Gourlay GK. Sustained relief of chronic pain: Pharmacokinetics of sustained release morphine. Clin Pharmacokinet 1998; 35(3): 173-190.
29. Levy MH. Advancement of opioid analgesia with controlled-release oxycodone. Eur J Pain 2001: 5(Supp A): 113-116.
30. Rischitelli DG, Karbowicz SH. Safety and efficacy of controlled-release oxycodone: A systematic literature review. Pharmacother 2002; 22(7): 898-904.
31. Latta KS. Extemporaneous compounding of pain and symptom control medications. J Pain Palliative Care Pharmacother 2002; 16(4): 51-60.
32. Siepmann J, Peppas NA. Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC). Adv Drug DelivRev2001; 48(2-3):139-157.
33. Costa P, Lobo JM. Modeling and comparison of dissolution profiles, fur J Pharm Sci 2001; 13(2): 123-133.
Dana L. Glowiak, BS
Department of Pharmaceutical Sciences
Julie L. Green, PharmD, RPh
Department of Pharmacy Practice
Bill J. Bowman, PhD, RPh
Department of Pharmaceutical Sciences
College of Pharmacy-Glendale
Midwestern University
Glendale, Arizona
Address correspondence to: Bill J. Bowman, PhD, RPh, Department of Pharmaceutical Sciences, College of Pharmacy-Glendale, Midwestern University, 19555 North 59th Avenue, Glendale, AZ 85308. E-mail: bbowma@midwestem.edu
Copyright International Journal of Pharmaceutical Compounding Mar/Apr 2005
Provided by ProQuest Information and Learning Company. All rights Reserved