Oxytocin
Oxytocin is a mammalian hormone that in women is released mainly after stimulation of the nipples or distention of the vagina and that facilitates birth and breastfeeding. It is also released during orgasm in both sexes. In the brain, it acts as a neurotransmitter and is involved in bonding and the formation of trust between people. more...
Synthetic oxytocin is sold as medication under the trade names Pitocin and Syntocinon and also as generic Oxytocin.
Synthesis, storage and release
Oxytocin is made in magnocellular neurosecretory cells in the supraoptic nucleus and paraventricular nucleus of the hypothalamus and is released into the blood from the posterior lobe of the pituitary gland. Oxytocin is also made by some neurons in the paraventricular nucleus that project to other parts of the brain and to the spinal cord.
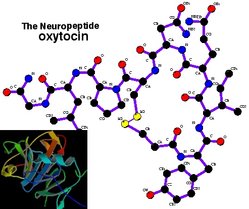
In the pituitary gland, oxytocin is packaged in large, dense-core vesicles, where it is bound to neurophysin as shown in the inset of the figure; neurophysin is a large peptide fragment of the giant precursor protein molecule from which oxytocin is derived by enzymatic cleavage.
Secretion is regulated by the electrical activity of the oxytocin cells in the hypothalamus. These cells generate action potentials that propagate down axons to the neurosecretory nerve endings in the pituitary; the endings contain large numbers of oxytocin-containing vesicles, which are released by exocytosis when the terminals are depolarised.
Structure and relation to vasopressin
Oxytocin is a peptide of nine amino acids (a nonapeptide). The sequence is cysteine - tyrosine - isoleucine - glutamine - asparagine - cysteine - proline - leucine - glycine (CYIQNCPLG). The cysteine residues form a sulfur bridge.
Oxytocin has a molecular mass of 1007 daltons. One international unit (IU) of oxytocin is the equivalent of about 2 micrograms of pure peptide.
The structure of oxytocin is very similar to that of vasopressin, which is also a nonapeptide with a sulfur bridge. Oxytocin and vasopressin are the only known hormones released by the human posterior pituitary gland to act at a distance. However, oxytocin neurons can make corticotropin-releasing hormone (CRH) and vasopressin neurons dynorphin, for example, that act locally. The magnocellular neurons that make oxytocin are adjacent to magnocellular neurons that make vasopressin, and are similar in many respects.
Oxytocin and vasopressin were discovered, isolated and synthesized by Vincent du Vigneaud in 1953, work for which he received the Nobel Prize in Chemistry in 1955.
The oxytocin receptor is a G-protein-coupled receptor which requires Mg2+ and cholesterol. It belongs to the rhodopsin-type (class I) group of G-protein-coupled receptors.
Actions
Oxytocin has peripheral (hormonal) actions, and also has actions in the brain.
Peripheral (hormonal) actions
The peripheral actions of oxytocin mainly reflect secretion from the pituitary gland. Oxytocin receptors are expressed by the myoepithelial cells of the mammary gland, and in both the myometrium and endometrium of the uterus at the end of pregnancy. In some mammals, oxytocin receptors are also found in the kidney and heart.
Read more at Wikipedia.org