The American Heart Association (AHA) has released a science advisory on the effects of antioxidant vitamin supplements on reducing the risk of cardiovascular disease. The full report appears in the August 3, 2004, issue of Circulation and is available online at http://circ.ahajournals.org/cgi/content/full/ 110/5/637.
The authors found that clinical trials generally have failed to demonstrate a beneficial effect of antioxidant supplements on cardiovascular morbidity and mortality. This lack of efficacy was demonstrated consistently for different doses of various antioxidants in diverse populations. Some smaller stud-ies did show benefits from [alpha]-tocopherol, [alpha]-tocopherol plus slow-release vitamin C, and vitamin C plus vitamin E on cardiovascular end points.
There is some evidence that antioxidant supplements may have adverse effects on cardiovascular end points. Some study results showed that antioxidant supplements may have interfered with the efficacy of statin-plus-niacin therapy, and that the addition of antioxidant vitamins blunted the expected rise in the protective high-density lipoprotein (HDL)-2 cholesterol and apolipoprotein A1 subfractions of HDL.
According to the advisory, the scientific data do not justify the use of antioxidant vitamin supplements for the prevention and treatment of cardiovascular disease. There are no consistent data to show that consuming micronutrients at levels exceeding those provided by a dietary pattern consistent with the AHA Dietary Guidelines will provide additional benefit. The authors state that this position is consistent with evidence-based guidelines for prevention of cardiovascular disease in women, which was released in 2004 by the AHA, and guidelines for patients with chronic stable angina released in 2002 from the American College of Cardiology. The advisory recommends achieving cardio-vascular risk reduction through long-term consumption of diets that are consistent with the AHA Dietary Guidelines and high in food sources of antioxidants and other cardioprotective nutrients, such as fruits, vegetables, whole grains, and nuts; long- term maintenance of a healthy body weight through balancing energy intake with regular physical activity; and attaining desirable blood cholesterol and lipoprotein profiles and blood pressure levels.
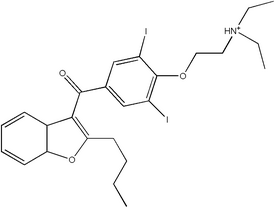
Medication Guide for Amiodarone
The U.S Food and Drug Administration (FDA) has mandated a medication guide for amiodarone. In 2004, approximately 3 million prescriptions were dispensed for amiodarone, a drug for heart arrhythmia. More than 90 percent of amiodarone prescriptions are filled with generic amiodarone. The medication guide was published by a manufacturer of branded amiodarone at the request of the FDA. The complete medication guide can be found online at http://www.wyeth.com/content/ShowLabeling.asp?id=470 and http://www.upshersmith.com/PDFs/Pacerone MedGuide.pdf.
Several factors may have led to the publication of the medication guide, including:
* The risks of using amiodarone as an antiarrhythmic agent. Serious side effects are associated with this agent (e.g., lung damage, liver damage, worse heartbeat problems) that can lead to death.
* Off-label prescribing for atrial fibrillation. The FDA has not approved amiodarone for the treatment of atrial fibrillation. Amiodarone is approved only for use in adults with ventricular arrhythmias (life-threatening heartbeat problems), for which other treatments did not work or were not tolerated.
* Concern that prescribing physicians and patients receiving amiodarone may not be fully informed of the risk of using this drug.
Physicians and patients may seek information about alternative medications to amio-darone that are approved by the FDA for the treatment of symptomatic atrial fibrillation without structural heart disease. Older patients may be at higher risk, because atrial fibrillation most commonly affects persons who are 50 years and older.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group