An Alternative High-Dose Weekly Schedule
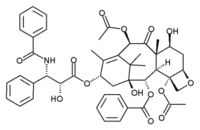
Study objectives: Sequential phase I and phase II trials of paclitaxel using an extended weekly schedule were performed to explore its effect on tolerance, limits of dose intensity, and activity at maximum dose intensity in disseminated non-small cell lung cancer (NSCLC).
Design: Patients with stage IIIB/IV NSCLC were eligible if they had a performance status of 0 to 2, no previous chemotherapy, and normal organ function. Paclitaxel was administered as a 3-h infusion weekly for 6 weeks of an 8-week cycle. Doses were modified for toxicity observed on the day of treatment. Measurements and results: Paclitaxel, 100 to 200 mg/[m.sup.2]/wk, was administered in the phase I trial. Dose escalation was limited primarily by neutropenia, and a relationship between dose and response was noted. A phase II trial of paclitaxel, 175 mg/ [m.sup.2]/wk, the maximum tolerated dose, was initiated; data are available for the first 25 patients. Eighty-three, 75, 58, and 50% of intended doses were delivered during cycles one to four, respectively. Grade 2 or 3 neuropathy occurred in nine patients, but improved in all following dose reduction. Platelet counts rose by 17,000/[micro]L/wk. Partial responses occurred in 14 of 25 patients (56%; confidence interval, 46 to 66%). The duration of response was 6 months, and 1-and 2-year survival rates were 53% and 18%, respectively.
Conclusion: Paclitaxel administered on a weekly schedule allows enhanced dose intensity, has a protective or stimulatory effect on platelets, and is active in NSCLC.
(CHEST 2000; 117:152S-155S)
Key words: dose intensity; maximum tolerated dose; non-small cell lung cancer; paclitaxel; platelets
Abbreviations: ANC = absolute neutrophil count; MTD = maximum tolerated dose; NSCLC = non-small cell lung cancer
Paclitaxel has demonstrated significant activity in non-small cell lung cancer (NSCLC)[1,2] and other malignancies,[3-5] but the optimal dose, schedule, and duration of administration have yet to be identified. Based largely on convenience, cost, and the need to prevent anaphylaxis, an intermittent schedule of paclitaxel given every 21 days using slow infusion, corticosteroids, and antihistamine premedication to deter hypersensitivity reactions has been widely used.[6] Conventional dosages range from 135 to 250 mg/[m.sup.2] infused over 1 to 24 h, but randomized trials completed to date have not shown a particular dose or infusion duration to be overwhelmingly superior.[7-9] Continuous or more frequent dosing schedules of this phase-specific agent,[10,11] may offer a theoretical advantage; however, randomized trials of these schedules do not exist, and limited data regarding alternative schedules have been published.
We recently completed two phase I trials using weekly administration of paclitaxel with radiation to take advantage of the properties of paclitaxel as a radiosensitizer. For patients with unresectable stage III NSCLC, the maximum tolerated dose (MTD) of a 3-h paclitaxel infusion administered with 60 Gy of thoracic radiation (2 Gy/d) was 60 mg/[m.sup.2] for each of 6 consecutive weeks.[12] Esophagitis, limited to the radiation field, precluded further dose escalation. Paradoxically, the anticipated toxicities of myelosuppression, neuropathy, and alopecia were not noted, even though a dose intensity equivalent to 210 mg/[m.sup.2] every 21 days was achieved.
In a similar phase I trial using weekly paclitaxel with cranial radiation in adult brain cancer, significantly greater doses were delivered with the same amelioration of toxicity.[13] Based on this apparent schedule-dependent moderation of toxicity, the Brown University Oncology Group initiated a series of trials designed to examine the response to extended delivery of weekly paclitaxel without radiation for patients with disseminated NSCLC.
PHASE I TRIAL OF WEEKLY PACLITAXEL
The goal of this phase I trial was to determine the maximum dose intensity of weekly paclitaxel that could be administered safely as outpatient therapy for advanced NSCLC.[14] Since a weekly schedule necessitated repeated dosing before the full degree of acute drug-related toxicity may be manifested, the traditional, phase I, dose-escalation format was modified to allow scheduled dose reduction for moderate hematologic or neurologic toxicity based on the day of treatment (Table 1). In this fashion, the dose escalation was tailored to the observed toxicity of the individual in an attempt to preclude severe toxicity, while still maintaining the escalation of the dose level. For this reason, tolerance was defined by both observed toxicity and the number of dose modifications. We postulated this approach to allow the opportunity to maximize dose intensity.
Table 1--Dose Modifications (Based on Day of Treatment)
Materials and Methods
Eligibility requirements included either relapsed or unresectable NSCLC, a performance status of 0 to 2, and adequate organ function. Prior radiation therapy was acceptable, but prior chemotherapy for metastatic disease was not allowed. Paclitaxel was administered as a 3-h IV infusion given for 6 consecutive weeks of each 8-week cycle. Anaphylaxis premedication included diphenhydramine, 25 mg, and ranitidine, 50 mg, administered IV 1 h prior to paclitaxel administration and dexamethasone, 20 mg orally, on the evening prior to and on the morning of paclitaxel administration. In the event that a patient omitted an oral dose of dexamethasone, the dose was replaced with an IV dose 1 h before paclitaxel administration. A CBC count was performed each week on the day of treatment, and liver enzymes were measured every 4 weeks. A restaging was performed to evaluate response at the completion of each 8-week cycle. Patients without disease progression continued to receive subsequent cycles without dose escalation. Patients with progressive disease were removed from study.
The initial dosage of paclitaxel was 100 mg/[m.sup.2]/wk. Three consecutive patients were entered at each dose level. If [is less than] 80% of the scheduled cumulative dose of paclitaxel in the first cycle was delivered, grade 2 neurotoxicity or grade 3 nonhematologic toxicity developed in any patient, the level was expanded to six patients. Unacceptable toxicity was established when [is greater than or equal to] 50% of patients at a dose level met these criteria; the MTD was defined as the dose preceding this level. If dose-limiting toxicity did not occur, three new patients were entered to the subsequent dose levels, planned at 125, 135, and 150 mg/[m.sup.2], with further increases at 25-mg/[m.sup.2] increments.
Paclitaxel doses were modified for toxicity determined on the day of treatment (Table 1). In the event of granulocyte counts [is less than] 1,800/[micro]L or platelet counts [is less than] 100,000/[micro]L, the paclitaxel dose was decreased by 50%; when granulocyte counts were [is less than] 1,000/[micro]L or platelet counts [is less than] 75,000/[micro]L, a dose was omitted. In addition, doses were decreased by 50% when grade 2 sensory or motor neuropathy occurred, and were omitted in the event of grade 3 or grade 4 neuropathy. When a dose reduction for neuropathy occurred, all future doses for that patient were limited to 50% of original dose, regardless of degree of neurologic recovery. Other grade 3 and grade 4 toxicities also triggered dose omission.
Results
There were 26 patients entered at six dose levels. Two patients were ineligible to be evaluated for toxicity, one due to underlying liver disease and the other due to volitional withdrawal before completion of the first cycle. Three patients received paclitaxel at each of the dosage levels: 100, 125, 135, and 150 mg/[m.sup.2]/wk. All but one dose was received, and no grade 3/4 toxicity directly attributable to paclitaxel occurred during the first cycle. One patient at the 125-mg/[m.sup.2] level developed an uncomplicated pneumonia that was not associated with neutropenia. One patient receiving 150 mg/[m.sup.2] required a transfusion of RBCs, and a second patient developed Aspergillus esophagitis (possibly related to steroids). At the 175-mg/[m.sup.2] dose level, patient accrual was expanded to six due to dose reductions for asymptomatic neutropenia (absolute neutrophil count [ANC] [is less than] 1,000/[micro]L), which caused two patients to receive [is less than] 80% of the scheduled dose. The remaining four patients received full doses without excessive toxicity.
Six patients were entered to receive 200 mg/[m.sup.2]/wk, but only one completed the first cycle without dose reduction or undue toxicity. This patient subsequently developed a grade 3 sensory-motor neuropathy and a grade 3 rash at the beginning of the second cycle. The remaining five patients received [is less than] 80% of the intended dose for a variety of reasons. Thus, dose escalation was ceased at 200 mg/[m.sup.2]/wk, and 175 mg/[m.sup.2]/wk was defined as the MTD.
Ten patients who did not demonstrate disease progression were available for evaluation of long-term toxicity. Subsequent courses were delivered at the initially assigned dose level. The only patient continuing therapy at the 200-mg/[m.sup.2] dose level was reassigned to 175 mg/[m.sup.2] when it was established as the MTD. A maximum of 12 cycles were delivered: three patients completed 2 cycles, two patients completed 3 cycles, one patient each completed 4, 5, 6, and 12 cycles. All but two patients discontinued therapy on eventual disease progression. One patient withdrew after three cycles (24 weeks), and the last patient withdrew for prolonged neuropathy.
Neuropathy was both cumulative and dose-related. Grade 2 and grade 3 neuropathy occurred in five patients (21%). Grade 3 neuropathy developed in one patient at the 175-mg/[m.sup.2] dose level during the second cycle, and in another at the 200-mg/[m.sup.2] dose level following the first cycle. Symptoms improved to grade 2 in both patients, and therapy was reinstituted with a 50% dose reduction. Grade 2 neuropathy developed in one patient at 175 mg/[m.sup.2] (third cycle), in one patient at 200 mg/[m.sup.2], and in one patient at 125 mg/[m.sup.2] (fifth cycle). Symptoms improved with dose reduction in all of these cases. Many patients noted subjective improvement in symptoms during the scheduled breaks at weeks 7 and 8, which may have contributed neurologic tolerance.
Responses and survival were greater for dosages of paclitaxel [is greater than or equal to] 175 mg/[m.sup.2]/wk. Although response occurred at the highest and lowest levels, 3 of 12 patients responded at dosages of paclitaxel [is less than] 175 mg/[m.sup.2]/wk, but 6 of 12 patients responded at higher doses. In addition, survival was significantly longer (24.9 weeks vs 45.1 weeks; p [is less than] 0.01 log-rank) for dosages [is greater than or equal to] 175 mg/[m.sup.2]/wk.
PHASE II TRIAL OF WEEKLY PACLITAXEL
Accordingly, a phase II trial was initiated to evaluate the response, survival, and toxicity of paclitaxel 175 mg/[m.sup.2]/wk (the MTD determined from the phase I trial) in the treatment of advanced NSCLC. Patient eligibility and study design were identical to those used for the phase I trial, except for the dose modification criteria: dose reduction was initiated for ANC [is less than] 1,500/[micro]L, rather than the 1,800/[micro]L used in the phase I trial. Modification for neurologic toxicity was unchanged (Table 1).
Results
The following are preliminary data from the first 25 of 30 patients entered on this trial. There were 18 men and 7 women, with a median age of 65 years (range, 37 to 78 years). Stage IV disease occurred in 24 patients, and 14 patients had received prior radiation treatment. Brain metastases had been previously treated in 11 patients.
Eighty-three percent of the intended first cycle dose was delivered due to scheduled dose modification. Doses were reduced, most commonly for neutropenia, especially in the third and sixth weeks, but blood count recovery was rapid. Figure 1 shows counts for a representative patient. In cycles 2 to 5, 75%, 58%, 50%, and 50% of intended doses were delivered, respectively.
[Figure 1 ILLUSTRATION OMITTED]
Grade 2 and grade 3 neuropathy became increasingly frequent and limited dose intensity in later cycles. Overall, only 32% (8 of 25) of patients developed significant (grade 9. or 3) neuropathy. It was rare in the first cycle, but occurred universally by the fourth 8-week cycle. Subjective improvement was noted by many patients during the 2-week interval between cycles. Grade 3 toxicities improved to grade 2 with the prescribed dose modifications in all patients, and most patients with grade 9. toxicities noted continued improvement in their symptoms, even during continued therapy.
An analysis of hematologic toxicity was remarkable for an unanticipated rise in platelets (Fig 2). During each week of therapy, the platelet count rose by 17,000/[micro]L per week and dropped back to normal between cycles. This cumulative rise approximates 100,000/[micro]L/6-week course. A similar trend was observed during each of the first three cycles, and was not affected by whether patients received more or less than four of the six intended doses. No thrombotic events were recorded during this trial.
[Figure 2 ILLUSTRATION OMITTED]
Objective responses (all partial) were observed in 14 of 25 (56 [+ or -] 10%) patients, and all occurred during the first cycle of treatment. Those that did not respond by the end of the first cycle did not respond subsequently. The median duration of response was 6.5 months. The 1-year survival rate was 53%, and the 2-year survival rate was 18%.
DISCUSSION
Paclitaxel administered on a weekly schedule is well tolerated and appears to demonstrate an improved therapeutic index compared with the standard schedule. The dose of 175 mg/[m.sup.2]/wk over the first 6 weeks, the equivalent of 525 mg/[m.sup.2] on a g 1-day schedule, yields a threefold increase in dose intensity. Hematologic toxicity is limiting acutely, but neurologic toxicity becomes dose limiting with extended therapy. Remarkably, patients who develop significant neurologic toxicity are able to continue therapy or even demonstrate improvement in symptoms with dose reduction. Long term, the therapy is well tolerated, and some patients have remained on therapy [is greater than] 2 years.
The rising platelet count noted during paclitaxel treatment is a novel observation. It appears to be independent of the weekly schedule because it occurred whether patients received more or less than four of the planned six doses. It is possible that the concurrent use of dexamethasone may have contributed, but we believe it to be an independent effect of the paclitaxel. It likely has been overlooked in other single-agent paclitaxel trials because toxicity scoring systems only highlight platelet declines. This phenomenon may explain the reports of improved platelet tolerance following carboplatin when paclitaxel is administered concurrently.[15]
Despite the apparent amelioration of toxicity associated with this weekly schedule, the response rate of [is greater than] 50% compares favorably with other single-agent trials (10 to 24%) or multiagent trials (30 to 63%) in advanced NSCLC. The 1- and 2-year survival rates of 53% and 18%, respectively, are also quite substantial when one considers the large fraction of these patients (40%) with preexisting brain metastases and the low number of stage IIIB patients included. Another important observation is the suggestion of improved efficacy of response rates and survival noted at dosages [is greater than or equal to] 175/[m.sup.2]/wk. Further investigation will be required to determine whether the activity observed in this trial is due to enhanced dose intensity, the weekly schedule, the frequency of paclitaxel levels exceeding a threshold dose, or a combination of these factors. A randomized trial is needed to compare the relative efficacy of the weekly schedule vs a conventional schedule.
REFERENCES
[1] Chang AY, Kim K, Glick J, et al. Phase II study of Taxol, merbarone, and piroxantrone in stage IV non-small cell lung cancer: the Eastern Cooperative Ontology Group results. J Natl Cancer Inst 1993; 85:388-394
[2] Murphy WK, Fossella FV, Winn RJ, et al. Phase II study of Taxol in patients with untreated non-small cell lung cancer. J Natl Cancer Inst 1993; 85:384-388
[3] Wiernik P, Schwartz E, Einzig A, et al. Phase I trial of Taxol given as a 24-hour infusion every 21 days: responses observed in metastatic melanoma. J Clin Oncol 1987; 5:1232-1239
[4] Donehower R, Rowinsky E, Grochow L, et al. Phase I trial of Taxol in patients with advanced cancer. Cancer Treat Rep 1987; 71:1171-1177
[5] Holmes FA, Walters RS, Therialt RL, et al. Phase II trial of Taxol, an active drug in metastatic breast cancer. J Natl Cancer Inst 1991; 17:1797-1805
[6] Arbuck S, Canetta R, Onetto O, et al. Current dosage and schedule issues in the development of paclitaxel. Semin Oncol 1993; 20(suppl 3):31-39
[7] Nabholtz J, Gelman K, Bontenbal M, et al. Multicenter, randomized comparative study of two doses of paclitaxel in patients with metastatic breast cancer, J Clin Oncol 1996; 14:1858-1867
[8] Bonomi P, Kim K, Chang A, et al. Phase II trial comparing etoposide, cisplatin versus Taxol, cisplatin, G-CSF versus Taxol, cisplatin in advanced non-small cell lung cancer [abstract 1145]: an ECOG thai. Proc Am Soc Clin Oncol 1996; 15:382
[9] Eisenhauer E, Huinink W, Swenerton K, et al. European-Canadian randomized trial of paclitaxel in relapsed ovarian cancer: high-dose versus low-dose and long versus short infusion. J Clin Oncol 1994; 12:2654
[10] Parness J, Horwitz SB. Taxol binds to polymerized tubulin in vitro. J Cell Biol 1981; 91:479-487
[11] Manfredi JJ, Parness J, Horwitz SB. Taxol binds to cellular microtubules. J Cell Biol 1982; 94:688-696
[12] Choy H, Akerley W, Safarin H, et al. Phase I trial of paclitaxel and thoracic radiation in NSCLC. J Clin Oncol 1994; 12: 2682-2686
[13] Glantz M, Choy H, Kearns C, et al. Phase I study of weekly outpatient astrocytomas. J Clin Oncol 1996; 14:600-609
[14] Akerley W, Glantz M, Choy H, et al. Phase I trial of weekly paclitaxel in advanced cell lung cancer, J Clin Oncol 1998; 16:153-158
[15] Kearns C, Egorin M. Considerations regarding the less-than expected thrombocytopenia encountered with combination paclitaxel/carboplatin chemotherapy. Semin Oncol 1997; 24(suppl 2):91-96
(*) From the Brown University Oncology Group, Providence, RI.
Correspondence to: Wallace Akerley III, MD, Rhode Island Hospital, Division of Oncology, 593 Eddy St, Providence, RI 02903; e-mail: akerley@brown.edu
COPYRIGHT 2000 American College of Chest Physicians
COPYRIGHT 2000 Gale Group