What are rebound headaches?
Headaches that happen every day or almost every day may be caused by overuse of pain medicines. Often these headaches begin early in the morning. The location and severity of the headache may change from day to day. People who have rebound headaches also may have nausea, anxiety, irritability, depression, or problems sleeping.
What kinds of medicine can cause rebound headache?
Both prescription and over-the-counter medicines for migraine (such as aspirin and acetaminophen) can cause headache if you take them too often. These medicines should not be taken on more than two days per week. Sedatives, tranquilizers, and ergotamine medicines also can cause rebound headache. Talk with your doctor to find out if you should stop taking these medicines, or take less of them.
Should I stop taking certain medicines?
Talk to your doctor about the medicines you are taking. You can safely stop taking some medicines right away. Other kinds of medicine have to be slowly reduced, little by little. After stopping the medicine that is giving you rebound headaches, your headaches may get worse for a few days. Do not make changes to your drug plan without talking with your doctor.
What effect does caffeine have on headaches?
Caffeine is an ingredient in some headache medicines. It may make your headache feel better for a little while. But if you take medicine with caffeine every day, or if you drink a beverage with caffeine every day, you might get more headaches. If your headache gets worse when you stop having caffeine, the caffeine may be causing some of your headaches.
How should I use medicine for my daily headaches?
There are several common medicines to prevent headaches. Medicines to prevent headache have to be taken every day. Here are some medicines that prevent headaches:
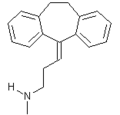
* Tricyclic antidepressants, such as amitriptyline (brand name: Elavil) and nortriptyline (brand name: Pamelor)
* Antiepileptic drugs, such as valproic acid (brand name: Depakote), gabapentin (brand name: Neurontin), and topiramate (brand name: Topamax)
* Beta blockers, such as propranolol (brand name: Inderal)
These medicines can help you get fewer headaches. But they will not stop every headache. It may take six weeks or more for your medicine to start working. Talk to your doctor about which medicines are right for you. It is important to follow your doctor's directions when you take these medicines.
What can I do to help my headaches?
Take medicines only as directed by your doctor. Take only the headache medicines recommended by your doctor, including over-the-counter medicines. Always have your medicines with you in case you begin to get a headache. Keep a headache diary so you and your doctor know what helps and when you are getting headaches.
Following a regular daily pattern will help. Eat meals at regular hours and do not skip breakfast. Fasting is a common cause of headache. Go to bed and get up at the same time every day. Regular aerobic exercise is helpful. You should exercise at least 20 minutes a day, three days a week. Yoga, meditation, relaxation therapy, and simple pleasurable activities may help. Your doctor may ask you to keep a headache calendar to help track your headache progress.
What about natural therapies and alternative medicines?
Natural supplements that may help to prevent your migraines include vitamin [B.sub.2], magnesium, feverfew, coenzyme [Q.sub.10], and butterbur root (Petasites hybridus). Many patients seek alternative therapies for headache relief. Acupuncture or chiropractic treatments may help your headaches. But, there is no proof that these treatments help. Be sure to tell your doctor about any natural medicines or supplements you are taking.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group