Study objectives: Stroke volume variation (SVV) and pulse pressure variation (PPV) determined by the PiCCOplus system (Pulsion Medical Systems; Munich, Germany) may be useful dynamic variables in guiding fluid therapy in patients receiving mechanical ventilation. However, with respect to the prediction of volume responsiveness, conflicting results for SVV have been published in cardiac surgery patients. The goal of this study was to reevaluate SVV in predicting volume responsiveness and to compare it with PPV.
Design: Prospective nonrandomized clinical investigation.
Setting: University-based cardiac surgery.
Patients: Forty patients with preserved left ventricular function undergoing elective off-pump coronary artery bypass grafting.
Interventions: Volume replacement therapy before surgery.
Measurements and results: Following induction of anesthesia, before and after volume replacement (6% hydroxyethyl starch solution, 10 mL/kg ideal body weight), hemodynamic measurements of stroke volume index (SVI), SVV, PPV, global end-diastolic volume index (GEDVI), central venous pressure (CVP) and pulmonary capillary wedge pressure (PCWP) were obtained. Also, left ventricular end-diastolic area index (LVEDAI) was assessed by transesophageal echocardiography. Prediction of ventricular performance was tested by calculating the area under the receiver operating characteristic (ROC) curves and by linear regression analysis; p < 0.05 was considered significant. All measured hemodynamic variables except heart rate changed significantly after fluid loading. GEDVI, CVP, PCWP, and LVEDAI increased, whereas SVV and PPV decreased. The best area under the ROC curve (AUC) was found for SVV (AUC = 0.823) and PPV (AUC = 0.808); the AUC for other preload indexes ranged from 0.493 to 0.636. A significant correlation with changes of SVI was observed for SVV (r = 0.606, p < 0.001) and PPV (r = 0.612, p < 0.001) only. SVV and PPV were closely related (r = 0.861, p < 0.001). Conclusions: In contrast to standard preload indexes, SVV and PPV, comparably, showed a good performance in predicting fluid responsiveness in patients before off-pump coronary artery bypass grafting.
Key words: cardiac preload assessment; cardiac surgery; pulse contour analysis; pulse pressure variation; stroke volume variation
Abbreviations: AUC = area under the curve; CO = cardiac output; CVP = central venous pressure; GEDV = global end-diastolic volume; GEDVI = global end-diastolic volume index. LVEDA = left ventricular end-diastolic area; LVEDAI = left ventricular end-diastolic area index. PCWP = pulmonary capillary wedge pressure; PPV = pulse pressure variation; ROC = receiver operating characteristic. SPV = systolic arterial pressure variation. SV = stroke volume; SVI = stroke volume index; SVV = stroke volume variation; TEE = transesophageal echocardiography
**********
Adequate volume replacement to achieve optimal cardiac performance is a primary goal of hemodynamic management in patients undergoing off-pump coronary artery bypass grafting. (1) Frequently used standard preload indexes such as central venous pressure (CVP) or pulmonary capillary wedge pressure (PCWP) often fail to provide reliable information on cardiac preload and are not capable of predicting a cardiac response to fluid therapy. (2,3) As an alternative to these static variables, assessment of stroke volume variation (SVV, expressed as percentage) has been used as a dynamic monitoring for guiding fluid therapy in patients receiving mechanical ventilation. (4) Cardiac preload is highly susceptible to changes in intrathoracic pressure induced by mechanical ventilation: as stroke volume (SV) varies, systolic arterial pressure variation (SPV) and arterial pulse pressure variation (PPV) can be observed. Both SPV and PPV are pronounced during hypovolemia, and variation decreases if intravascular blood volume is restored; they have shown to reliably predict changes in cardiac output (CO) related to volume replacement. (5-7) However, both SPV and PPV are also influenced by vasomotor tone, which is supposed to be less the case with SVV; therefore, assessment of SVV is thought to be more accurate. (8)
An estimate of both PPV and SVV is displayed in real-time by the PiCCOplus system (Pulsion Medical Systems; Munich, Germany), a continuous CO monitoring device based on arterial pulse contour analysis. (9,10) Conflicting results have been published regarding the clinical use of this SVV variable in cardiac surgery patients: although SVV was able to predict fluid responsiveness in patients after cardiac surgery as reported by Beuter et al, (11,12) Wiesenack and colleagues (13) could not confirm these results in a study performed before cardiac surgery. Both PPV and SVV have been shown to be closely correlated. (14) However, to our knowledge no data on comparison of these variables regarding prediction of fluid responsiveness are available.
The aim of this study was to reevaluate the value of SVV regarding the prediction of volume responsiveness and to compare it with PPV as well as the standard preload variables in a clinical setting in patients before elective off-pump coronary artery bypass grafting.
MATERIALS AND METHODS
Patients and Anesthesia
With local ethics committee approval and patient written informed consent, 40 patients (American Society of Anesthesiologists class III; mean age [+ or -] SD, 62 [+ or -] 7 years; body mass index, 27 [+ or -] 3; left ventricular ejection fraction, 65 [+ or -] 6%) undergoing elective off-pump coronary artery bypass grafting were included in the study. Patients with preoperative dysrhythmias, reduced left and right ventricular function (ejection fraction < 40%), valvular heart disease, intracardiac shunts, pulmonary artery hypertension, or severe peripheral vascular obstructive disease were excluded.
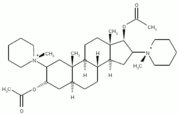
After application of the routine hemodynamic monitoring according to institutional standards (pulse oximetry, five-lead ECG, and noninvasive BP monitoring [CMS; Philips Medical Systems; Andover, MA]) and the insertion of arterial and peripheral IV lines, anesthesia was induced using fentanyl (10 to 30 [micro]g/kg IV), lidocaine (1.5 mg/kg IV), and propofol (up to 2 mg/kg IV) and was maintained with propofol (1.5 to 3 mg/kg/h) and fentanyl. Neuromuscular blockade was achieved with pancuronium bromide (0.1 mg/kg IV). Following endotracheal intubation, mechanical ventilation was performed without positive end-expiratory pressure using an inspired oxygen concentration of 50% and tidal volumes of 10 mL/kg to maintain an end-expiratory PC[O.sub.2] at 4 to 4.5 kPa during the study period. Effective applied mean tidal volumes were 698 [+ or -] 79 mL, and peak airway pressures ranged from 8 to 25 cm [H.sub.2]O (mean, 17 [+ or -] 3 cm [H.sub.2]O).
Hemodynamic Assessment and Study Protocol
After induction of anesthesia, a standard 7.5F pulmonary artery catheter (Swan-Ganz Thermodilution Catheter; Edwards Lifescience LLC; Irvine, CA) was introduced via right internal jugular vein access. CVP and PCWP were measured using standard transducers and displayed on the monitor (CMS; Philips Medical Systems). Pressure transducers were zeroed at midaxillary level to ambient pressure. A 4F thermistor-tipped arterial catheter (Pulsiocath; Pulsion Medical Systems) was inserted in the left femoral artery and connected to the stand-alone monitor PiCCOplus (computer version 5.2.2; Pulsion Medical Systems). Transpulmonary thermodilution measurements of 15 mL of normal iced saline solution were performed to determine CO and SV. These measurements were made by the same observer to avoid interobserver variation. Global end-diastolic volume (GEDV) is calculated from CO, mean transit time, and dovmslope time of the indicator: GEDV = CO X (mean transit time - down-slope time). Transpulmonary thermodilution is used to calibrate pulse contour analysis for continuous CO monitoring and SVV. SVV, as a percentage change of SV during the ventilatory cycle, is assessed according to the following equation: SVV(%) = (maximum SV - minimum SV)/mean SV, where maximum and minimum SV are mean values of the four extreme values of SV during a period of 30 s, and mean SV is the average value for this time period. Additionally, using the PiCCOplus system, PPV can be determined during the same time interval: PPV(%) = (maximum pulse pressure - minimum pulse pressure)/mean pulse pressure, where maximum and mean pulse pressure are mean values of the four extreme values of pulse pressure, and mean pulse pressure is the average value for this time period. The system, the related methods, and the currently used algorithm integrating aortic compliance and systemic vascular resistance have been described in detail elsewhere. (9,15) For transesophageal echocardiography (TEE), a Philips SONOS 5500 system with an Omniplane III TEE probe (Philips Medical Systems, Andover, MA) was used. The probe was positioned to obtain the transgastric, midpapillary, short-axis view of the left ventricle. Left ventricular end-diastolic area (LVEDA) was measured by manual planimetry of the area circumscribed by the leading-edge technique of the endocardial border in this position. LVEDA was determined, recorded, and calculated by the same experienced examiner who was blinded to the results of the hemodyuamic measurements throughout the study.
On completion of baseline measurements and prior to any surgical intervention, volume replacement using 6% hydroxyethyl starch solution was performed (mean molecular weight, 130,000 d/mean degree of substitution, 0.4; Voluven; Fresenius Kabi; Stans, Switzerland), 10 mL/kg ideal body weight over 20 min, resulting in applied volumes of 695 [+ or -] 65 mL. Immediately thereafter, all hemodynamic measurements including TEE were repeated.
Data Analysis
All hemodynamic variables were recorded as mean of three repeated measurements, and CO, SV, GEDV, and LVEDA were post hoc indexed to body surface area using the "du Bois formula" (body surface area = body weight [[kilograms].sup.0.425] x body length [[centimeters].sup.0.725] x 71.84). (16) Statistical analysis was performed using statistical software (Statview 5.01; SAS Institute; Cary, NC; and SPSS 10.0; SPSS; Chicago, IL). A student t test was used for comparison of hemodynamic data before and after fluid bolus. A Pearson correlation between changes of SVI and changes of the different hemodynamic variables was established. Prediction of fluid responsiveness for SVV, PPV, and standard preload indexes was tested by calculating the area under the receiver operating characteristic (ROC) curve for a SV index (SVI) increase of [greater than or equal to] 25% (area under the curve [AUC] = 0.5: not better than chance, no prediction possible; AUC = 1.0: best possible prediction). Furthermore, regression analysis was performed for preload variables and changes of SVI related to the fluid bolus. Comparison between SVV and PPV was done by Bland-Altman analysis and Pearson correlation. ROC curves of SVV and PPV were compared according to Hanley and McNeil. (17) Linear correlations of SVV vs changes of SVI and PPV vs changes of SVI were compared using Fisher z-transformation and Hotelling Williams test. A p value < 0.05 was considered to be statistically significant. Unless otherwise stated, data are presented as mean [+ or -] SD.
RESULTS
From 40 patients studied, 35 complete data sets were available for statistical analysis. Volume replacement resulted in significant changes of all measured hemodynamic variables except heart rate: mean arterial pressure, mean pulmonary artery pressure, CVP, PCWP, LVEDA index (LVEDAI), cardiac index, SVI, and GEDV index (GEDVI) increased, whereas systemic vascular resistance index, PPV, and SVV decreased (Table 1).
Mean increase of SVI as a result of volume loading was 27 [+ or -] 13% (Fig 1, top, a). Twenty-one patients (60%) had an increase of SVI [greater than or equal to] 25% (mean, 34 [+ or -] 7%). In five patients (14%), a SVI increase [less than or equal to] 10% was observed (mean, 7 [+ or -] 3%). Mean decrease of SVV was -8 [+ or -] 4% and of PPV was -9 [+ or -] 3% (Fig 1, center, b and bottom, c). For patients with an increase of SVI [greater than or equal to] 25%, SVV at baseline was 15 [+ or -] 4% and PPV was 16 [+ or -] 3%. In patients with an SVI increase [less than or equal to] 10%, SVV at baseline was 10 [+ or -] 2% and PPV was 8 [+ or -] 3%. Percentage changes ([DELTA]) of SVV, PPV, GEDVI, and LVEDAI correlated significantly with [DELTA]SVI, but [DELTA]CVP and [DELTA]PCWP did not correlate with [DELTA]SVI (Table 2). Furthermore, a significant positive correlation was found for [DELTA]GEDVI with [DELTA]LVEDAI (r = 0.635, p < 0.001), whereas correlations for [DELTA]CVP and for [DELTA]PCWP with [DELTA]LVEDAI were not significant (r = 0.200, p = 0.432, and r = 0.051, p = 0.872, respectively).
[FIGURE 1 OMITTED]
Results of ROC curve analysis and linear regression analysis are summarized in Table 3. The best AUC to identify a 25% increase in SVI was seen with SVV and PPV (Fig 2). The optimal threshold value given by the ROC analysis was 12.5% for SVV: in patients with SVV [greater than or equal to] 12.5% at baseline, a response to subsequent fluid replacement therapy by an increase of SVI [greater than or equal to] 25% could be expected with a sensitivity of 74% and a specificity of 71%. This threshold value was 13.5% for PPV (sensitivity, 72%; specificity, 72%). Only for SVV and PPV were significant correlations observed with [DELTA]SVI induced by the fluid bolus (Fig 3).
[FIGURES 2-3 OMITTED]
SVV and PPV were closely related (r = 0.897, p < 0.001). Bland-Altman analysis (SVV-PPV) revealed a mean bias [+ or -] 2 SD (limits of agreement) of 1 [+ or -] 4%. ROC curves for SVV and PPV did not show a significant difference (p = 0.456), nor did correlations of SVV before fluid load with [DELTA]SVI and PPV before fluid load with [DELTA]SVI (p = 0.698).
DISCUSSION
SVV and PPV assessed by pulse contour analysis using the PiCCOplus system were comparable predictors of changes in SVI related to volume replacement therapy in patients before off-pump coronary artery bypass grafting. The conventional static preload indexes assessed in this study as well as the volumetric preload variable GEDVI and also LVEDAI determined by TEE, however, were not capable of predicting fluid responsiveness.
SVV occurs due to cyclic changes of intrathoracic pressure induced by mechanical ventilation. It has been recognized as an interesting concept for guiding fluid replacement therapy > 20 years ago. (18) The major determinant of this variable is the reduced venous return during mechanical (positive pressure) inspiration. The method per se appears to visualize the individual cardiac response--ie, the changes in SV--related to myocardial contractility due to diastolic volume loading. In the presence of hypovolemia, high SVVs can be observed and the preload dependence of left ventricular function is pronounced, ie, the ventricle operates on the ascending limb of the Frank-Starling curve. During volume expansion, there is a rightward shift of left ventricular function on the Frank-Starling curve, which is thought to correspond to the observed decrease of SVV. SVVs result in concomitant changes of arterial pressure, a well-known clinical phenomenon, which can be assessed by measurement of SPV and PPV.
Both variables have been used to assess fluid responsiveness and have been shown in different investigations (3,7,19) to have sensitivity in predicting the ventricular response to fluid administration. However, PPV was found to be superior to SPV by Michard et al (20) because PPV more reliably reflected changes in transmural pressures and was less influenced by extramural, ie, pleural pressure changes associated with mechanical ventilation. Similarly, Denault et al (21) stated that SPV cannot be explained by changes in left ventricular volume only but may more likely reflect changes in airway and intrathoracic pressures during mechanical ventilation. In addition, both SPV and PPV may be also influenced by vasomotor tone (8); furthermore, clinical use of these variables was limited due to the need for off-line quantification. The current PiCCOplus system now provides PPV on an automated real-time basis.
SVV, however, is a volume- (not pressure-) related variable derived from pulse contour analysis and is provided continuously in real-time by the PiCCOplus system. SVV was advocated to be more accurate than SPV and PPV, (8) and studies in patients during sepsis state (22) or undergoing neurosurgery (4) demonstrated the ability of this method to predict fluid responsiveness. However, inconsistent results investigating SVV in cardiac surgery patients have been obtained: Reuter et al (11) found SVV to be useful in predicting fluid responsiveness postoperatively in patients with preserved as well as with reduced left ventricular function, (12) whereas Wiesenack et al (13) found no correlation between SVV and SV changes during a preoperative fluid trial. These different study results may primarily be based on considerable differences in the study designs, ie, different ventilation strategies as well as fluid management protocols and different patient cardiovascular status. After all, the value of SVV to assess fluid responsiveness has been questioned. (8) Interestingly, data on direct comparison of SVV with other estimates of variation in SV are sparse: in one study, (23) SVV and SPV were closely correlated, and both variables showed a comparable capability to predict fluid responsiveness. SVV and PPV were well correlated in another study (14); however, prediction of fluid responsiveness was not assessed. Our results now confirm the usefulness of both SVV and PPV to predict the individual cardiac response to fluid loading in the clinical setting used.
In clinical practice, distinct information regarding the cardiac response to planned fluid replacement therapy is usually hard to obtain. We found a threshold value of 12.5% for SVV and of 13.5% for PPV to induce an SVI increase [greater than or equal to] 25% with fluid replacement according to the protocol (6% hydroxyethyl starch solution [mean molecular weight, 130,000 d/mean degree of snbstitution, 0.4]; 10 mL/kg ideal body weight over 20 min). Only few data on SVV threshold values can be found in the literature. ROC analyses have revealed a threshold value for SVV of 9.5% to induce a stepwise SVI increase of [greater than or equal to] 5% in studies (4,12) using incremental volume administration. For PPV, a threshold value of 13% to predict a change in cardiac index [greater than or equal to] 15% after a single fluid bolus was described. (19)
In contrast to SVV and PPV, conventional static preload indexes assessed in this study failed to predict fluid responsiveness, confirming the results of previous work on this topic. (3,24) Standard pressure preload variables (CVP and PCWP) did not adequately reflect preload status and therefore are not suitable to predict ventricular response to fluid load. (2,25) Both volumetric variables assessed in this study--GEDVI and LVEDAI--more adequately reflected changes of cardiac preload, in accordance with data of previously published work. (26) However, these two preload indexes also failed to predict the reaction of the heart to fluid loading. This finding may be explained by the fact that fluid responsiveness relies more on the slope of the Frank-Starling curve than on cardiac preload itself.
With respect to practical use of SVV monitoring for guiding fluid therapy in clinical practice, the limitations of this method have to be emphasized. While monitoring SV over time, alterations in ventilatory settings--ie, tidal volumes, level of positive end-expiratory pressure, respiratory rate with concomitantly increasing intrinsic positive end-expiratory pressure, intermittent spontaneous patient breathing--as well as the occurrence of dysrhythmias or alterations of myocardial contractility (including pharmacologic stimulation) may render these SVV estimates unreliable. Thus, mechanical ventilation in fully sedated patients, sinus rhythm, or pacing in a fixed mode and unchanged catecholamine management are prerequisites for proper use of this dynamic monitoring tool. Furthermore, sternotomy as well as other surgical manipulations may further influence SVV readings. Some limitations of this study also have to be addressed. First, SVV and PPV were assessed by the same device and were not compared with another technique, for instance cyclic changes of aortic Doppler flow. (27) Second, we did not assess myocardial contractility. Furthermore, preoperative [beta]-blockade in all patients may be responsible for the observed lack of heart rate response to fluid loading and may have influenced our findings. Although [beta]-blockade is widely used today in patients undergoing coronary artery bypass grafting or other high-risk surgeries, our findings may not directly be applicable to patients other than the population studied. Moreover, during measurements and fluid trial, no manipulations were allowed, ie, table-tilting maneuvers, catheter insertion, or surgical interventions were strictly avoided. These conditions rarely apply to clinical situations, when the decision on fluid replacement therapy has to be taken. In conclusion, SVV and PPV assessed by the PiCCOplus system showed comparably good performance in predicting fluid responsiveness in patients with preserved left ventricular function undergoing off-pump coronary artery bypass grafting.
REFERENCES
(1) Heames RM, Gill RS, Ohri SK, et al. Off-pump coronary artery surgery. Anaesthesia 2002; 57:676-685
(2) Kumar A, Anel R, Bunnell E, et al. Pulmonary artery occlusion pressure and central venous pressure fail to predict ventricular filling volume, cardiac performance, or the response to volume infusion in normal subjects. Crit Care Med 2004; 32:691-699
(3) Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest 2002; 121:2000-2008
(4) Berkenstadt H, Margalit N, Hadani M, et al. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg 2001; 92:984-989
(5) Gunn SR, Pinsky MR. hnplications of arterial pressure variation in patients in the intensive care unit. Curr Opin Crit Care 2001; 7:212-217
(6) Michard F, Teboul JL. Using heart-lung interactions to assess fluid responsiveness during mechanical ventilation. Grit Care 2000; 4:282-289
(7) Perel A. Assessing fluid responsiveness by the systolic pressure variation in mechanically ventilated patients: systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 1998; 89:1309-1310
(8) Pinsky MR. Probing the limits of arterial pulse contour analysis to predict preload responsiveness. Anesth Analg 2003; 96:1245-1247
(9) Godje O, Hoke K, Goetz AE, et al. Reliability of a new algorithm for continuous cardiac output determination by pulse-contour analysis during hemodynamic instability. Crit Care Med 2002; 30:52-58
(10) Goedje O, Hoeke K, Lichtwarck-Aschoff M, et al. Continuous cardiac output by femoral arterial thermodilution calibrated pulse contour analysis: comparison with pulmonary arterial thermodilution. Crit Care Med 1999; 27:2407-2412
(11) Reuter DA, Felbinger TW, Schmidt C, et al. Stroke volume variations for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intensive Care Med 2002; 28:392-398
(12) Reuter DA, Kirchner A, Felbinger TW, et al. Usefulness of left ventricular stroke volume variation to assess fluid responsiveness in patients with reduced cardiac function. Crit Care Med 2003; 31:1399-1404
(13) Wiesenack C, Prasser C, Rodig G, et al. Stroke volume variation as an indicator of fluid responsiveness using pulse contour analysis in mechanically ventilated patients. Anesth Analg 2003; 96:1254-1257
(14) Reuter DA, Goresch T, Goepfert MS, et al. Effects of mid-line thoracotomy on the interaction between mechanical ventilation and cardiac filling during cardiac surgery. Br J Anaesth 2004; 92:808-813
(15) Felbinger TW, Reuter DA, Eltzschig HK, et al. Comparison of pulmonary arterial thermodilution and arterial pulse contour analysis: evaluation of a new algorithm. J Clin Anesth 2002; 14:296-301
(16) Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 1989; 5:303-311
(17) Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983; 148:839-843
(18) Jardin F, Farcot JC, Gueret P, et al. Cyclic changes in arterial pulse during respiratory support. Circulation 1983; 68:266-274
(19) Preisman S, DiSegni E, Vered Z, et al. Left ventricular preload and function during graded haemorrhage and retranfusion in pigs: analysis of arterial pressure waveform and correlation with echocardiography. Br J Anaesth 2002; 88: 716-718
(20) Michard F, Boussat S, Thelma D, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 2000; 162:134-138
(21) Denault AY, Gasior TA, Goresan J III, et al. Determinants of aortic pressure variation during positive-pressure ventilation in man. Chest 1999; 116:176-186
(22) Marx G, Cope T, McCrossan L, et al. Assessing fluid responsiveness by stroke volume variation in mechanically ventilated patients with severe sepsis. Eur J Anaesthesiol 2004; 21:132-138
(23) Reuter DA, Felbinger TW, Kilger E, et al. Optimizing fluid therapy in mechanically ventilated patients after cardiac surgery by on-line monitoring of left ventricular stroke volume variations: comparison with aortic systolic pressure variations. Br J Anaesth 2002; 88:124-126
(24) Bendjelid K, Romand JA. Fluid responsiveness in mechanically ventilated patients: a review of indices used in intensive care. Intensive Care Med 2003; 29:352-360
(25) Hansen RM, Viquerat CE, Matthay MA, et al. Poor correlation between pulmonary arterial wedge pressure and left ventricular end-diastolic volume after coronary artery bypass graft surgery. Anesthesiology 1986; 64:764-770
(26) Buhre W, Buhre K, Kazmaier S, et al. Assessment of cardiac preload by indicator dilution and transoesophageal echocardiography. Eur J Anaesthesiol 2001; 18:662-667
(27) Feissel M, Michard F, Mangin I, et al. Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 2001; 119:867-873
Manuscript received November 8, 2004; revision accepted February 15, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal.org/misc/reprints.shtml).
Correspondence to: Christoph K. Hofer, MD, Institute of Anesthesiology and Intensive Care Medicine, Triemli City Hospital Birmensdorferstr. 497, CH-8063 Zurich, Switzerland; e-mail: christoph.hofer@triemli.stzh.ch
* From the Institute of Anesthesiology and Intensive Care Medicine (Drs. Hofer, Muller, Furrer, and Zollinger), Triemli City Hospital, Zurich, Switzerland; and Departments of Psychosocial Medicine (Dr. Klaghofer) and Cardiac Surgery (Dr. Genoni), University Hospital Zurich, Zurich, Switzerland.
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group