Appreciating that CO2 modifies the chemical reactivity of nitric oxide (NO)-derived inflammatory oxidants, we investigated whether hypercapnia would modulate pulmonary inflammatory responses. Rabbits (n = 72) were ventilated with approximately 7-ml/kg tidal volume for 6 hours. Animals were randomized to one of the following conditions: eucapnia (Pa^sub CO^sub 2^^ at approximately 35-40 mm Hg), eucapnia + lipopolysaccharide (LPS), eucapnia + LPS + inhaled NO (iNO delivered at approximately 20 ppm), hypercapnia (Pa^sub CO^sub 2^^ at approximately 60 mm Hg), hypercapnia + LPS, and hypercapnia + LPS + iNO. The hypercapnia + LPS groups compared with groups exposed to eucapnia + LPS displayed significantly increased bronchoalveolar lavage fluid protein concentrations (p
Keywords: carbon dioxide; low tidal volume ventilation; lung injury
Protective lung strategies serve to reduce pulmonary morbidity and patient mortality in a critical care setting and include employing reductions in tidal volume and/or plateau pressure, thus reducing end-inspiratory alveolar stress (1). In response, diminished expression of inflammatory mediators in both bronchoalveolar lavage fluid (BALF) and serum has been observed (2, 3). Not infrequently, reductions in minute ventilation brought about by such strategies will induce varying degrees of hypercapnia (4). Blood partial pressure of CO2 has traditionally been employed as a gauge of ventilation. However, in addition to regulating vasomotor tone, which is intimately linked to partial pressures of CO2, this species is now recognized to be chemically reactive and immunomodulatory, especially on accrual (hypercapnia) (5, 6).
We have previously reported that hypercapnic conditions, principally in the presence of reactive inflammatory mediators, stimulates inducible nitric oxide synthase (NOS[2]) gene expression, lung cell protein tyrosine nitration, and lung cell apoptosis. These actions of hypercapnia, in the absence of pH changes, combine to impair epithelial barrier function (6). Augmented production of reactive species, including superoxide (O^sub 2^^sup .^), hydrogen peroxide, hypochlorous acid, NO (^sup .^NO), and peroxynitrite (ONOO^sup -^) occurs during pulmonary inflammatory responses, with these and other mediators proposed to contribute to the induction and maintenance of injury (7, 8). Hypercapnia alone as well as the acidemia linked with its accrual has been associated with the upregulation of NOS(2)-mediated NO-depenclent effects at the vascular, organelle, biochemical, and molecular levels (9-11). Recent reports also reveal the possibility that hypercapnia is associated with impaired pulmonary gas exchange and amplification of lipid peroxidation (12, 13). These observations contrast with recent reports of salutary actions of hypercapnia, specifically hypercapnic acidosis achieved by the inhalation of varied CO2 concentrations (14-18). These latter studies have demonstrated significant reductions in indices of lung injury and inflammation after ischemia-reperfusion, endotoxin exposure, surfactant treatment, and high tidal volumes and inspiratory pressures. Because of these contrasting results, we investigated whether ventilation under hypercapnic circumstances induced by reducing minute ventilation would modify lung inflammatory responses in an intact rabbit model of reduced tidal volume ventilation and lung inflammation induced by the intravenous administration of lipopolysaccharide (LPS). Our results reveal that animals undergoing reduced tidal volume ventilation with concomitant hypercapnia in the presence of LPS compared with normocapnic animals exposed to LPS alone displayed amplified pulmonary inflammatory responses. This response was attenuated by simultaneous administration of inhaled NO (iNO). Interestingly, animals exposed to hypercapnia alone did not exhibit these findings. From these data, it was concluded that hypercapnia amplified oxidative inflammatory injury to the lung.
METHODS
All experimental work conformed to the guidelines of the National Institutes of Health guidelines and was approved by the Institutional Animal Care and Use Committee at the University of Alabama at Birmingham (see also the expanded METHODS section in the online supplement).
Animal Preparation
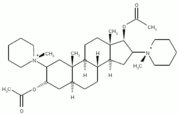
New Zealand white rabbits (Myrtle's Rabbits, Thompson Station, TN) weighing 2.5 to 3.0 kg were used in this study. All were fasted from food for 24 hours previous to use but were allowed free access to water. Rabbits were anesthetized with intravenous ketamine (10 mg/kg), administered via a marginal ear vein. Anesthesia was maintained with ketamine (10 mg/kg/hour), xylazine (3 mg/kg/hour), and intermittent neuromuscular blockade with pancuronium bromide (0.5 mg/kg/hour). Via tracheostomy, a 3.5-mm endotracheal tube was placed. Ventilation was initiated with VT at approximately 7 ml/kg, positive end-expiratory pressure (PEEP) at approximately 2 cm H2O, with a respiratory rate to maintain a Pa^sub CO^sub 2^^ at approximately 40 mm Hg and FI^sub O^sub 2^^ = 1.0 for the initial 30 minutes of each experiment before allocation (model 55-7058; Harvard Inspira asv, Holliston, MA).
Assessment of Physiologic Indices
Stable physiologic conditions were obtained before allocation. Mean arterial pressure (mm Hg), heart rate (beats per minute), and esophageal temperature (°C) were measured throughout the study protocol and recorded at 30-minute intervals.
Lung Injury Protocol
LPS (5-mg/kg Escherichia coli, serotype 055/B5, Catalog No. L2637; Sigma Chemical, St. Louis, MO) was administered through a marginal ear vein over a 20-minute interval to 48 animals. The animals were given Lactated Ringer's solution intravenously by an Omni-Flow 4000 infusion pump at 7.5 ml/kg/hour (Abbott Laboratories, Abbott Park, IL). iNO was administered to 12 animals in each series at a continuous concentration of 20 ppm (Table 1).
Series 1: Eucapnia: Rabbits were allocated to eucapnia (Pa^sub CO^sub 2^^ of approximately 40 mm Hg, n = 36) and ventilated supine with VT of approximately 7 ml/kg, PEEP of approximately 2 cm H2O, and FI^sub O^sub 2^^ = 1.0 for 6 hours.
Series 2: Hypercapnia: Rabbits were allocated to hypercapnia (Pa^sub CO^sub 2^^ of approximately 60 mm Hg, n = 36) and ventilated supine with VT of approximately 7 ml/kg, PEEP of approximately 2 cm H2O, and FI^sub O^sub 2^^ = 1.0 for 6 hours.
Bronchoalveolar Lavage Analysis
At study completion, the animals were exsanguinated, and the heart-lung block was removed. The left lung was lavaged with 6 aliquots of 25 ml (total = 150 ml) 0.9% NaCl with the retrieval ranging between 110 and 130 ml. The BALF was centrifuged, and the resulting cells were washed and resuspended in Hanks' balanced salt solution (19). Cells were counted and distinguished by their characteristic appearances. The BALF was stored at -80°C. In addition, a 1-ml aliquot was used to measure total protein concentration (bicinchoninic acid [BCA]; Pierce, Rockford, IL).
Gravimetric Analysis
The right lung was used for determination of lung wet-to-dry weight ratio. Lung segments were weighed before and after drying (a 2-week drying period) to calculate the wet-to-dry weight ratios. These data were not corrected for residual intrapulmonary blood.
Lung Morphometric Analysis
The unlavaged left upper lobe was isolated, dissected, and placed in formalin for 18 hours before transferring to 70% methanol for an additional 24 hours. The paraffin-embedded lung sections measuring 5 µm were mounted on slides and stained with hematoxylin and eosin. Each section was evaluated by a pathologist blinded to the experimental conditions.
Biochemical Analysis
Nitrite and nitrate assay. Plasma and lung homogenates were transferred to an ultrafiltralion unit and centrifuged for 1 hour to remove protein. Analyses of scrum and lung tissue homogenates were performed in duplicate via the Greiss reaction (20).
Lung Immunohistochemistry
Formalin-fixed, paraffin-embedded lung tissue sections 5 µm in thickness were prepared. Sections were permeabilized using 0.1% Triton-X-100 in phosphate-buffered saline. Primary antibody incubations were performed for 1 hour at 25°C with monoclonal anti-NOS(2) (32 µg/ml; BD Transduction Laboratories, San Diego, CA), monoclonal antinitrotyrosine (1:50 dilution; Cayman, Hornby, ON, Canada) and monoclonal anti-myeloperoxidase (MPO) (1:40 dilution; Research Diagnostics Incorporated, Flanders, NJ) (21). The secondary antibody was either Alexa-594 or Alexa-488 conjugated goat anti-mouse IgG (1:100 dilution; Molecular Probes, Eugene, OR). Nuclei were counterstained with Hoechst 33,258 (20 µg mg^sup -1^). Four random images were selected from four separate animals in each condition. Image acquisition was performed on a Leica DMRXA2 epifluorescence microscope with SimplePCI software (Compix, Inc., Cranberry Township, PA). Images were adjusted appropriately to remove background fluorescence. Pixel intensity was analyzed by measuring the intensity (mean red, mean green) of the region of interest with Image Pro Plus (Media Cybernetics).
Statistical Analysis
Data were analyzed by one-way analysis of variance followed by a post hoc Student Newman-Keuls test. Significance was set at p
RESULTS
Baseline Characteristics
All treatment groups displayed similar 1-hour physiologic characteristics before study initiation. Table 2 summarizes physiologic indices determined during the 6-hour ventilation protocol under the previously described conditions (n = 12 per group studied). Four rabbits died of refractory hypotension within 1 hour of administration of LPS and were not studied further.
Hemodynamic, Gas Exchange, and Acid-Base Data
The mean arterial pressures of all groups at baseline and 6 hours were not significantly different, with mean arterial pressure maintained using Lactated Ringer's solution and vasopressors in animals receiving LPS. Heart rate was greater in animals receiving LPS and was highest in the hypercapnic + LPS group (p
Significant changes in Pa^sub O^sub 2^^ were not observed. Although rabbits not receiving iNO had a lower Pa^sub O^sub 2^^ at 6 hours compared with baseline, this difference was not significant. Animals receiving iNO had modest increases in Pa^sub O^sub 2^^ at 6 hours. The Pa^sub CO^sub 2^^ in the groups exposed to hypercapnic conditions was significantly greater (40 ± 4 mm Hg in eucapnia + LPS groups, 59 ± 7 mm Hg in hypercapnia + LPS groups; p
Blood pH decreased in both the eucapnia and hypercapnia groups receiving LPS, with rabbits exposed to hypercapnia in the presence of LPS displaying a significantly lower pH (7.25 ± 0.3 in eucapnia + LPS groups, 7.17 ± 0.1 in hypercapnia + LPS groups; p
Fluid requirements, both maintenance and bolus, were not observed to be significantly different. There was a trend for groups that received endotoxin to require a net increase in fluids during the study period. Phenylephrine requirements were much greater in all groups receiving endotoxin but were not different between eucapnia, hypercapnia and iNO groups.
Indices of Lung Inflammation
Concentrations of BALF protein, lung wet-to-dry weight ratios, and lung histology scoring were used to reflect extents of inflammatory lung injury. Protein concentration in the BALF was significantly greater in the hypercapnia + LPS group compared with eucapnia + LPS (0.17 ± 0.2 vs. 0.12 ± 0.1 mg/ml protein, p
Important differences were observed after evaluation of lung histology (Figures 3A and 3B). Groups receiving ventilation with hypercapnia displayed extensive polymorphonuclear cell (PMN) and macrophage infiltration. The greatest degree of histologic changes were observed in animals receiving hypercapnia + LPS, where significant alveolar transudation, septal edema, and extravasation of red blood cells occurred. There was mild attenuation of these responses in both groups that received iNO.
PMN infiltration was the greatest in the group receiving hypercapnic ventilation + LPS + iNO, although this was not statistically significant (Table 3). No other significant differences were observed. The alveolar septal surface area of lung tissue sections, an indicator inflammatory proliferation and edema, was greatest after hypercapnia + LPS exposure compared with eucapnia + LPS (5.2 × 10^sup 5^ ± 0 vs. 3.6 × 10^sup 5^ ± 0.67 pixels, p
Pulmonary cells recovered by BALF were most numerous after hypercapnia + LPS exposure when compared with eucapnia + LPS (5.7 × 10^sup 6^ ± 0.8 × 10^sup 6^ vs. 4.3 × 10^sup 6^ ± 0.5 × 10^sup 6^ cells/ml, p
Serum NO^sup -^^sub 2^ + NO^sup -^^sub 3^ concentration increased in all groups over the 6-hour treatment interval, especially the animals receiving LPS. Hypercapnia further increased serum NO^sup -^^sub 2^ and NO^sup -^^sub 3^ concentrations in all groups receiving LPS (Figure 5). The increase in serum NO^sup -^^sub 2^ and NO^sup -^^sub 3^ levels in exposure groups became significant at 3-6 hours after LPS administration (p
Immunohistochemical Analysis
Expression of NOS(2) was enhanced in lungs of animals exposed to LPS (Figure 7). However, image analysis of NOS(2) fluorescence intensity revealed LPS-exposed animals ventilated under hypercapnic conditions displayed even greater extents of NOS(2) expression compared with ventilation under eucapnic conditions (19 ± 4.5 vs. 11.7 ± 3.0, p
Exposure to hypercapnic conditions increased protein 3-nitrotyrosine (3-NT) content (Figure 8), an event that image analysis fluorescence intensity showed was only significantly increased in the hypercapnia + LPS group compared with the eucapnia + LPS group (24 ± 4.6 vs. 14.7 ± 2.8, p
Neutrophil-derived MPO, a heme peroxidase catalyst of 3-NT formation (21) and a general index of inflammatory cell influx, was present to the greatest extent under hypercapnic conditions (Figure 9). Pulmonary tissue MPO content increased to the greatest extent when LPS was co-administered to animals ventilated under hypercapnia-inducing conditions (19.2 ± 4.3, p
DISCUSSION
This investigation indicates that ventilation employing a strategy of reduced VT ventilation and respiratory rate with reduced PEEP and 100% oxygen results in an expected concomitant hypercapnia. These conditions amplify LPS-induced pulmonary inflammatory injury, as indicated by increased BALF protein concentration, lung wet-to-dry weight ratio, increased BALF neutrophil count, biochemical indices of oxidative inflammatory reactions, and lung histologic changes. A mitigating role for NO-dependent mechanisms in lung inflammatory responses to hypercapnia + LPS is reinforced by the observation in chemical reaction systems that CO2 reacts with NO-derived species to yield products that redirect and amplify inflammatory oxidation and nitration reactions. This view was experimentally supported herein by the observation of CO2-dependent increases in bronchoalveolar NOS(2) expression, lung tissue protein tyrosine nitration, and elevated lung neutrophil-derived MPO content in the presence of LPS. Hypercapnia alone did not amplify lung injury, and the inhalation of iNO attenuated selected indices of lung injury.
The Experimental Model
This investigation was performed in intact rabbits and thus cannot be directly applied to the clinical setting. With that stated, however, this model does mimic most of the conditions encountered when ventilating a patient with lung injury in the critical care setting (i.e., systemic inflammation, reduced VT, elevated FI^sub O^sub 2^^, hemodynamic instability, the use of iNO, and of present relevance, hypercapnia).
There are limitations of this model that prevent direct extrapolation to the bedside. Acute pulmonary inflammation was induced by intravenous administration of LPS and thus did not specifically reflect the more complex and sometimes more chronic inflammatory milieu of severe sepsis and septic shock that would normally be encountered clinically. Additionally, the duration of experiments was only 6 hours, which may have been insufficient time for eucapnic groups to fully express the degree of ultimate injury. In this regard, we are presently extending current observations to an intensive care unit-like experimental model that will use less acute inflammatory stimuli and permit for 24- to 48-hour ventilation intervals, thus more closely mimicking clinical scenarios.
VT of approximately 7 ml/kg were used herein to incorporate the most recent clinical recommendations and lend additional credibility to the model. However, the PEEP used in this study was lower than traditionally clinically recommended but was consistent with that used by others assessing the role of hypercapnia in animal models (0-3 cm H2O) (14, 17, 18).
The use of an elevated FI^sub O^sub 2^^ is commonly required in patients suffering from acute lung injury/acute respiratory distress syndrome (ARDS). Hyperoxia is independently associated with increases in lung injury. The mechanisms involved are numerous and diverse and generally involve the enhanced production of oxygen radicals from lung parenchymal cells and activated macrophages (22-24). Thus, using a FI^sub O^sub 2^^ of 1.0 almost certainly enhanced production rates of reactive oxygen species and consequently was additive in enhanced lung injury. However, all groups were exposed to the same FI^sub O^sub 2^^; thus, any observed difference in injury would be attributable to other conditions such as LPS, hypercapnia, and/or iNO.
The use of "moderate" CO2 tension as an exemplary hypercapnic condition herein was intentional to better mimic clinical practice. Although previous animal studies used much higher CO2 tensions (range of 70-110 mm Hg) (13-18), the most recent prospective clinical study assessing the effects of permissive hypercapnia reported a mean tension of 67 mm of Hg and pH of 7.23 (12). The CO2 ranges previously cited are rarely feasible clinically because of concomitant metabolic acidosis and a potential for compromising other concomitant clinical problems, such as head injury. Additionally, clinically, if CO2 tensions venture into the range of 80-100 mm Hg in critically patients, the use of alkali therapy is generally mandatory.
iNO is used a pharmacologic adjunct in patients with lung injury, especially in the pediatric patient population where pulmonary hypertension is severe and a significant factor in potentiating permeability pulmonary edema and right heart failure (25-27). Thus, because of a high use rate and unappreciated potential for detrimental biochemical consequences in the setting of hypercapnic environments, we viewed the analysis of iNO as a legitimate limb in this study. The use of iNO in patients with ARDS is linked with increased lung tissue protein 3-NT content (28). As to be discussed, a hypercapnic environment could thus enhance lung inflammatory nitration reactions. Additionally, the effect of exogenous administration of iNO on endogenous NO production has been controversial (29, 30). This study revealed the suppression of NOS(2) protein expression during exogenous iNO administration with similar extents of 3-NT formation. The concomitant study of tissue responses to NOS inhibitors, such as L-N-monomethyl-L-arginine (L-NMMA), was not considered because of their clinical impracticality and a desire to focus on the most common clinical approaches used in a critical care setting.
The Rationale for Hypercapnia
First, the genesis of lung dysfunction in acute lung injury/ARDS is multifactorial but once established involves the complex interplay of pro-inflammatory and anti-inflammatory mediators (31). second, mechanical ventilation (pulmonary mechanical stress) can both induce or amplify lung injury (ventilator-associated lung injury) because of the myriad of interactions between the mechanical ventilator, inspired oxidizing gases, inflammatory mediators, and the lung (3, 32-34). Hence, one potentially protective clinical strategy for the management of acute lung injury/ARDS is permissive hypcrcapnia, wherein tissue and plasma CO2 tensions are allowed to increase as a result of reductions in VE (35, 36). The rationale underlying the use of permissive hypercapnia is to allow for reductions in lung mechanical stress at a time when alveolar-capillary integrity is vulnerable and at risk for permeability pulmonary edema to accrue. The respiratory acidosis ensuing from hypercapnia via reduced VE has been viewed to be "well tolerated" by most patients, suggesting that the limitation of repetitive ventilatory cycles during the time of alveolar vulnerability could be advantageous in protecting the previously injured lung (i.e., during sepsis) from secondary injury (i.e., ventilator-associated lung injury) (4, 37). Although recent clinical trials using varying degrees of CO2 have yielded encouraging results, including improved survival in patients suffering from acute lung injury/ARDS, CO2 accrual from reduced VE has not been a focus in these studies (38, 39).
Potential Contributions of Carbon Dioxide to Lung Oxidative Inflammatory Responses
Carbon dioxide has a potential to exert either deleterious or protective effects during pulmonary inflammatory responses because of an ability to influence acid-base physiology and a potent reactivity with oxidative inflammatory mediators.
NO, an endogenously produced free radical species, is characteristically enhanced in concentration during pulmonary inflammation via NOS(2) induction by multiple pulmonary cell types (40). A reaction of particular significance during inflammatory responses occurs between NO and O2^sup -^, yielding the potent oxidizing and nitrating product ONOO^sup -^ and its conjugate acid peroxynitrous acid (41-43). The half-life and reaction pathways of ONOO^sup -^ are profoundly influenced, both kinetically and mechanistically, by CO2 (5). Of relevance, CO2 has been previously viewed to be metabolically inert beyond acid-base chemistry. However, CO^sub 2^/HCO^sub 3^^sup -^ has historically been appreciated to yield oxidizing free radical products when exposed to high energy irradiation. More recently, in vitro studies show that CO2-dependent formation of nitrosoperoxocarbonate (ONOOCO^sub 2^^sup -^) and its secondary products serve to increase O2^sup -^, NO and ONOO^sup -^-mediated oxidative, free radical and nitration reactions, as well as cell injury (41, 44, 45).
Depending on the local milieu of NO-derived reactive inflammatory mediators and the CO2 concentration in pulmonary tissue microenvironments, the reaction of ONOO with CO2 has a potential to be "protective" by virtue of facilitating the formation of an inflammatory oxidant with a 103-fold shorter half-life (ONOOCO^sub 2^). Alternatively, the altered oxidative and nitrating capacity of ONOOCO^sub 2^^sup -^ could lead to amplification of inflammatory injury during hypercapnia. The data reported herein support the occurrence of this latter outcome. ONOO^sup -^, when produced in the presence of the physiologically ubiquitous CO2, yields a nitrosoperoxocarbonate intermediate, ONOOCO^sub 2^^sup -^, with this reaction viewed to represent a major pathway for tissue ONOO^sup -^ reactivity (44, 45). Chemically oriented studies reveal that CO2-dependent formation of ONOOCO^sub 2^^sup -^ and its secondary products can increase for O2^sup -^, NO, and ONOO^sup -^-mediated oxidative, free radical, and nitration reactions, hence cell injury (41, 44, 45). Appreciating that the half-life of the ONOOCO^sub 2^ intermediate (approximately 1 millisecond) is approximately 10^sup 3^ shorter than for ONOO^sup -^ (approximately 1 second) (46), a balance between enhanced oxidizing and nitrating reactivity and a shorter tissue half-life must be considered when predicting the role of CO2 in oxidative inflammatory injury. This latter consideration motivated the design of this clinically and physiologically relevant study.
The nitration of pulmonary cell protein tyrosine residues are increased in respiratory distress syndromes and represents a molecular footprint of enhanced rates of production of NO-derived inflammatory oxidants. This reaction was shown to be accelerated by hypercapnia in an in vitro model of lung injury (6). An emerging issue of significance thus becomes the pathophysiologic consequence(s) of 3-NT production. For example, increased concentrations of tissue protein 3-NT derivatives in BALF proteins have been associated with patients "at risk" for ARDS and in patients with ARDS who have succumbed from this disease (47). However, nitration of tyrosine in clinical BALF samples generally represents a very small fraction of total protein tyrosines. Thus, the issue remains as to whether oxidative and nitrative lung injury is a consequence of 3-NT-mediated alterations in protein structure and function or is merely a functionally "inert" index of oxidative and nitrosative reactions. Recently, pathogenic tissue responses have been linked to renal and hepatic 3-NT formation in humans and mice suffering from sickle cell disease, where 3 of the 15 tyrosine residues of cytoskeletal actin were specifically nitrated by inflammatory oxidant-mediated reactions (48). In response to this post-translational protein modification, impaired actin filament formation occurred that morphologically correlated with renal and hepatocellular injury and apoptosis. Our intact model of LPS-induced lung injury was an abundant source of reactive species supporting the formation of ONOO^sup -^ and following reaction with CO2, ONOOCO^sub 2^^sup -^. Interestingly, expression of NOS(2) was greatest in the group receiving hypercapnic ventilation in the presence of LPS. iNO diminished NOS(2) expression in the hypercapnic + LPS group and limited the extent of lung edema formation and lung inflammation in some cases. Similar to the feedback regulation of other cell signaling mediators, NO exerts a negative regulatory effect on both NOS(2) expression and catalytic activity (29, 49, 50). In this study, the extent of 3-NT formation was increased in lungs of rabbits administered iNO, consistent with previous observations (51, 52).
Total cell counts and PMN counts (%) were elevated under of conditions of hypercapnia + LPS in the BAL fluid. Although cell counts decreased in the hypercapnia + LPS group receiving iNO, neutrophil counts remained elevated compared with eucapnic + LPS groups receiving iNO (10.5% vs. 5%, respectively). The finding of increased PMN counts in BAL fluid in rabbits subjected to hypercapnia is not exclusively ours. Billert and colleagues recently reported their finding of significantly increased BAL neutrophil counts in Chinchilla rabbits subjected to 4 hours of hypercapnia when compared with animals exposed to the eucapnia for the same duration (5.2 ± 2.1% vs. 1.6 ± 0.7%, respectively) (53). These animals did not receive LPS and/or iNO. Of interest, chemiluminescence activity used as a marker of reactive oxidative intermediates was not increased in animals ventilated under hypercapnic conditions.
The increased content of MPO in lungs of animals exposed to hypercapnia + LPS reinforced that this condition may represent both a response and amplification of pulmonary oxidative inflammatory injury. MPO is a neutrophil hemcprotein secreted after PMN activation that is capable of both binding to and transcytosing vascular and pulmonary cells (54, 55). MPO readily catalyzes formation of oxidizing, nitrating, and chlorinating species that are both bactericidal and have the capacity to induce pulmonary target molecule modifications. In addition, MPO is a significant catalyst for vascular and pulmonary cell protein tyrosine nitration (21). Immunohistochemical analyses reported in Figures 8 and 9 support that hypercapnia + LPS significantly enhanced airway epithelial 3-NT and alveolar MPO content, affirming that these experimental conditions enhance both oxidative inflammatory reactions. The administration of iNO attenuated extents of detectable MPO in the hypercapnia + LPS group, possibly secondary to endogenous downregulation of NOS(2) and/or from direct attenuation of PMN responses.
The Ambiguous Action of Induced Hypercapnia
Hypercapnia via reduced VE. The influence of endogenous hypercapnia produced by a reduction in VE on the generation of secondary reactive inflammatory mediators and parameters of systemic inflammatory signaling has not been studied in an a priori fashion in preclinical or clinical studies. Recently, improved survival was reported in patients with ARDS when strategies using low VT (6-7 ml/kg) were compared with conventional VT (10-12 ml/kg) (1,38). Although arterial tensions of CO2 differed significantly between these two studies (43 vs. 58.2 mm Hg), a comparison with respect to this variable is difficult because of the disparity of VT between groups (higher VT aggravating lung injury via volutrauma) and no evaluation of the impact of hypercapnia on indices of lung inflammation. In the only other study of a similar design, BALF and serum cytokine concentrations were significantly decreased in patients with ARDS ventilated with reduced VT (3). Tensions of CO2 were 37.4 mm Hg in the conventionally ventilated group and 46.9 mm Hg in the patients receiving the protective lung strategy. However, both reductions in VT and increases in PEEP were used in the protective lung strategy group; thus, no causal relationships could be established. In rabbits exposed to an "open lung" protective strategy, resulting in a Pa^sub CO^sub 2^^ of approximately 70-75 torr, lung tissue malondialdehyde, a marker of lipid oxidation, was significantly increased, suggesting increased tissue inflammatory oxidant production, whereas other markers of inflammation were decreased (13). Finally, increased intrapulmonary shunt secondary to elevated cardiac output and decreased alveolar ventilation was observed after initiating permissive hypercapnia in eight patients suffering from ARDS (12). Potential hypercapnia-induced oxidant generation and alterations in cell signaling pathways were not evaluated.
Hypercapnia via inhaled CO2. The technique of "therapeutic hypercapnia," for example, administering varying inspired fractions of carbon dioxide, has been observed to be antiinflammatory to the lung. In models of pulmonary and mesenteric ischemia-reperfusion, ventilator-induced lung injury and the surfactant treatment of animals with lung disease of prematurity, administration of inhaled CO2 in varying concentrations to attain preset partial pressures of CO2 attenuated lung injury compared with eucapnic cohorts (14-17). In fact, buffering the respiratory acidosis caused by inhaled CO2 abrogated the protective effect of the high P^sub CO^sub 2^^ (15). In addition to an increase in lung wet-to-dry weight ratios, uric acid, used as a footprint of xanthine oxidasc activity, was also significantly increased when buffered sodium hydroxide was used to increase pH. This point seemingly proved that the lowered pH caused by hypercapnia (indirect acidemia), rather than CO2, acted as the antiinfiammatory stimulus. In contrast, investigations in pulmonary epithelial cells in vitro revealed that when pH was maintained at 7.35-7.40 confirmed with intracellular fluorescence probes and in the presence of physiologically relevant partial pressures of hypercapnia, total lung cell NO production, nitration, and apoptosis were all significantly increased after 24- and 48-hour exposures. Additionally, epithelial barrier function was impaired under these conditions (6).
Most recently, Laffey and colleagues concluded that hypercapnic acidosis induced prophylactically and therapeutically in a rat model of acute endotoxin-induced lung injury attenuated injury (14). In this study in which partial pressures of CO2 were approximately 73 ± 2.7 mm Hg, therapeutic hypercapnia (FI^sub CO^sub 2^^ = 0.05) retained more favorable oxygenation indices, resulted in reduced histologic lung injury, and NO-derived metabolites. Formation of lung cell protein 3-NT derivatives was greatest in the hypercapnic groups, suggesting that in this study the advantageous effect of therapeutic hypercapnia was not via inhibition of NO-dependent nitration reactions. Our findings are the same but then become opposing, as we have found the greatest degree of protein 3-NT derivatives is formed under hypercapnic conditions in the presence of LPS and iNO, conditions also when lung injury is greatest. The study design of Laffey and colleagues differed from the present in both species used (rat versus rabbit), route of LPS administration (intratracheal versus intravenous), and finally, in that CO2 was delivered via an inhaled route versus allowing for endogenous accrual, thus possibly resulting in differences in outcome.
Acidic conditions induce disparate effects on NO and the formation of NO-derived metabolites, with disparate injurious versus protective responses persisting in various models as well. Specifically, acidemia induced by hydrochloric acid infusion has been shown to increase tissue NO generation, presumably via increased NOS(2) expression (9, 56). Acidemia also activates nuclear factor-κB, resulting in upregulation of NOS(2) activity, a mechanism that upregulates expression of proinflammatory molecules such as tumor necrosis factor-α and cell adhesion molecules (10). Other potentially injurious influences of acidemia include increased CD18-mediated neutrophil adhesion, although paradoxically intracellular adhesion molecule (ICAM-1) expression was significantly decreased (11). In contrast, exposure of LPS-stimulated rabbit macrophages to decreasing pH concentrations attenuates tumor necrosis factor-α production (57). More recently, exposure of isolated neutrophils to 10% CO2 environments significantly decreased interleukin-8 production and intracellular oxidant generation (58). Treatment of neutrophils with carbonic anhydrase abrogated the acidemic effect (decreased intracellular pH) of hypercapnia, suggesting that the attenuation of inflammation was not a direct effect of CO2. Favorable effects resulting from acidemia also comprise augmentation of cellular antiapoptic pathways (Gas6/Axl) and inhibition of nuclear factor-κB expression by means of suppressed inhibitory protein-κB resulting in downregulation of ICAM-1 and interleukin-8 (59, 60). In summary, biochemical and cellular model systems suggest that CO2 has the capacity to exert either proinflammatory or antiinflammatory actions, thus motivating the present animal model-based investigation.
Possible Explanations For Our Findings
The model employed herein gave opportunity for clinically relevant extents of intracellular and extracellular production of reactive inflammatory mediators in a setting in which different clinically relevant concentrations of CO2 could be maintained. In aggregate, our data supported a capacity for CO2 to amplify lung injury induced by LPS-induced inflammatory oxidants and/or indirect acidemia induced by hypercapnia. Although partial pressures of arterial CO2 were significantly greater in the hypercapnic groups, similar extents of acidemia were also observed in eucapnic groups receiving LPS. The pH of all exposure groups was not significantly different; pH changes induced by hypercapnia did not appear to account for differences in outcome observed between hypercapnic and eucapnic exposure groups. With this said, scenarios may still exist for indirect acidemia to have some influence on outcome. The potential increase in pulmonary vascular resistance (unmeasured in this study) may partially contribute to increased lung wet-to-dry ratios observed in the hypercapnia + LPS group. Additionally, the accompanying endothelial mechanical stimulation associated with increased hydrostatic forces (both increased pressure and flow) could have also upregulated neutrophil adhesive and aggregatory responses, leading to increased PMN and MPO levels in LPS-stimulated hypercapnic animals. Finally, these observations may differ from others, with respect to the concept of "therapeutic hypercapnia," in the following regards: reducing VE as herein may result in more regional heterogeneous acidosis, with that acidosis and injury occurring in areas that are poorly ventilated. Moreover, delivery of CO2 to the lung is probably not heterogeneous because of pulmonary microvascular flow being predominantly in areas of low V/Q and shunt, particularly in animals with LPS. Inhaled CO2 will probably result in higher net lung CO2 concentrations because of the mechanism of delivery, which will direct CO2 to areas of moderate to high V/Q areas. Additionally, because of the low PEEP used in our study (2 cm H2O), the potential for causing recruitment-derecruitment injury exists as well, thus providing additional inflammatory insult. For example, inadequate recruitment strategies lead to microvascular injury, decreased oxygen tensions, and increased pulmonary vascular resistance (PVR), all variables that could intensify lung injury (61). In summary, we have observed that LPS-induced oxidative inflammatory injury to lung, as manifested by both physiologic and biochemical indices, is enhanced by clinically relevant reduced respiratory rate and Vr-induced strategies that result from tissue hypercapnia.
Conclusions
These animal model-based observations reinforce recently established biochemical precepts regarding facile oxidative reactions of CO2 by revealing that permissive hypercapnia in the presence of LPS amplifies lung injury and the pulmonary production of oxidizing and nitrating species. This CO2-dependent alteration in pulmonary inflammatory responses occurred only in the presence of LPS, suggesting a requirement for an existing prooxidative milieu. The detailed mechanisms underlying these findings remain elusive and are likely multiple, including pro-oxidative reactions of CO2, effects of acidemia associated with CO2 accrual, increased PVR, and stimulation of endothelial-neutrophil responses. These results also lend support to the use of iNO as an anti-inflammatory adjunctive therapy under conditions of systemic inflammation and concomitant hypercapnia.
Conflict of Interest Statement: J.D.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; K.D.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.A. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; Y.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; P.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; B.A.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
1. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-1308.
2. Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS. Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest 1997;99:944-952.
3. Ranieri VM, Suter PM, Tortorella C, De Tullio R, Dayer J M, Brienxa A, Bruno F, Slutsky AS. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress. JAMA 1999;282:54-61.
4. Hickling KG, Walsh J, Henderson S, Jackson R. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med 1994;22:1568-1578.
5. Denicola A, Freeman B, Trujillo M, Radi R. Peroxynitrite reaction with carbon dioxide/bicarbonate: kinetics and influence on peroxynitrite-mediated oxidations. Arch Biochem Biophys 1996;333:49-58.
6. Lang JD Jr, Chumley P. Eiserich J P, Estevez A. Bamberg T, Adhami A, Crow J, Freeman BA. Hypercapnia induces injury to alveolar epithelial cells via a nitric oxide-dependent pathway. Am J Physiol Lung Cell Mol Physiol 2000;279:994-1002.
7. Baldwin SR, Gram CM, Boxer LA, Simon RH, Ketai L, Devall LJ. Oxidant activity in expired breath of patients with adult respiratory distress syndrome. Lancet 1986;1:11-14.
8. Mathru M, Rooney MR, Dries DJ, Hirsch LJ, Barnes L, Tobin MJ. Urine hydrogen peroxide during adult respiratory distress syndrome in patients with and without sepsis. Chest 1994;105:232-236.
9. Pedoto M, Caruso JE, Nandi J, Oler A, Hoffman SP, Tassiopoulos AK, McGraw DJ, Camporesi EM, Hakim TS. Acidosis stimulates nitric oxide production and lung damage in rats. Am J Respir Crit Care Med 1999;159:397-402.
10. Bellocq A, Suberville S, Philippe C, Bertrand F, Perez J, Fouqueray B, Cherqui G, Baud L. Low environmental pH is responsible for the induction of nitric-oxide synthase in macrophages. J Biol Chem 1998;273:5086-5092.
11. Serrano CV Jr, Fraticelli A, Paniccia R, Teti A, Noble B, Corda S, Faraggiana T, Ziegelstein RC, Zweier JL, Capogrossi MC. pH dependence of neutrophil-endothelial cell adhesion and adhesion molecule expression. Am J Physiol 1996;271:C962-C970.
12. Feihl F, Eckert P, Brimioulle S, Jacobs O, Schaller M-D, Melot C, Naeue R. Permissive hypercapnia impairs pulmonary gas exchange in the acute respiratory distress syndrome. Am J Respir Crit Care Med 2000;162:209-215.
13. Rotta AT, Gunnarsson B, Furhman BP, Hernan LJ, Steinhorn DM. Comparison of lung protective ventilation strategics in a rabbit model of acute lung injury. Crit Care Med 2001;29:2176-2184.
14. Laffey JO, Honan D, Hopkins N, Hyvelin J-M, Boylan JF, McLoughlin P. Hypercapnic acidosis attenuates endotoxin-induced acute lung injury. Am J Respir Crit Care Med 2004;169:46-56.
15. Laffey JG, Tanaka M, Engelberts D, Luo X, Yuan S, Tanswell AK, Post M, Lindsay T, Kavanagh BP. Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung rcpcrfusion. Am J Respir Crit Care Med 2000;162:2287-2294.
16. Strand MA, Ikegami M, Jobe AH. Effects of high PCO^sub 2^, on ventilated prcterm lamb lungs. Pediatr Res 2003;53:468-472.
17. Sinclair SE, Kregenow DA, Lamm WJE, Starr IR, Chi EY, Hlaslala MP. Hypercapnic acidosis is protective in an in vivo model of ventilator-induced lung injury. Am J Respir Crit Care Med 2002;166:403-408.
18. Broccard AF, Hotchkiss JR, Vannay C, Markert M, Sauty A, Feihl F, Schaller M-D. Protective effects of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 2001;164:802-806.
19. Matute-Bello G, Frevert CW, Kajikawa O, Skerrett SJ, Goodman RB, Park DR, Martin TR. Septic shock and acute lung injury in rabbits with peritonitis: failure of the neutrophil response to localized infection. Am J Respir Crit Care Med 2001;163:234-243.
20. Giovannoni G, Land JM, Keir G, Thompson EJ, Heales SJ. Adaptation of the nitrate reductase and Griess reaction methods for the measurement of scrum nitrate plus nitrite levels. Am Clin Biochem 1997;34:193-198.
21. Baldus S, Eiscrich JP, Mani A, Castro L, Figueroa M, Chumley P, Ma W, Tousson A, White RC, Bullard DC, Brennan M-L, Lusis AJ, Moore KP, Freeman BA. Endothelial transcytosis of myeloperoxidase confers specificity to vascular ECM proteins as targets of tyrosine nitration. J Clin Invest 2001;108:1759-1770.
22. Rozycki HJ, Comber PG, Huff TF. Cytokines and oxygen radicals after hyperoxia and term alveolar macrophages. Am J Physiol Lung Cell Moll Physiol 2002;282:L1222-L1228.
23. Jankov RP, Johnstone L, Luo X, Robinson BH, Tanswell AK. Macrophages as a major source of oxygen radicals in the hyperoxic newborn rat lung. Free Radic Biol Med 2003;35:200-209.
24. Lee PJ, Choi AMK. Pathways of cell signaling in hypcroxia. Free Radic Biol Med 2003;35:341-350.
25. Fioretto JR, De Moraes MA, Bonatto RC, Ricchetti SM, Carpi MF. Acute and sustained effects of early administration of inhaled nitric oxide to children with acute respiratory distress syndromes. Pediatr CnV Care Med 2004;5:469-474.
26. Finer NN, Barrington KJ. Nitric oxide for respiratory failure in infants born at or near term. The Cochrane Database of Systemic Reviews 2001; Issue 4.
27. Clark RH, Kueser TJ, Walker MW, Southgate WM, Huckaby JL, Perez JA, Roy BJ, Keszler M, Kinsella JP. Low-dose nitric oxide therapy for persistent pulmonary hypertension of the newborn. N Engl J Med 2000;342:469-474.
28. Lamb NJ, Quinlan GJ, Westerman ST, Gutteridge MD, Evans TW. Nitration of proteins in bronchoalveolar lavage fluid from patients with acute respiratory distress syndrome receiving inhaled nitric oxide. Am J Respir Crit Care Med 1999;160:1031-1034.
29. Koh Y, Kang JL, Park W, Pack IS, Lee HS, Kim MJ, Lim C-M. Inhaled nitric oxide down-regulates intrapulmonary nitric oxide production in lipopolysaccharide-induced acute lung injury. Crit Care Med 2001;29:1169-1174.
30. Honda K, Kohayashi H, Hataishi R, Hirano S, Fukuyama N, Nakazawa H, Tomita T. Inhaled nitric oxide reduces tyrosinc nitration after lipopolysaccharide instillation into lungs of rats. Am J Respir Crit Care Med 1999;160:678-688.
31. Fulkerson WJ, MacIntyre N, Stamler J, Crapo JD. Pathogenesis and treatment of the adult respiratory distress syndrome. Arch Intern Med 1996;156:29-38.
32. Chollet-Martin S, Jourdain B, Gibert C, Elhim C, Chastre J, Gougerot-Pocidalo MA. Interactions between neutrophils and cytokines in blood and alveolar spaces during ARDS. Am J Respir Crit Care Med 1996;154:594-601.
33. Von Belhmann AN, Brasch F, Nusing R, Vogt K, Volk HD, Muller KM, Wendel A, Uhlig S. Hyperventilation induces release of cytokines from perfused mouse lung. Am J Respir Crit Care Med 1998;157:263-272.
34. Chiumello D, Pristine G, Slutsky A. Mechanical ventilation affects local and systemic cylokines in an animal model of acute respiratory distress syndrome. Am J Respir Crit Care Med 1999;160:109-116.
35. Bidani A, Tzouanakis AE, Cardenas VJ, Zwischenbcrgcr JB. Permissive hypercapnia in acute respiratory failure. JAMA 1994;272:957-962.
36. Tuxen DV. Permissive hypercapnic ventilation. Am J Respir Crit Care Med 1994;150:870-874.
37. Hickling KG, Joyce C. Permissive hypercapnia in ARDS and its effects on tissue oxygenation. Acta Anaesthesiol Scand Suppl 1995;107:201-208.
38. Amato MBP, Barbas CSV, Medeiros DM, Magaldi RB, Schettino GPP, Lorcnzo-Filho G, Kairalla RA, Dcheinzelin D, Munoz, C, Oliveira R, et al. Effect of a protective ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998;338:347-354.
39. Ullrich R, Lorber C, Roder G, Urak G, Faryniak B, Sladen RN, Germann P. Controlled airway pressure therapy, nitric oxide inhalation, prone position, and extracorporeal membrane oxygenation (ECMO) as compounds of an integrated approach to ARDS. Aneslhesiology 1999;91:1577-1586.
40. Rubbo H, Darley-Usmar V, Freeman B. Nitric oxide regulation of tissue free radical injury. Chem Res Toxicol 1996;9:809-820.
41. Gutierrez HH, Pitt BR, Schwarz M, Watkins SC, Lowenstein C, Caniggia I, Chumley P, Freeman B. Pulmonary alveolar epithelial inducible NO synthase gene expression: regulation by inflammatory mediators. Am J Physiol 1995;268:L501-L508.
42. Squadrito GL, Pryor W. Oxidative chemistry of nitric oxide: the roles of Superoxide, peroxynitrite, and carbon dioxide. Free Radie RM Med 1998;25:392-403.
43. Beckman JS, Beckman TW, Chen J, Marshall PA, Freeman BA. Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and Superoxide. Proc Natl Acad Sci USA 1990;87:1620-1624.
44. Lymar SV, Hurst JK. Carbon dioxide: physiological catalyst for peroxynitrite-mediated cellular damage or cellular protectant? Chem Res Toxicol 1996;9:845-850.
45. Radi R, Denicola A, Freeman BA. Peroxynitrite reactions with carbon dioxide-bicarbonate. Methods Enzymol 1999;301:353-367.
46. Schopfer FJ, Baker PRS, Freeman BA. NO-dependent protein nitration: a cell signaling event or an oxidativc inflammatory response. Trends Biochem Sci 2003;28:646-654.
47. Baldus S, Castro L, Eiserich JP, Freeman BA. Is NO news bad news in acute respiratory distress syndrome? Am J Respir Crit Care Med 2001;163:308-310.
48. Asian M, Ryan TM, Townes TM, Coward L, Kirk MC, Barnes S, Alexander CB, Rosenfeld SS, Freeman BA. Nitric oxide-dependent generation of reactive species in sickle cell disease: renal and hepatocellular actin tyrosine nitration. J Biol Chem 2003;278:4194-4204.
49. Colasanti M, Persichini T, Menegazzi M, Marriotto S, Giordano E, Caldarera CM, Sogos V, Lauro GM, Suzuki H. Induction of nitric oxide synthase mRNA expression: suppression by exogenous nitric oxide. J Biol Chem 1995;270:26731-26733.
50. Eiserich JP, Estevez AG, Bambcrg TV, Ye YZ, Chumley PH, Beckman JS, Freeman BA. Microtubule dysfunction by posttranslational nitrotyrosination of α-tubulin: a nitric oxide-dependent mechanism of cellular injury. Proc Natl Acad Sci USA 1999;96:6365-6370.
51. Sitlipunt C, Steinberg KP, Ruzinski JT, Mylcs C, Zhu S, Goodman RB, Hudson DH, Matalon S, Martin TR. Nitric oxide and nitrotyrosine and the lungs of patients with acute respiratory distress syndrome. Am J Respir CrU Care Med 2001;163:503-510.
52. Weinberger B, Fakhrzadeh L, Heck DE, Laskin JD, Gardner CR, Laskin DL. Inhaled nitric oxide primes lung macrophages to produce reactive oxygen and nitrogen intermediates. Am J Respir Crit Care Med 1998;158:931-938.
53. Billert H, Drobnik L, Makowski A. The influence of acute hypercapnia on the quantity and oxidative metabolism of bronchoalveolar lavage-derived leukocytes in the mechanically ventilated rabbit. Med Sci Monil 2003;9:BR8-BR15.
54. Abu-Soud HM, Hazen SL. Nitric oxide modulates the catalytic activity of myeloperoxidasc. J Biol Chem 2000;275:5425-5430.
55. Baldus S, Eiserich JP, Brennan M-L, Jackson RM, Alexander CB, Freeman BA. Spatial mapping of pulmonary and vascular nitrotyrosine reveals the pivotal role of myeloperoxidase as a catalyst for tyrosine nitration in inflammatory diseases. Free Radic Biol Med 2002;33:886-893.
56. Haque IU, Huang C-J, Scumpia PO, Nasiroglu O, Skimming JW. Intravascular infusion of acid promotes intrapulmonary inducible nitric oxide synthase activity and impairs blood oxygecute;nation in rats. Crit Care Med 2003;31:1454-1460.
57. Bidani A, Wang CZ, Saggi SJ, Hemming TA. Evidence for pH sensitivity of tumor necrosis factor-α release by alveolar macrophages. Lung 1998;176:111-121.
58. Coakley RJ, Taggart C, Greene NG, McElvaney, O'Neill SJ. Ambient PcO2 modulates intracellular pH, intracellular oxidant generation, and interleukin-8 secretion in human neutrophils. J Leukoc Biol 2002;71:603-610.
59. D'Arcangelo D, Gaetano C, Capogrossi MC. Acidification prevents endothelial cell apoptosis by Axl activation. Circ Res 2002;91:e4-e12.
60. Takeshita K, Suzuki Y, Nishio K, Takeuchi O, Toda K, Kudo H, Miyao, Ishii M, Sato N, Naoki K, et al. Hypercapnic acidosis attenuates endotoxin-induced nuclear factor-κB activation. Am J Respir Cell Mol Biol 2003;29:124-132.
61. Duggan M, McCaul CL, McNamara PJ, Engelberts D, Ackerley C, Kavanagh BP. Atelectasis causes vascular leak and lethal right ventricular failure in uninjured rat lungs. Am J Respir Crit Care Med 2003;167:1633-1640.
John D. Lang, Mario Figueroa, K. David Sanders, Mutay Aslan, Yuliang Liu, Phillip Chumley, and Bruce A. Freeman
Departments of Anesthesiology and Biochemistry and Molecular Genetics, and The Center for Free Radical Biology, The University of Alabama at Birmingham, Birmingham, Alabama
(Received in original form February 28, 2003; accepted in final form October 1, 2004)
Supported by the American Heart Association and the National Institutes of Health (KO8 HL67982, RO1 HL64937, RO1 HL58115-6, and RO1 HL58115).
Correspondence and requests for reprints should be addressed to John D. Lang, Jr., M.D., The University of Alabama at Birmingham, Department of Anesthesiology, 845 Jefferson Tower, 619 South 19th Street, Birmingham, AL 35233-6810. E-mail: john.lang@ccc.uab.edu
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Am J Respir Crit Care Med Vol 171. pp 147-157, 2005
Originally Published in Press as DOI: 10.1164/rccm.200302-305OC on October 11, 2004
Internet address: www.atsjournals.org
Copyright American Thoracic Society Jan 15, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved