Only 20% of smokers develop chronic obstructive pulmonary dis ease. An important determinant of susceptibility is genomic variation. We undertook this study to define strains of mice with different susceptibilities for the development of smoking-induced emphysema because they could help identify genetic factors of susceptibility. NZWLac/J, C57BL6/J, A/J, SJ/L, and AKR/J strains were exposed to cigarette smoke for 6 months. Elastance (Htis), the extent of emphysema (mean linear intercept [Lm]), and the inflammatory cell and cytokine response were measured. NZWLac/J had no change in Lm or Htis (resistant). C57BL6/J, A/J, and SJ/L increased Lm, but not Htis (mildly susceptible). AKR/J increased Lm and Htis (super-susceptible). Only AKR/J had significant inflammation comprising macrophages, neutrophils, and T cells. The AKR/J showed an upregulation of Th1 cytokines whereas in the C57BL/6/J and NZWlac/J, cytokines did not change or were downregulated. We conclude that Lm, elastance, and inflammation are features that are needed to phenotype emphysema in mice. The inflammatory cell and cytokine profile may be an important determinant of the phenotype in response to cigarette smoke exposure. The identification of resistant and susceptible strains for the development of emphysema could be useful for genomic studies of emphysema susceptibility in mice and eventually in humans.
Keywords: elastance; emphysema; immunity; genomics; mice
Cigarette smoking is the most important environmental factor in the pathogenesis of chronic obstructive pulmonary disease (COPD). However, only approximately 20% of smokers develop COPD regardless of the amount smoked, indicating that other factors are at play. One important determinant of susceptibility is genomic variation. In a recent study, the heritability of FEV^sub 1^ in subjects with severe early onset COPD was 35% (1). The best known example of the influence of genomic variation on susceptibility to COPD is α-1 antitrypsin gene polymorphisms. However, these polymorphisms accounts for only 1-2% of COPD cases.
Susceptibility to COPD likely results from multiple genetic and environmental effects. Approaching such a problem by methods primarily designed to study single gene mendelian inheritance has proven difficult, particularly in genetically heterogeneous populations (2). A variety of candidate genes have been assessed using case control association studies, but the results have not been consistent across studies (3); to date, the results of investigations into the genetic basis for COPD have had limited success (4).
An essential step in the investigation of the genetic basis for complex diseases is an accurate assessment of phenotype. COPD is a heterogeneous disorder with variable morphologic and physiologic phenotypes (5). Therefore, careful phenotypic characterization is essential in studies of COPD genetics. Assessment of the degree of airflow limitation, the type of emphysema, the tissue elastance, and the nature of the inflammatory response are all important in characterizing the disease in humans and animal models.
Recent trends in molecular genetics and advances in molecular physiology make the mouse an ideal investigative model for determining genomic variants affecting susceptibility to COPD. It offers the advantage of studying a large number of genetically identical animals under controlled conditions. It complements human studies by introducing experimental control and the opportunity to pursue functional genomics and expression studies at the level of organs, tissues, or cells. Moreover, comparisons of the human and the mouse genome indicate significant conservation in gene order and chromosomal structure between these mammals (6).
Mice are susceptible to the development of emphysema, and several strains have been described that develop emphysema after prolonged cigarette smoke exposure (7). In recently published studies, we used a comprehensive pathologic and physiologic phenotyping approach to demonstrate the varying types and degrees of emphysema that mice develop during smoke exposure (8). We believe that an important step in the use of this model to detect susceptibility traits in COPD is to identify phenotypically resistant and susceptible strains. Generation of controlled crosses between these defined inbred strains could be of great value for identifying susceptibility trait loci and ultimately for the investigation of susceptibility and resistance to the disease in humans (9). In this investigation, we describe the disease phenotype of five different strains of mice with different susceptibilities for the development of emphysema, ranging from resistant to supersusceptible. Because it is now accepted that an inflammatory response is an important component of the development of COPD (10), for these studies, we chose mouse strains according to differences in their major histocompatibility complex (MHC) haplolypes. These haplotypes are important genetic determinants of an inflammatory immune response (11) and may be important in determining the inflammatory response of mice to cigarette smoke. Some of the results of these studies have been previously reported in abstract form (12, 13).
METHODS
Animals and Cigarette Smoke Exposure
Male NZWLac/J, C57BL6/J, A/J, SJL/J, and AKR/J (H-2 Allelic Haplotype z, b, a, s, and k, respectively) mice were divided into sham-exposed control animals (six animals per group) and cigarette smoke-exposed groups (six per group) at 3 months of age. The smoke-exposed animals were subjected for 5 days a week during 6 months (age 3-9 months) to the smoke of two standard research nonfiltered cigarettes (2R1) generated by a cigarette smoke exposure system (Cigarette Laboratory at the Tobacco and Health Research Institute, University of Kentucky, Lexington, KY). Carboxyhemoglobin levels in the blood were monitored. The body weights of all mice were measured monthly. The serum α-1 antitrypsin level in these animals were C57BL6/J, 2.5 mg/ml; SJL/J, 1.9 mg/ml; A/J, 1.7 mg/ml; AKR/J, 2.1 mg/ml; and NZWLac/J, not available.
Measurement of Lung Mechanics
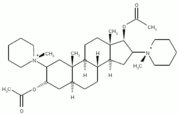
At the end of the 6 months of exposure, lung mechanics were measured in control and exposed animals. Each mouse was weighed and then deeply anesthetized by an intraperitoneal injection of xylazine (8 mg/kg) and pentobarbital (70 mg/kg), tracheostomized, and the trachea cannulated. The cannula was connected to a computer-controlled small animal ventilator (flexiVent; SCIREQ, Montreal, PQ, Canada), and regular quasisinusoidal ventilation was delivered at a frequency of 150 breaths/ minute and tidal volume of 5 ml/kg. The mouse was paralyzed with pancuronium bromide (0.8 mg/kg intraperitoneally), and the chest was opened. After stabilization, lung mechanics were measured at positive end-expiratory pressure (PEEP) levels of 1 to 9 cm H2O applied in random order by delivering a broad-band volume perturbation to the lungs for a period of 16 seconds, during which time the combined system of the ventilator and lungs remained closed to the environment (14).
The signals of cylinder pressure and piston volume displacement obtained during the perturbations were low-pass filtered and stored on a computer for analysis. The fast Fourier transforms of the data windows were used to calculate the input impedance of the lung, as described previously (15-17). The parameter Htis is equal to lung elastance at a frequency of ω = 1 rad/second = 0.16 Hz, and we used Htis versus PEEP to calculate an equivalent pressure-volume (P-V) curve for the lungs between 1 and 9 cm H2O. We previously have shown that these partial P-V curves are superimposable in the mechanical characteristics of the lung obtained by measuring pressure and volumes (8).
Lung Histology and the Quantitation of Emphysema
After measuring mechanics, animals were killed by exsanguination. The left lung was inflated with optimal cutting temperature fluid to a transpulmonary pressure of 25 cm H2O for 30 minutes and then flash frozen in isopentane and liquid nitrogen. Five-micrometer sagittal sections were cut, fixed, and stained with hematoxylin and eosin for histologie examination. Two nonconsecutive slides per mouse were coded and analyzed (magnification of ×100). Airspace enlargement was quantified by the mean linear intercept (Lm) in 20 randomly selected fields per slide (8).
Measurement of Lung Inflammatory Response
Ten nonconsecutive 5-µm sagittal sections per mouse were cut, fixed, and stained with specific immunostains for the assessment of alveolar wall inflammation (8): polymorphonuclear cells, rat anti-mouse neutrophil monoclonal dilution 1:33 (Cedarlane, Hornby, ON, Canada); lymphocytes, rat anti-mouse CD4+ monoclonal; rat anti-mouse CD8+ monoclonal (BD Biosciences Pharmingen, San Diego, CA) both dilution 1:250; γδ rat anti-mouse monoclonal 1:250 (Cedarlane); alveolar macrophages, rat anti-mouse macrophages/monocytes dilution 1:100 (Serotec Ltd., Oxford, UK). Twenty fields per slide (two slides per cell per mouse) at ×600 magnification were analyzed directly under the microscope in a blind fashion. In each ×600 magnification field, all of the cells and the immunostained staining cells were counted. Results were expressed as the percentage of positive staining cells relative to total cells.
Chemokine and Cytokine Assay
A Pharmingen's Riboquant multiprobe Rnase protection assay kit containing tumor necrosis factor-α, IL12p35, IL12p40, interleukin (IL)-10, macrophage inflammatory protein (MIP)-1β, MIP-1α, MIP-2, interferon inducible protein-10 (IP10), IL-6, and interferon-γ was used. Five micrograms of whole lung tissue mRNA was used. The Riboquant multiprobe Rnase protection assay is based on the hybridization of target RNA to P-labeled antisense RNA probe in vitro transcribed from a DNA template (18). Rnase treatment follows, resulting in degradation of single-stranded RNA and excess probe. The probe and target RNA are resolved by denaturing polyacrylamide gel electrophoresis, and the "protected" probe is visualized using autoradiography. Data extraction from the raw image and analysis were performed using the Eisen Lab software.
Statistics
Data are expressed as mean ± SEM or SD. Analysis of variance linear mixed-effects model were used to compare differences between groups. Statistical significance was taken as a p value of less than 0.05. Because pairwise comparisons were of primary interest, a t test was performed, followed by Bonferroni correction within each set of comparisons.
RESULTS
Cigarette smoke exposure was well tolerated by all five strains for the entire 6 months of exposure. Carbon monoxide concentrations obtained immediately after exposure ranged between 10% and 12%. Body weight in smokers was lower than in nonsmokers after 6 months of smoke exposure in C57BL6/J and AKR mice, but not in NZWLac/J, A/3, or SJ/L (Table 1).
Lung Morphometry
Figure 1 shows a representative lung field of the cigarette-exposed and -nonexposed resistant NZWLac/J, moderately susceptible C57BL6/J, and supersusceptible AKR/J strains. Figure 2 shows the Lm in the various experimental groups. The most striking increase in Lm was observed in the smoke-exposed AKR/J strain, where a 38% increase was observed compared with sham-exposed control animals. Lm also increased significantly after smoke exposure in the A/J (17.9%), SJ/L (23.8%), and C57BL6/J (13.2%) strains. Lm tended to decrease (-11%, p = NS) in the tobacco smoke-exposed NZWLac/J mice.
Lung Mechanics
Figure 3 shows the tissue elastance (Htis) value at 3 cm of PEEP in all strains. This level of PEEP was chosen because at all time points the minimum value of Htis occurs at a PEEP of 3 cm H2O. Significant decreases in Htis (loss of recoil) were seen in AKR/J (-39.4%, p
P-V Relationships
Figure 4 shows the partial P-V curves between 1 - and 9-cm H2O PEEP calculated from Htis in the NZWLac/J, C57BL6/J, and AKR/J after 6 months of smoke exposure compared with nonexposed control animals. The data from the pallid strain of mice from our previous publication (8) have been added to the figure for comparison. The AKR/J and pallid strains had significant increases in compliance after 6 months of smoking when compared with the nonexposed control animals (p
Inflammatory Response
The inflammatory response to 6 months of cigarette smoke-exposure in the five strains is shown in Table 2. Inflammatory cells are expressed as percentages of all cells in the lung. Of the strains developing an increase in Lm with smoking (A/J, SJL/J, C57BL6/J, and AKR/J), AKR/J showed the most intense inflammatory response with increases in the percentage of polymorphonuclear cells (p = 0.007), alveolar macrophages (p = 0.0004), CD8+ T cells (p = 0.048), CD4+ T cells (p = 0.01), and γδ T cells (p = 0.002). The SJL/J strain had an increase in γδ cells after smoking (p = 0.02). Of interest is that the αβ T cells (CD4+ and CD8 +) had a tendency to decrease after smoking for 6 months, and this trend was significant for the C57BL6/J CD8+ T cells (p = 0.009). We previously reported a similar trend in the C57BL6/J T cells (8). The resistant strain, NZWLac/J, had a significant increase in alveolar macrophages (p = 0.007) and γδ T cells (p = 0.001) but no changes in other inflammatory cell types.
Cytokines and Chemokines
Figures 5A-5C show the results of the cytokines and chemokines analysis by Rnase protection assay in the AKR/J, supersusceptible, C57BL/6/J as a representative of the mildly susceptible group, and the resistant NZWlac/J mice. In the AKR/J IL12p35 (p
In contrast to the findings in the AKR/J the resistant strain, NZWlac/J showed a downregulation of all measured cytokines and chemokines after cigarette smoke exposure with significant changes in tumor necrosis factor-α (p
DISCUSSION
In this investigation, we describe five strains of mice with strikingly different susceptibilities for the development of emphysema after tobacco smoke exposure. Based on the experimental results, we characterize the AKR/J strain as supersusceptible to the development of emphysema, the C57BL/6/J A/J and SJ/L strains as mildly susceptible, and the NZWLac/J as resistant. The degree of susceptibility was determined not only by increases of airspace enlargement, as determined by the Lm, but also by measuring the elastic properties of the lung (elastance), the functional counterpart of emphysema. In addition to the changes in the degree of emphysema, the cellular and inflammatory cytokine response after smoking exposure differed strikingly among the strains. T cells and a Th1 cytokine profile were present only in the lungs of the supersusceptible animals (change in both Lm and elastance).
Cigarette smoking is the major environmental factor responsible for the development of emphysema; however, only a minority of smokers develops the disease, suggesting that other risk factors are important. Family studies of patients with COPD have clearly demonstrated the importance of genetic factors in determining individual susceptibility to this disease, but most of these factors remain unexplained (19). Mice develop emphysema when exposed to cigarette smoke (7, 8, 20) or after genetic manipulations (21, 22), and the knowledge derived from this animal model could potentially help in the determining the genomic variants affecting susceptibility to COPD in humans. Different genetic manipulations using knockout and transgenic technology (matrix metalloproteinase [MMP]-12, interferon-γ, IL-13, tumor necrosis factor-α, and surfactant protein D among others) have been used to produce emphysema in mice, suggesting that some or all of these factors might be relevant for the development of emphysema in humans (21, 22).
In addition to manipulation of the expression of specific genes, a complementary approach in mice for the study of the risk factors for the development of COPD would be the characterization of inbred mice strains that differ in susceptibilities for the development of emphysema when exposed to cigarette smoke. The genetic determinants of resistance and susceptibility to the development of emphysema could then be investigated through cross-breeding, and this information could be applied to study the determinants of COPD in humans.
We based the selection of the strains studied on their differing MHC haplotypes reasoning that COPD is caused by an abnormal inflammatory reaction of the lung to cigarette smoke (Gold Guidelines definition) (10). The fact that T lymphocytes are a prominent component of the inflammation in COPD indicates that an adaptive immune reaction could be important for the development of emphysema (23, 24). Naïve T cells do not enter the lung; therefore, the increased numbers of T cells found in the lung in COPD ought to be stimulated after exposure to antigenic material originating in the lung, probably as a consequence of the innate immune reaction caused by cigarette smoke (25, 26). Although most immune diseases are polygenic, with multiple gene variants working in concert to produce the abnormal phenotype, it is well accepted that the MHC makes an important contribution to disease susceptibility (11, 27, 28), as differences in the ability of allelic variants of MHC molecules to present autoantigenic peptides are important determinants of susceptibility to autoimmune disease. Thus, it could be speculated that the MHC haplotypes could be an important genetic determinant for the development of emphysema in mice. In support of this contention is our own data derived from gene microchip analysis in response to cigarette smoke in mice, showing an important upregulation of some of the MHC genes in the susceptible animals (AKR/J) but not in the resistant (NZWlac/J) (29).
We defined the phenotype of the disease, emphysema, by determining the degree of airspace enlargement by Lm and by measuring the mechanical properties of the lung, specifically lung elastance. We previously have demonstrated that for a similar degree of airspace enlargement functional abnormalities in the lung can vary, and thus, we believe that the mechanical properties of the lung are important for phenotype characterization in mice, (8) reasoning that true emphysema ought to have a functional counterpart, namely loss of elastance. Except for the NZWLac/J strain, all other strains had increased Lm after 6 months of smoking. This increase ranged from 13.2% for C57BL6/J to 38% for AKR/J. However, changes in Lm after smoking were not always mirrored by changes in lung mechanics. The reasons for this disparity are not clear. One possibility is that a threshold change in airspace enlargement is necessary to alter the mechanical characteristics of the lung. Of note, the strains with the greatest change in compliance (elastance), the AKR/J strain and the pallid mouse in our previous publication (8), also had the greatest increases in Lm. Alternatively, the distribution of the emphysema throughout the lung (diffuse versus localized) might be important in determining the loss of elasticity and increased compliance. The emphysema in the C57BL/6 strain is limited to the alveolar ducts, whereas in both the Pallid (8) and AKR/J strains, the emphysema is more diffused, also affecting the alveoli.
An interesting difference in the response of the different strains to smoke exposure is the weight change. When compared with nonsmokers, only the AKR/J, supersusceptible, and the C57BL6/J mildly susceptible failed to gain weight over 6 months of smoke exposure. The lack of weight gain was also observed in the susceptible pallid strain (8). The alterations in weight cannot be a function of smoke exposure alone, but rather must be clue to the interaction of smoking and other strain characteristics. Inflammation could be one cause for the lack of weight in the AKR/J and pallid strains, but we have been unable to show a sustained inflammatory response in the lungs of C57BL/6/J mice that also fail to maintain their weight. Thus, other mechanisms would have to be implicated, along with an ongoing inflammatory process.
The inflammatory response to cigarette smoke exposure observed in this investigation bears striking similarities to the inflammation in the lung parenchyma seen in human smokers with and without COPD (23). Our results are not necessarily comparable to the inflammatory profile obtained by bronchoalveolar lavage in mice exposed to cigarette smoke (30). Bronchoalveolar lavage, at least in humans, reflects a different lung compartment and the inflammatory profile in bronchoalveolar lavage and lung airway biopsies is quite different (31). Strain-specific differences in inflammatory response to cigarette smoke exposure might be a basis, at least in part, for the different susceptibilities to the development of emphysema. A limitation of this investigation is that the inflammatory response in the lungs was determined only after 6 months of smoke exposure; thus, the dynamic nature of the inflammatory process and the inflammatory changes after short periods of cigarette smoke exposure reported by others (32) were not investigated. However, our results determined the inflammatory process that develops after chronic exposure to cigarette smoke. The differences in response demonstrated between strains are likely meaningful. Of note, the "supersusceptible" AKR/J strain had a marked inflammatory infiltrate comprised of CD4+, CD8+, γδ T cells, polymorphonuclear cells, and alveolar macrophages. This pattern of inflammation is similar but of greater magnitude to the inflammatory reaction found in the lungs of pallid mice that also develop emphysema accompanied by loss of elastic recoil (8). The resistant NZWLac/J strain showed a much milder inflammatory reaction comprised of macrophages and γδ cells but conspicuously lacked CD4+ and CD8+ T cells and polymorphonuclear cells. In the C57BL6/J, SJ/L, and A/J strains, the only clear inflammatory reaction seen after 6 months of smoking was an increase of γδ cells in the SJ/L strain.
A potentially important component of the inflammatory profile in smoke-exposed mice is the increased γδ cells, which we have also described in human smokers (23). It is believed that tissue-associated subsets of γδ cells respond to tissue-specific "stress antigens" derived primarily from the epithelium. The role of these cells is complex, and by their ability to influence other immune cells, they can modulate the course and outcome of a variety of inflammatory immune responses (33). Early in an inflammatory process, there is a large increase in γδ cells (Vγ4+) in the lung. These cells are proinflammatory, express interferon-γ, and induce polymorphonuclear cell accumulation in the lung. Later, in an inflammatory process, a γδ cell (Vγ1+) can have an immunoregulatory role, express IL-4, and suppress inflammation (34). Thus, the γδ T cells in resistant and susceptible mice strains for the development of emphysema could have different roles, either proinflammatory or even cytolytic in the susceptible and/ or immunoregulatory or suppressor in the resistant strains.
The cytokines and chemokines investigated in the resistant NZW/Lac/J, the mildly susceptible C57BL6/J, as a representative strain of this group, and the supersusceptible AKR/J mirror the cellular inflammatory response. The differences among the three strains are striking. There is a broad upregulation of the inflammatory mediators pointing toward a Th1-adaptive inflammatory response in the AKR/J with significant increases in IL-12p35 and p40 and the CC chemokines MIP-1β and MIP-1α. MIP-1α and MIP-1β are considered along with interferon-γ type 1 cytokines and are secreted together with interferon-γ in vitro and in vivo. Furthermore, it has been shown that both natural killer (NK) and T cells use MIP-1α and MIP-1β, along with interferon-γ, RANTES, and interferon-inducible T-cell α-chemoattractant (I-TAC) as a "functional unit" to drive the Th1 response in vivo (35). Besides being chemoattractants for macrophages and distinct populations of T cells, mainly CD8+, MIP-1α, and MIP-1β have additional functions in the immune system, augmenting the cytolytic capacity of T cells and co-stimulating T-cell proliferation and IL-2 synthesis (36-38). The significant upregulation of MIP-1α and MIP-1β in the AKR/J, which develops significant CD8+ and CD4+ T-cell inflammation after smoke exposure, suggests that these chemokines may be playing an important role in the recruitment and activation of the T cells, mainly the CD8+, in the susceptible strain, and account for the lack of significant T-cell response in the other strains in which these chemokines were not upregulated. Furthermore, these chemokines might be an important mediator of tissue injury in the production of emphysema because specialized CC-chemokines secretion by Th1 cells contributes to their high pathogenic potential, and MIP-1α has been identified as an important mediator in the pathogenesis of other immune-mediated diseases such as myocarditis (39).
In contrast with the pattern of cytokine upregulation seen in the AKR/J strain, the resistant NZWlac/J downregulaled most of the inflammatory mediators studied, whereas the C57BL/6/J did not show any significant change from control animals, except for an increase in IL-10, a cytokine also increased in the AKR/J. IL-10 is a potent antiinflammatory cytokine that modulates expression of cytokines, soluble mediators, and cell surface molecules by cells of myeloid origin, with important consequences for their ability to activate and sustain immune and inflammatory responses (40). IL-10 inhibits production of most inducible chemokines that are involved in inflammation, including MIP-1α and MIP-1β. This scenario could explain the findings in the C57BL/6/J strain, in which no cellular inflammation and no cytokine upregulation are seen; however, a different explanation for the upregulation of IL-10 in the supersusceptible AKR/J will have to be sought. It is of interest that although IL-10 generally inhibits macrophage and CD-4+ T-cell function, it stimulates the development of B cells and promotes growth, differentiation, and cytotoxic activity of CD8+ T cells by activating activation protein-1 (AP-1) and nuclear factor-κB in CD-8+ T cells (41). Studies of IL-10 in vivo in models of autoimmunity, cancer, and transplantation have revealed that IL-10 can effect very different outcomes depending of timing, dose, and location of expression; in some scenarios, the expected immunosupprcssive activities are observed, whereas in others, IL-10 enhances immune or inflammatory responses (40). Thus, it is possible that IL-10 could be playing different roles in the C57BL/6/J, in which it could suppress inflammation, and in the AKR/J in which the inflammation, chemokine expression, and macrophage function are obviously not downregulated.
These data suggest that an adaptive immune inflammatory reaction with CD4+ and CD8+ T cells and a Th1 chemokine-cytokine profile might be an important contributor in the production of emphysema in the supersusceptible animals. The Th1 T-cell adaptive immune response could be also responsible for the recruitment and maintenance in the lung of alveolar macrophages and neutrophils in the supersusceptible AKR/J, which would participate in the pathogenic process. Furthermore, the presence of high levels of MIP-1α, and possibly IL-10, highlights the potential importance of the CD8+ T cell in the mechanism of the cigarette-induced emphysema in the mouse model. In contrast, the inflammatory response found in the resistant and mildly susceptible strains appears to be suppressed, and this might prevent the development of functionally significant emphysema.
In summary, we have characterized the susceptibility to the development of emphysema by cigarette smoke exposure in six strains of mice with different MHC haplotypes: NZWLac/J, C57BL6/J, A/J, SJ/L, AKR/J, and pallid (8), a strain with the same MHC as the C57BL/6/J but with low levels of α-1 antitrypsin in blood (42). By using the anatomic, physiologic, and inflammatory response, we define these strains as resistant: NZWLac/J no change in Lm, elastance, and no T (αβ)-cell inflammation; mildly susceptible: C57BL/6/J, A/J, SJ/L, characterized by changes in LM, but no changes in elastance, and no T (αβ)-cell inflammation; susceptible: pallid, changes in Lm, changes in elastance, and T (αβ)-cell inflammation; and supersusceptible: AKR/J. With the advent of the description of the full genome in humans and in mice (C57BL6/J) (6), the similarity in the ontology of both genomes, and the very close synteny between human and mice chromosomes, the study of the genomics of the resistant and susceptible strains might provide very helpful leads for the investigation of the genomic consequences leading into COPD in humans (6).
In conclusion, mice like humans, show different susceptibilities to the development of COPD. The molecular mechanisms underlying the pathophysiology of COPD are undoubtedly complex. Understanding how biological variability arises from those individual factors that contribute to COPD will provide the basis for understanding the molecular physiology and heritability of this disorder. The ability to sustain an inflammatory response, or perhaps more properly, the lack of ability to suppress such a response, could be one of those factors. One of the most striking differences in the response to cigarette smoking in the strains studied is the Th1 T-cell inflammatory response in the supersusceptible strain, indicative of an adaptive immune response and suggestive of an autoimmune component in the mechanism of emphysema production (23, 43, 44). The fact that this response is similar to the response seen in humans (23) highlights the importance of these strains as an animal model for emphysema.
Conflict of interest Statement: A.G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; Y.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; Y.T. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.T. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.Y. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; H.G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.T. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; K.W. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.R.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.G.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
1. Silverman KK, Mosley JD, Palmer LJ, Barth M, Senter JM, Brown A, Drazen JM, Kwiatkowski DJ, Chapman HA, Campbell E, et al. Genomewide linkage analysis of severe, early-onset chronic obstructive pulmonary disease: airflow obstruction and chronic bronchitis phenotypes. Hum Mol Genet 2002;11:623-632.
2. Guttmacher AE, Collins FS. Genomic medicine: a primer. N Engl J Med 2002;347:1512-1519.
3. Lomas DA, Silverman EK. The genetics of chronic obstructive pulmonary disease. Respir Res 2001;2:20-6.
4. Hoidal JR. Genetics of COPD: present and future. Eur Respir J 2001;18: 741-743.
5. Kim WD, Eidelman DH, Izquierdo JL, Ghezzo H, Saetta MP, Cosio MG. Centrilobular and panlobular emphysema in smokers: two distinct morphologic and functional entities. Am Rev Respir Dis 1991;144: 1385-390.
6. Mouse Genome Sequencing Consortium. Initial sequencing and comparative analysis of the mouse genome. Nature 2002;420:520-562.
7. Shapiro SD. Animal models for chronic obstructive pulmonary disease: age of klotho and marlboro mice. Am J Respir Cell Mol Biol 2000;22: 4-7.
8. Takubo Y, Guerassimov A, Ghezzo H, Triantafillopoulos A, Bates JHT, Hoidal JR, Cosio MG. Alpha-1 antitrypsin determines the pattern of emphysema and function in tobacco smoke-exposed mice: parallels with human diseases. Am J Respir Crit Care Med 2002;166:1596-1603.
9. Dyment D, Ebers GC. An array of sunshine in multiple sclerosis. N Engl J Med 2002;347:1445-1447.
10. Pauwels RA, Buist AS, Ma P, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001;163:1256-1276.
11. Davidson A, Diamond B. Autoimmune diseases. N Engl J Med 2001;345: 340-350.
12. Takubo Y, Guerassimov A, Triantafillopoulos A, Ghezzo H, Hoidal JR, Cosio MG. Cigarette smoked-induced emphysema in mice with different haplotypes of MHC and alpha-1 antitrypsin levels. Am J Respir Crit Care Med 2002;165:A602.
13. Guerassimov A, Takubo Y, Triantafillopoulos A, Ghezzo H, Hoidal JR, Cosio MG. Inflammatory cell profile in the lungs of smoking mice with different major histocompatibility genes [abstract]. Am J Respir Crit Care Med 2002;165:A599.
14. Hantos Z, Daroczy B, Suki B, Nagy S, Fredberg JJ. Input impedance and peripheral inhomogeneity of dog lungs. J Appl Physiol 1992;72: 168-178.
15. Bates JHT, Schuessler TF, Dolman C, Eidelman DH. Temporal dynamics of acute isovolume bronchoconstriction in the rat. J Appl Physiol 1997;82:55-62.
16. Hirai T, McKeown KA, Gomes RFM, Bates JHT. Effects of lung volume on lung and chest wall mechanics in rats. J Appl Physiol 1999;86:16-21.
17. Schuessler TF, Bates JHT. A computer controlled research ventilator for small animals: design and evaluation. IEEE Trans Biomed Eng 1995; 42:860-866.
18. Gilman M. Ribonuclease protection assay. In: Ausubel FM, Brent R, Kingston RE, Moore DD, Seidman JG, Smith JA, Stuhi K, editors. Current protocols in molecular biology. Vol. 1. New York: John Wiley and Sons; 1993. p. 4.7.1-4.7.8.
19. Silverman EK, Chapman HA, Drazen JM, Weiss ST, Rosner B, Campbell EJ, O'Donnell WJ, Reilly JJ, Ginns L, Mentzer S, et al. Genetic epidemiology of severe, early onset COPD: risk to relatives for airflow obstruction and chronic bronchitis. Risk to relatives for airflow obstruction and chronic bronchitis. Am J Respir Crit Care Med 1998;157: 1770-1778.
20. Cavarra E, Bartalesi B, Lucatteli M, Fineschi S, Lunghi B, Gambelli F, Ortiz LA, Martorana PA, Lungarella G. Effects of cigarette smoke in mice with different levels of alpha-1 proteinase inhibitor and sensitivity to oxidants. Am J Respir Crit Care Med 2001;164:886-890.
21. Mahadeva R, Shapiro SD. Chronic obstructive pulmonary disease-3: experimental animal models of pulmonary emphysema. Thorax 2002;57: 908-914.
22. Morris DG, Huang X, Kaminski N, Wang Y, Shapiro SD, Dolganov G, Glick A, Sheppard D. Loss of integrin αVβ6-medialed TGF-β activation causes MMP12-depcndent emphysema. Nature 2003;422:169-173.
23. Majo J, Ghezzo H, Cosio MG. Lymphocyte population and apoptosis in the lungs of smokers and their relation to emphysema. Eur Resptr J 2001;17:946-953.
24. Cosio MG, Majo J, Cosio Piquenas MG. Inflammation of the airways and lung parenchyma in COPD: role of the T-cells. Chest 2002;121: 160S-165S.
25. Kamradt T, Mitchison NA. Tolerance and autoimmunily. N Engl J Med 2001;344:655-664.
26. Butcher EC, Picker LJ. Lymphocyte homing and homeostasis. Science 1996;272:60-66.
27. Klein J, Sato A. The HLA system. N Engl J Med 2000;343:702-709.
28. McDevitt H. Discovering the role of the major histocompatibility complex in the immune response. Annu Rev Immunol 2000;18:1-17.
29. Hoshino Y, Radzioch D, Ghezzo H, Marrades R, Triantafillopoulos A, Hoidal J, Skamene E, Cosio MG. Smoke-induced and inherent differences at the level of gene expression in mice with different susceptibility to emphysema. Eur Respir J 2003;22:195s.
30. Shapiro SD, Goldstein NM, Houghton AM, Kobayashi DK, Kelley D, Belaaouaj A. Neutrophil elastase contributes to cigarette smoke-induced emphysema in mice. Am J Pathol 2003;163:2329-2335.
31. Maestrelli P, Saetta M, Di Stefano A, Calcagni PG, Turato G, Ruggieri MP, Roggeri A, Mapp CE, Fabbri LM. Comparison of leukocyte counts in sputum, bronchial biopsies, and bronchoalveolar lavage. Am J Resilr Crit Care Med 1995;152:1926-1931.
32. Churg A, Dai J, Tai H, Xie C, Wright JL. Tumor necrosis factor-α is central to acute cigarette smoke-induced inflammation and connective tissue breakdown. Am J Respir Crit Cure Med 2002;166:849-854.
33. Carding S, Egan P. γδ T-cells: functional plasticity and heterogeneity. Nat Rev Immunol 2002;2:336-345.
34. Hayday A, Tigelaar R. Immunoregulation in the tissues by γδ T-cells. Nat Rev Immunol 2003;3:233-242.
35. Dorner BG, Scheffold A, Rolph MS, Hüser MB, Kaufmann SHE, Radbruch A, Flesch IEA, Kroczek RA. MIP-1 alpha, MIP-1 beta, RANTES, and ATAC/lymphotactin function together with IFN-γ as type 1 cytokines. Proc Natl Acad Sci USA 2002;99:6181-6186.
36. Taub DD, Sayers TJ, Carter CR, Ortaldo JR. Alpha and beta chemokines induce NK cell migration and enhance NK-mediated cytolysis. J Immunol 1992;155:3877-3888.
37. Taub DD, Turcovski-Corrales SM, Key ML, Longo DL, Murphy WJ. Chemokines and lymphocyte activation: I: beta chemokines costimulate human T lymphocyte activation in vitro. J Immunol 1996;156: 2095-2103.
38. Maric M, Chen L, Sherry B, Liu Y. A mechanism for selective recruitment of CD8 T cells into B7-1 transfected plasmacytoma: role of macrophage-inflammatory prolein 1 alpha. J Immunol 1997;159:360-368.
39. Song HK, Noorchashm H, Lin TH, Moore DJ, Greeley SA, Caton AJ, Naji A. Specialized CC-chemokine secretion by Th1 cells in destructive autoimmune myocarditis. J Autoimmunity 2003;21:295-303.
40. Moore KW, de Waal Malefyt R, Coffman RL, O'Garra A. Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol 2001;19:6830-765.
41. Hurme M, Henttinen T, Karppelin M, Varkila K, Matikainen S. Effect of Interleukin-10 on NF-kB and AP-1 activities in interleukin-2 dependent CD8 T lymphoblasts. Immunol Lett 1994;42:129-133.
42. Martorana PA, Brand T, Gardi C, van Even P, de Santi MM, Calzoni P, Marcohongo P, Lungarella G. The pallid mouse: a model of genetic alpha 1-antitrypsin deficiency. Lab Invest 1993;68:233-241.
43. Agusti A, MacNee W, Donaldson K, Cosio MG. Does COPD have an autoimmune component? Thorax 2003;58:832-834.
44. Cosio MG. Autoimmunity, T-cells and STAT-4 in the pathogenesis of chronic obstructive pulmonary disease [editorial]. Eur Respir J 2004;24: 3-5.
Alexei Guerassimov, Yuma Hoshino, Yasutaka Takubo, Antony Turcotte, Midori Yamamoto, Heberto Ghezzo, Alexandra Triantafillopoulos, Kevin Whittaker, John R. Hoidal, and Manuel G. Cosio
Respiratory Division, Royal Victoria Hospital, Meakins-Christie Laboratories, McGill University, Montreal, Quebec, Canada; and Division of Respiratory, Clinical Care and Occupational Medicine, University of Utah Health Sciences Center, Salt Lake City, Utah
(Received in original form September 11, 2003; accepted in final form July 26, 2004)
Supported by the Alpha-1 Foundation Fellowship (A.G.), an Alpha-1 Foundation Grant, National Institutes of Health Grant #R01 HL66543, and the Lloyd Carr-Harris Foundation.
Correspondence and requests for reprints should be addressed to Manuel G. Cosio, M.D., McGill University, Royal Victoria Hospital, Respiratory Division, Room L4.11, 687 Pine Avenue West, Montreal, PQ, H3A 1A1 Canada. E-mail: manuel. cosio@muhc.mcgill.ca
Am J Respir Crit Care Med Vol 170. pp 974-980, 2004
Originally Published in Press as DOI: 10.1164/rccm.200309-1270OC on July 28, 2004
Internet address: www.atsjournals.org
Copyright American Thoracic Society Nov 1, 2004
Provided by ProQuest Information and Learning Company. All rights Reserved