By recognizing early signs of kidney disease, you can stem its devastating effects and may prevent or delay end-stage renal failure.
CHRONIC RENAL FAILURE (CRF) is the progressive loss of kidney function. Damaged by disease or another insult, the kidneys gradually lose their ability to perform their main functions: removing fluid and wastes from the body and maintaining kidney-regulated chemicals in the bloodstream. (See Around the Bend: How the Kidneys Work.) In many cases, CRF leads to incurable end-stage renal disease (ESRD).
People with diabetes are at greatest risk for developing CRF, which is expected to affect 3 million Americans by 2008. At present, CRF contributes to 50,000 deaths per year in the United States and is a particularly costly disease to treat, in part because of the need for dialysis.
But early recognition of CRF, followed by aggressive management and treatment strategies, can maintain kidney function and prevent or slow the progression of CRF to ESRD. Here's what you need to know.
Types of kidney failure Acute renal failure is a sudden decline in renal function with at least a 50% decrease in glomerular filtration rate (GFR). Acute renal failure can occur from decreased blood flow to the kidneys (prerenal failure); acute damage to the renal parenchyma, such as from trauma or toxins (intrinsic renal failure); or conditions that block urine flow (postrenal failure). Kidney function usually returns if the underlying problem resolves. (For more information, see "How Acute Renal Failure Puts the Brakes on Kidney Function" in the January issue of Nursing2003.)
In contrast, chronic renal failure occurs when disease or another disorder causes progressive destruction of nephrons and loss of kidney function. Typically, both kidneys are affected, and the patient may notice signs and symptoms when the GFR falls to below 30% of normal. When 90% to 95% of the nephrons stop functioning, the patient is considered to have ESRD. Signs and symptoms of uremia develop, leading to hemodynamic instability and potentially fatal complications.
Who's at risk?
The following conditions increase a patient's risk of CRF:
* Type 1 or Type 2 diabetes, which damage the glomeruli
* hypertension, which damages renal vessels over time
* glomerulonephritis, or chronic inflammation of the glomeruli
* polycystic kidney disease, a hereditary disorder that causes cysts to form in the kidneys
* other systemic diseases, such as sickle-cell disease and systemic lupus erythematosus.
Recognizing clues
Because symptoms of CRF may not appear for a long time-perhaps not until the patient's GFR falls below 30% of normal-you need to stay alert for more subtle indications of trouble brewing. When taking a patient's history, for example, raise a red flag if he has any risk factors for CRF, such as diabetes or chronic hypertension.
Certain abnormal lab values-especially elevated serum creatinine and urine protein levels-are early markers of kidney disease. By casting a knowledgeable eye on lab values, you may spot CRF at an early stage. See Assessing Renal Function for more information.
Uremia, although uncommon, may be obvious in a patient with undiagnosed CRF who has severe renal dysfunction. Signs and symptoms include:
* bad, urinous breath or an ammonia-like taste in the mouth
* edema around the eyes, face, arms, hands, and feet, caused by fluid overload
* hypertension from excessive serum sodium levels and extracellular fluid volume expansion, as well as renin hypersecretion
* extended neck veins from excess extracellular fluid
* anemia from decreased red blood cell (RBC) production and shortened RBC survival (because of uremic toxins)
* fatigue from anemia and toxic substances in the blood
* neurologic disturbances caused by uremic toxins, including lethargy, impaired mentation, and sleep disorders
* nausea, vomiting, and anorexia from retention of urea and metabolic waste products
* headaches and blurred vision from extracellular volume expansion and uremic toxins
* pruritus from phosphorus, calcium, and aluminum buildup
* shortness of breath secondary to fluid buildup in the body (which can lead to pulmonary edema if untreated)
* bone and joint problems from bone resorption associated with vitamin D deficiency, demineralization, and calcium and phosphate imbalances.
* bone pain, paresthesia, numbness, weakness, or tremors of the extremities caused by uremic toxins.
Assess and document your patients vital signs, lung and heart sounds, and cardiac rhythm. Assess for tetany: Are Chvosteks and Trousseaus signs (indicating hypocalcemia) present?
If your patients health care provider suspects kidney disease, she'll order an extensive renal assessment to determine the cause of kidney dysfunction and to guide interventions. These diagnostic tests provide helpful information:
* Renal ultrasonography helps pinpoint obstruction in the urinary collecting system, manifested by dilation of the collecting system and ureters. This is the most useful test for diagnosing CRF, and it also confirms the presence of two symmetric kidneys and estimates kidney size.
* A kidneys-ureters-bladder X-ray can help detect renal calculi, renal pelvis enlargement (hydronephrosis), tumors, or cysts.
* Noncontrast computed tomography reveals the renal parenchyma and can identify lesions, masses, cysts, calculi, obstructions, congenital anomalies, and abnormal fluid collection.
* A renal radionudide scan detects renal artery stenosis, especially if performed with captopril.
* A renal biopsy helps determine the extent of pathology. This test is reserved for patients with near-normal kidney size when a diagnosis can't be made by less invasive testing.
Managing multiple problems
Even in its early stages, CRF affects multiple body systems. Possible complications include left ventricular hypertrophy, anemia, hypoalbuminemia, secondary hyperparathyroidism, metabolic acidosis, dyslipidemia, hypertension, and malnutrition. Early evaluation and intervention by a nephrologist-led multidisciplinary team can slow disease progression, reduce the need for dialysis, and improve the patients quality of life.
Management strategies should include controlling independent risk factors that make things worse. Help implement the following interventions:
* Improve nutrition. Good eating habits can help prevent or slow atherosclerotic disease, hyperlipidemia, diabetes, hypertension, and uremia-related muscle wasting. Teach the patient to keep his diet low in sodium, potassium, and phosphorus, three substances regulated by the kidneys. Reducing protein may alleviate uremic symptoms but can also lead to further muscle wasting. Protein restriction should be guided by the patients GFR and be part of an overall dietary program to avoid malnutrition.
* Monitor electrolyte levels, especially sodium, potassium, calcium, phosphate, and magnesium, because even minor shifts in electrolytes can be lethal.
* Manage anemia. Treating CRF-related anemia commonly involves long-term intravenous (I.V) or subcutaneous administration of erythropoietin to elevate or maintain erythrocyte levels and reduce the need for transfusion. Darbepoetin alfa (Aranesp), a recombinant erythropoiesis-stimulating protein, requires less frequent dosing than erythropoietin. Oral or I.V iron supplements can enhance the response to erythropoietin.
* Control hypertension. Lowering blood pressure slows renal decline and damage. Angiotensin-converting enzyme (ACE) inhibitors are considered first-line drugs because they delay CRF progression, help reduce proteinuria and microalbuminuria, and improve left ventricular function. However, because they can also abruptly reduce GFR, closely monitor patients for renal deterioration and hyperkalemia. Calcium channel blockers are a useful alternative for patients who can't tolerate ACE inhibitors or don't respond to them.
* Maintain glycemic control. Abnormal glucose metabolism and hyperinsulinemia have been connected to the development of atherosclerotic complications in patients with CRF Closely monitor the patient's serum glucose level and hemoglobin A1C.
Treating ESRD
If the patients condition progresses to ESRD, he has two treatment options: dialysis or a kidney transplant. Dialysis steps in for the failed kidneys but doesn't cure kidney disease or CRF-related complications, and it may cause dialysisrelated complications and reduce the quality of life.
During hemodialysis, the more common type, the patient's blood is sent through a dialyzer and returned after toxins and excess fluid are removed. Hemodialysis is usually performed three times a week, with each treatment lasting 3 to 5 hours, sometimes more. Common adverse reactions include fluid and electrolyte imbalances, hypotension, light-headedness, leg cramps, nausea, and vomiting.
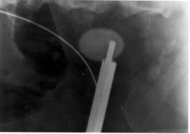
Peritoneal dialysis uses the peritoneum to filter the blood without removing it from the body. Dialysate is administered into the peritoneal space, where fluid and electrolyte exchange between the dialysate and bloodstream occur. Then the dialysate is drained via a peritoneal catheter. The most common complication of peritoneal dialysis is peritonitis. (For more information on this procedure, see "When Your Patient Needs Peritoneal Dialysis" in the August issue of Nursing2003.)
Transplantation can relieve many symptoms and restore well-being even in a patient with complete kidney failure. Surgery typically takes 3 to 4 hours. The diseased kidney is left in place, and the healthy one is transplanted just below it in the lower abdomen. The donor renal artery and vein are anastomosed to the recipient's iliac artery and vein, and the donor ureter is anastomosed to the recipients bladder.
The kidney usually doesn't begin to function for at least 24 hours after transplantation. Close monitoring of kidney function and lifelong immunosuppression are essential to prevent graft rejection.
Contraindications to transplantation include human immunodeficiency virus (HIV) infection, disseminated or untreated cancer, severe psychiatric disease, persistent substance abuse, and refractory heart failure.
Offering emotional support
A patient with CRF must cope with the realization that, eventually, renal replacement therapy will probably become a permanent part of his life. The diagnosis, coupled with an understanding that dialysis isn't a cure, can trigger anxiety, denial, frustration, anger, depression, and hopelessness. With your knowledge and compassion, you can help guide him and his family through these painful emotions and teach them how to manage the condition effectively.
SELECTED REFERENCES
Bell, J., and Ross, K.: "Kidney Transplant Recipient Referral and Evaluation (Focus on Transplantation)." Nephrology Nursing Journal. 29(5):477-496, October 2002.
Jancin, B.: "Targeted Screening Detects Patients at High Risk for Chronic Kidney Disease," Family Practice News. 31(17):13, September 1, 2001.
Perazella, M.: "Chronic Kidney Disease: The Silent Epidemic," Hospital Physician. 39(3):15-17, March 2003.
Ruggenenti, P., et al.: "Progression, Remission, Regression of Chronic Renal Diseases." The Lancet. 357(9268):1601-1608, May 19, 2001.
Stephenson. J.: "Hypertension and Kidney Disease," JAMA. 284(19):2445, November 15, 2000.
Stevens, L: "Kidney Failure," JAMA. 286(22):2898, December 12, 2001.
BY JAN D. CANNON, RN, MSN
Jan D. Cannon is an instructor of nursing at Amarillo (Tex.) College.
Copyright Springhouse Corporation Jan 2004
Provided by ProQuest Information and Learning Company. All rights Reserved