The incidence of rickets caused by vitamin D deficiency, once a common health problem among British Asian children, seems to have declined during the past decade.[1] We describe six cases of florid rickets in infants aged 10 to 28 months who were referred to our paediatric unit by local general practitioners between 1995 and 1997. They were all born in the United Kingdom to parents who were either postgraduate students or recent immigrants. All the children had been breast fed for a prolonged period without vitamin D supplementation. The mothers of these infants had not received vitamin D supplements during pregnancy or lactation.
Case reports
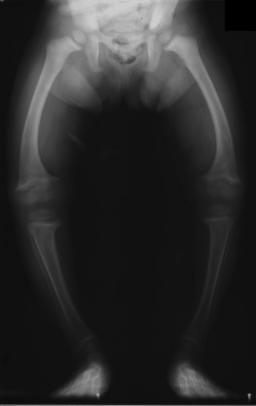
All six patients had several of the clinical signs and symptoms of rickets: bow legs, rickety rosary, swelling of the ends of long bones, frontal bossing of the skull, delayed dentition, poor growth, and slow motor development. They all had classic radiological features of rickets, including generalised osteopenia, widening of the growth plates, and cupping of metaphyseal regions of long bones (figure). As shown in table 1, biochemical features of the disease included increased serum alkaline phosphatase activity for their age, low serum concentrations of 25-hydroxycholecalciferol (a measure of vitamin D status; concentrations [is less than] 5 ng/ml are associated with rickets or osteomalacia), and secondary hyperparathyroidism leading to hypophosphataemia and normal or above normal serum concentrations of 1,25-dihydroxycholecalcfferol. Two subjects had asymptomatic hypocalcaemia. All the subjects had been breast fed, either exclusively or for prolonged periods of time (table 1). No infant had received vitamin D supplements. Treatment with oral cholecalcfferol (vitamin [D.sub.3]) successfully healed the rickets in all subjects.
25(OH)D=25-hydroxycholecalciferol concentration. 1,25[(OH).sub.2]=1,25-dihydroxycholecalciferol concentration.
(*) Fathers of these toddlers were postgraduate students.
([dagger]) In addition to genu varum and swelling of ends of long bones, this patient presented with swelling of right clavicle from healing pathological fracture.
All infants were born in the United Kingdom at full term. Their mothers had not received vitamin D supplements during pregnancy or while nursing their infants. None of the patients received supplementary vitamin D after birth. Four out of five mothers of the toddlers who agreed to undergo biochemical testing were deficient in vitamin D, with low serum 25-hydroxycholecalciferol concentrations (table 1). These four mothers were all practising Muslims who wore concealing clothing when attending the hospital. Further inquiries revealed that three of them had nonspecific aches and pains in their legs.
Discussion
Rickets resulting from vitamin D deficiency is a disorder of growing children in which the newly formed bone matrix does not become mineralised. In humans the main source of vitamin D is formed by conversion of 7-dehydrocholesterol in the skin to cholecalciferol (vitamin [D.sub.3]) with exposure to the sun's ultraviolet B radiation. This cutaneous synthesis is compromised in people with increased skin pigmentation[2] and those who wear concealing clothing or live predominantly an indoor life for religious and cultural reasons.
Environmental factors that reduce the penetration of antirachitic ultraviolet B radiation (290-310 nm) through the atmosphere include cloudy skies, pollution, and residence in northern latitudes, where the sun is too low in the sky during winter months. Under these conditions of insufficient exposure of the skin to sunlight, dietary and supplemental sources of vitamin D are important in preventing rickets in children and osteomalacia in adults.
Infants born to mothers with subclinical vitamin D deficiency have reduced umbilical cord blood concentrations of 25-hydroxycholecalciferol.[3] The prolonged consumption of breast milk is another risk factor for developing vitamin D deficiency as human milk contains only about 1 [micro]g of vitamin D per litre, with concentrations varying according to maternal vitamin D status.[4] Thus, exclusively breast fed infants with insufficient exposure to ultraviolet B radiation consuming 750-1000 ml of breast milk per day would fail to receive the 7-8.5 [micro]g of vitamin D per day needed to prevent rickets.[5] In Saudi Arabia, despite the abundance of sunshine throughout the year, vitamin D deficiency rickets has been reported among infants owing to prolonged breast feeding and voluntary avoidance of sunshine.[6]
Thus, vitamin D deficiency rickets in our patients probably resulted from a combination of factors, including maternal vitamin D deficiency leading to reduced maternofetal transfer of vitamin D during pregnancy, prolonged breast feeding by mothers deficient in vitamin D, residence in the United Kingdom (Manchester's latitude is 53 [degrees] north of the equator), and probably reduced exposure to the sun during summer months. More importantly, the infants with rickets and their mothers did not receive vitamin D supplements. The Committee on Medical Aspects of Food Policy's recommendations for vitamin D intakes for children up to 3 years of age are given in table 2.[5] The committee also recommends that children at high risk of vitamin D deficiency should be encouraged to take supplements throughout the first five years and that all pregnant and lactating mothers should receive 10 [micro]g of vitamin D daily.[5]
Historically, rickets has been associated with poverty, but clinical vitamin D deficiency occurred in the infants and spouses of three comparatively affluent and well educated overseas postgraduate students. Complacency in implementing the vitamin D supplementation policy, in our view, contributed to local resurgence of a completely preventable condition. Our cases serve to re-emphasise the importance of providing vitamin D supplements to growing children and pregnant and lactating women when their exposure to sunshine is limited, regardless of their socioeconomic status.
We thank Drs S Rimmer and S Russell for radiological assessments and Drs A Kapoor, P L Harris, and A Maw for referring three of the patients.
Funding: None.
Conflict of interest: None.
[1] Dunnigan MG, Glekin BM, Henderson lB, McIntosh WB, Sumner D, Sutherland GR. Prevention of rickets in Asian children: assessment of the Glasgow campaign. BMJ 1985;291:239-42.
[2] Clemens TL, Adams JS, Henderson SL, Holick MF. Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet 1982;i:74-6.
[3] Brooke OG, Brown IR, Cleeve HJ, Sood A. Observations on the vitamin D state of pregnant Asian women in London. Br J Obstet Gynaecol 1981;88:18-26.
[4] Specker BL, Tsang RC, Hollis BW. Effect of race and diet on human-milk vitamin D and 25-hydroxyvitamin D. Am J Dis Child 1985;139:1134-7.
[5] Department of Health. Dietary reference values for food energy and nutrients for the United Kingdom. London: HMSO, 1991. (Report on health and social subjects 41.)
[6] Eldrissy ATH, Sedrani SH, Lawson DEM. Vitamin D deficiency in mothers of rachitic infants. Calcified Tissues Int 1984;36:266-8.
(Accepted 23 April 1998)
Observing patients
The knock on the door
So much of the benefit from a medical consultation must depend on how comfortable the patient feels in the presence of the doctor, coupled, of course, with the attitude and behaviour of that doctor.
Throughout my 27 years of practice I have observed a physical sign, which greatly concerns and upsets me. Carrying out three busy standard medical clinics a week, this sign has hit me approximately once a month. I open the door to ask in a patient--"Hello, good morning"--I hope in a friendly and reassuring manner. As the patient walks in they knock on the door--they knock on the door that I am holding open for them. Why? I can only assume they in some way feel inferior, out of place, or uneasy. I want to shout--"please, you do not have to do that"--but as yet have not done so.
Perhaps they feel better for it, but not me. I have not measured or audited this phenomenon but my strong impression is that these are older patients, often from the east side of our city. Surely this must be telling us something of which we should be aware when thinking about our consultation technique. Colleagues to whom I have mentioned this phenomenon tell me that they have never noticed this. I wonder if any readers have made a similar observation?
John Ward, physician, Sheffield
We welcome articles up to 600 words on topics such as A memorable patient, A paper that changed my practice, My most unfortunate mistake, or any other piece conveying instruction, pathos, or humour. If possible the article should be supplied on a disk. Permission is needed from the patient or a relative if an identifiable patient is referred to. We also welcome contributions for "Endpieces" consisting of quotations of up to 80 words (but most are considerably shorter) from any source, ancient or modern, which have appealed to the reader.
Editorial by Wharton Papers p 28
St Mary'g Hospital, Central Manchester Healthcare Trust, Manchester M13 0JH
M Z Mughal, consultant paediatrician
H Salama, specialist registrar in paediatrics
I Laing, consultant biochemist
Alexandra Practice, Manchester M16 8NG
T Greenaway, general practitioner
University Department of Medicine, Manchester Royal Infirmary, Manchester M13 9WL
E B Mawer, professor of bone and mineral metabolism
Correspondence to: Dr Mughal mmughal@fs1.cmhct. nwest.nhs.uk
BMJ 1999;318:39-40
COPYRIGHT 1999 British Medical Association
COPYRIGHT 2000 Gale Group