Study objective: To determine whether adding IV theophylline to an aggressive regimen of inhaled and IV [Beta]-agonists, inhaled ipratropium, and IV methylprednisolone would enhance the recovery of children with severe status asthmaticus admitted to the pediatric ICU (PICU).
Design: A prospective, randomized, controlled trial. Asthma soaring was performed by investigators not involved in treatment decisions and blinded to group assignment.
Setting: The PICU of an urban, university-affiliated, tertiary-care children's hospital.
Patients: Children with a diagnosis of status asthmaticus who were admitted to the PICU for [is less than or equal to] 2 h and who were in severe distress, as indicated by a modified Wood-Downes clinical asthma score (CAS) of [is greater than or equal to] 5.
Interventions: All subjects initially received continuous albuterol nebulizations; intermittent, inhaled ipratropium; and IV methylprednisolone. The theophylline group was also administered infusions of IV theophylline to achieve serum concentrations of 12 to 17 [micro]g/mL. A CAS was tabulated twice daily.
Measurements and results: Forty-seven children (median age, 8.3 years; range, 13 months to 17 years) completed the study. Twenty-three children received theophylline. The baseline CASs of both groups were similar and included three subjects receiving mechanical ventilation in each group. All subjects receiving mechanical ventilation and theophylline were intubated before drug infusion. Among the 41 subjects who were not receiving mechanical ventilation, those receiving theophylline achieved a CAS of [is less than or equal to] 3 sooner than control subjects (18.6 [+ or -] 2.7 h vs 31.1 [+ or -] 4.5 h; p [is less than] 0.05). Theophylline had no effect on the length of PICU stay or the total incidence of side effects. Subjects receiving theophylline had more emesis (p [is less than] 0.05), and control patients had more tremor (p [is less than] 0.05).
Conclusions: Theophylline safely hastened the recovery of children in severe status asthmaticus who were also receiving albuterol, ipratropium, and methylprednisolone. The role of theophylline in the management of asthmatic children in impending respiratory failure should be reexamined.
(CHEST 2001; 119:1480-1488)
Key words: aminophylline; asthma; [Beta]-agonist; children; clinical asthma store; intensive care; methylxanthines; randomized controlled trial; status asthmaticus; theophylline
Abbreviations: CAS = Wood-Downes clinical asthma score; CK = creatine kinase; ED = emergency department; [FIO.sub.2] = fraction of inspired oxygen; PICU = pediatric ICU; PRISM = pediatric risk of mortality
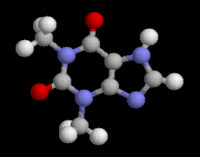
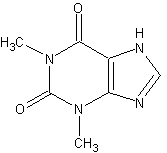
The treatment of status asthmaticus with an IV methylxanthine bronchodilator was first described in 1937 and continues to be a therapy considered for the treatment of this condition.[1,2] Methylxanthines have been associated with significant improvements in the [FEV.sub.1] and FVC during exacerbations of acute bronchial obstruction.[3,4] The methylxanthine theophylline, and its soluble ethylenediamine salt aminophylline, provide not only relaxation of bronchial smooth muscle in reactive airways but may also have salutary effects on diaphragmatic muscle function, ventilatory drive, mucociliary clearance, antidiuretic hormone secretion, and inflammation.[5-9] Although theophylline has a relatively narrow range of therapeutic concentrations, the drug can be administered safely with appropriate consideration to dosing, serum concentrations, concurrent illness and medications, and side effects.[10]
In spite of their efficacy, the methylxanthines have been supplanted in acute asthma by advancements in [Beta]-adrenergic agonist therapy. The [Beta]-agonists are faster and more potent in treating acute bronchospasm.[11] Furthermore, the selectivity of newer agents for the [[Beta].sub.2] receptor has reduced the cardiotoxicity historically associated with [Beta]-agonist therapy and permitted safer continuous inhaled or IV administration.[12,13]
The benefits of combined methylxanthine and [Beta]-agonist use in severe status asthmaticus remain unclear because most studies have specifically excluded critically ill patients from the analysis. Two controlled trials in hospitalized adults showed a significant improvement in [FEV.sub.1] when a methylxanthine was added to inhaled [Beta]-agonist therapy.[14,15] A controlled emergency department (ED) study[16] also demonstrated a threefold decrease in the hospital admission rate for adult patients treated with aminophylline and [Beta]-agonists. However, similar studies[17-21] examining [FEV.sub.1], peak expiratory flow, subjective patient response, and hospital admission rate or length of stay have been unable to show any advantage of combination therapy in adults. Several studies[22-27] in hospitalized children, also excluding critically ill patients, have likewise failed to show improvements in physical examination, pulmonary function, or length of hospital stay from adding a methylxanthine to [Beta]-agonist therapy. Furthermore, concern has been raised over the increased incidence of adverse effects in patients receiving methylxanthines and the potentiation of adverse effects from combined therapy.[24,26,28,29] The most recent expert panel report[30] of the National Heart, Lung, and Blood Institute does not generally recommend methylxanthines for children with acute asthma regardless of severity.
Despite advancements in therapy for this common childhood disease, the hospitalization rate, admission severity, and the incidence of intubation, cardiopulmonary arrest, and death among children with acute asthma have risen.[31-33] The exploration of treatment strategies must therefore include the child in intensive care. For these reasons, we designed a prospective, randomized, controlled study of IV theophylline infusion in patients with severe exacerbations of asthma who required admission to the pediatric ICU (PICU). We tested the hypothesis that theophylline, when added to a regimen of cardioselective [[Beta].sub.2]-adrenergic agonist bronchodilators, inhaled ipratropium, and IV methylprednisolone, would result in accelerated clinical improvement, a shorter ICU stay, and no greater incidence of adverse effects.
MATERIALS AND METHODS
The Institutional Review Board of St. Louis University reviewed and approved this study at Cardinal Glennon Children's Hospital. Patients were enrolled after informed consent was obtained from their parents or guardians.
Patient Selection
Children were eligible for this study if they had a history of asthma (previous evaluation by a physician for recurrent wheezing) and were admitted for [is less than or equal to] 2 h to the PICU at Cardinal Glennon Children's Hospital with severe status asthmaticus. Alternative acute diagnoses were excluded by history, physical examination, and chest radiograph. Severe status asthmaticus was defined as intractable wheezing after ED treatment and a Wood-Downes clinical asthma score (CAS) of [is greater than or equal to] 5.[34,35] The CAS is frequently used for severity assessment in pediatric asthma and has been correlated with Pa[CO.sub.2], Pa[O.sub.2], respiratory rate, pulse rate, and peak expiratory flow.[36] The CAS was modified to reflect the current use of pulse oximetry in monitoring oxygenation (Table 1). Admission to the PICU was based on an inadequate response to repeated albuterol nebulizations and the judgment of the pediatric ED and critical care staff. Patients were excluded for a known allergy or hypersensitivity to any methylxanthine, [Beta]-agonist, or anticholinergic medication; a serum theophylline level [is greater than or equal to] 3 [micro]g/mL in the ED; underlying cardiovascular disease; pregnancy; or failure to obtain consent.
Treatment Protocol
Eligible patients were consecutively entered into the study and randomly assigned to control or experimental groups by means of a computer-generated random number series (StatView 4.51; Abacus Concepts; Berkeley, CA). Individual assignments were kept within sealed and numbered envelopes until a patient was enrolled. Treatment decisions were made by the PICU attending and resident team, all of whom were aware of the subject's group assignment. CAS evaluations were performed by separate physician investigators blinded to group assignment. A written protocol promoted uniformity in dosing and titration of medications.
Subjects in both groups were administered [Beta]-agonists, inhaled ipratropium, and IV methylprednisolone. All were started on a continuous nebulization of albuterol sulfate (Glaxo Wellcome; Research Triangle Park, NC) of at least 0.3 mg/kg/h through a small volume nebulizer (Airlife; Baxter Healthcare; Valencia, CA) at 7 to 8 L/min and titrated by the PICU team. Subjects who demonstrated a rising [PCO.sub.2] or worsening respiratory distress despite upwards titration of albuterol were loaded with 10 [micro]g/kg of IV terbutaline sulfate (Ciba-Geigy; Summit, NJ) and begun on an infusion at 0.4 [micro]g/kg/min. Terbutaline infusions were titrated upwards every 10 to 15 min to achieve the desired effect. Nebulized ipratropium bromide (Dey Laboratories; Napa Valley, CA) was used primarily during the first 48 h of hospitalization and dosed at 250 to 500 [micro]g q6h. Methylprednisolone sodium succinate (Upjohn; Kalamazoo, MI) was administered as a loading dose of 2 to 4 mg/kg, then 0.5 to 1.0 mg/kg/dose q6h until discharge from the ICU.
In addition to the above therapy, subjects in the experimental group were loaded with theophylline administered as a 7 mg/kg IV bolus of aminophylline (American Regent Laboratories; Shirley, NY). Infusion of premixed theophylline in 5% dextrose (Abbott Laboratories; North Chicago, IL) followed at rates adjusted for age (6 to 12 months, 0.5 mg/kg/h; 1 to 9 years, 0.8 mg/kg/h; [is greater than or equal to] 10 years, 0.65 mg/kg/h). Theophylline levels were drawn 1 to 2 h and 8 to 12 h after the bolus as well as daily. Levels between 12 [micro]g/mL and 17 [micro]g/mL were considered acceptable.
Nonpharmacologic care for all subjects included maintenance IV fluids and humidified oxygen sufficient to keep the pulse oximetry saturation [is greater than or equal to] 95%. Baseline laboratories on admission to the PICU included a blood gas, serum potassium and glucose, and total creatine kinase (CK) with fractionated isoenzymes. Hypokalemia was indicated by a potassium level [is less than] 3.5 mEq/L, and hyperglycemia by a glucose level [is greater than] 120 mg/dL. Blood gases (either arterial or capillary) were repeated as needed, potassium and glucose were repeated every 12 h for the first 48 h, and CK with isoenzymes was repeated daily for the first 2 days in the PICU. Pediatric risk of mortality (PRISM) scores were calculated on all subjects as a general measure of illness severity at the time of admission.[37]
Outcome Variables
Response to therapy was determined primarily by changes in the subject's clinical asthma score. Specifically, we examined the time to reach a CAS of [is less than or equal to] 3 that correlates well in our institution with an intensity of care safely managed outside of the PICU. A secondary measure was the time required to meet predetermined criteria for discharge from the PICU. These criteria included the discontinuation of IV terbutaline, the administration of [Beta]-agonist inhalations no more frequently than every 2 h; and an fraction of inspired oxygen ([FIO.sub.2]) of [is less than or equal to] 0.5. Evaluations were performed twice daily (8 to 9 AM and 4 to 5 PM) throughout a subject's PICU admission by one of four investigators familiar with the CAS scoring system and blinded to the subject's group assignment. With few exceptions, the entire PICU stay for a subject was scored by the same investigator. Collection of asthma scores was suspended during mechanical ventilation and resumed on extubation. Scorers also queried subjects and their nurses for recent headaches, abdominal pain, nausea, emesis, tremor, agitation, and seizure activity. Vital signs were collected for each scoring interval after discharge from the PICU.
Statistics
Independent t tests and Fisher's Exact Tests were used to compare sets of continuous and nominal data respectively. A [chi square] analysis was used to examine any group differences in the time of admission (shift), and a Kaplan-Meier analysis incorporating the log-rank test was used to compare the rate of recovery in treatment and control subjects. Data are displayed as the mean [+ or -] 1 SEM unless otherwise specified. Results were considered significant at p [is less than or equal to] 0.05.
RESULTS
Patient Characteristics
Patients were enrolled in the study from October 1995 through January 2000. During this period, 4,520 patients were admitted to the PICU, including 320 in status asthmaticus. Forty-seven children in severe status asthmaticus, representing 49 separate admissions to the PICU, qualified and were enrolled in the study. Enrolled subjects ranged in age from 13 months to 17 years of age. One patient was enrolled on three occasions (two theophylline and one control assignment). Two other children were withdrawn, one because of parental concerns over repeated blood sampling and the other to uncertainty, regarding the diagnosis of asthma. Subjects were randomized to receive a theophylline infusion during 23 of the resulting 47 PICU admissions. There were no significant differences between the theophylline and control groups with respect to age, sex, race, home medications, past use of hospital resources, origin (ED vs the ward), ED treatment, or time of admission (Table 2). The respiratory rate, pH, [PCO.sub.2], CAS, and PRISM scores of the two groups were also not different. Six subjects required mechanical ventilation. Three were intubated before enrollment and three after randomization. Hypercarbia necessitated intubation in four subjects, and a decline in mental function with rising metabolic acidosis in the remaining two.
Theophylline Levels
Loading doses were complete within 2.1 [+ or -] 0.2 h from the time of arrival in the PICU. Initial theophylline levels were 11.2 [+ or -] 0.4 [micro]g/mL, with the subsequent infusion achieving levels of 12.5 [+ or -] 1.2 [micro]g/mL at 8 to 12 h and an average daily level of 14.5 [+ or -] 0.7 [micro]g/mL.
Recovery Time and Clinical Course
Theophylline was associated with a significant decrease in the time to reach a CAS [is less than or equal to] 3 among the 41 subjects who were not receiving mechanical ventilation (Table 3). Figure 1 shows the difference between the treatment and the control groups using a Kaplan-Meier cumulative event plot (p [is less than] 0.05). The respiratory rates of these subjects also fell during recovery and are displayed as the percentage change from baseline of observations pooled at 12-h intervals (Fig 2). Subjects receiving theophylline showed a greater percentage reduction in respiratory rate than control subjects during the first 12 h of PICU admission (p [is less than] 0.05). Theophylline did not significantly influence the time to meet PICU discharge criteria among patients not receiving mechanical ventilation.
[ILLUSTRATIONS OMITTED]
The use of mechanical ventilation in six subjects was equally distributed between the two groups. However, the three control group subjects were intubated 6 to 12 h after enrollment, as opposed to the three theophylline subjects who were intubated before receiving the drug. Although few in number, patients receiving mechanical ventilation and theophylline required less time to reach a CAS of [is less than or equal to] 3 and required less time to meet discharge criteria than did control subjects receiving mechanical ventilation (p [is less than] 0.05).
Resource Utilization
The mean length of stay in the PICU or the hospital was not altered by treatment in subjects not receiving mechanical ventilation (Table 4). However, the PICU stay of subjects receiving mechanical ventilation and theophylline was reduced (p [is less than] 0.05). Post hoc analysis did not suggest an influence of theophylline on the use or dose of continuous inhaled albuterol or IV terbutaline.
Side Effects
Data on serum CK concentrations were available for 37 admissions (79%). Total CK concentrations ranged from 33 to 6,984 U/L and were not related to treatment group. One child receiving mechanical ventilation in each group, also receiving neuromuscular blockade, developed rhabdomyolysis with CK levels [is greater than] 6,000 U/L. In both cases, the patients recovered. One subject in the theophylline group and three in the control group had an elevation in the MB isoenzyme fraction during their first 48 h of PICU admission that ranged from 5 to 7%. All of these subjects received terbutaline infusions in addition to continuous albuterol. However, there were 14 patients who were administered terbutaline and had no isoenzyme elevation. No patient in the study developed a clinically significant dysrhythmia.
Hypokalemia and hyperglycemia were common findings, occurring in 64% and 100% of subjects, respectively. There was no association between the use of theophylline and the occurrence or magnitude of either laboratory abnormality.
Side effects were frequently noted among the 41 patients who were neither intubated nor receiving sedation (Table 5). More than 85% of all subjects had one or more complaints or apparent sign of distress. There was no statistically significant difference detected in the frequency of headache, abdominal pain, nausea, or agitation between the two treatment groups. An increased incidence of emesis was observed in the group treated with theophylline (p [is less than] 0.05), and tremor was significantly greater among subjects in the control group (p [is less than] 0.05).
DISCUSSION
This is the first prospective, randomized, controlled trial of IV theophylline limited to children admitted to the PICU and receiving standard [Beta]-agonist, anticholinergic, and steroid therapy for severe status asthmaticus. We found that theophylline hastened the improvement of our nonintubated patients and shortened their observed recovery time from 31.1 [+ or -] 4.5 to 18.6 [+ or -] 2.7 h. Theophylline was associated with a greater fall in baseline respiratory rate than was seen in control subjects, particularly within the first 12 h of admission. The greatest benefit of theophylline may have been seen in the small number of subjects receiving mechanical ventilation who recovered faster and had a shorter PICU stay than intubated control subjects (3.9 [+ or -] 0.3 days vs 8.8 [+ or -] 1.5 days, respectively).
The favorable response of our patients to theophylline differs from most pediatric reports on combination therapy in less-severe acute asthma. Carter et al[23] and Strauss et al[24] performed serial measurements of [FEV.sub.1] and peak expiratory flow on children hospitalized for asthma and saw no beneficial effect from adding aminophylline to inhaled albuterol and methylprednisolone. Others have been unable to show that adding a methylxanthine to conventional therapy reduced the subject's requirement for albuterol,[22-24,26,27] supplemental oxygen,[22,26] or hospitalization.[23,25] Furthermore, controlled studies incorporating a variety of clinical scoring tools for gauging asthma severity have been unable to document an influence of methylxanthines on the rate of improvement or time to achieve a predetermined severity score.[22,23,25-27] However, the generalization of these results to severe status asthmaticus has been limited by the exclusion of patients who could not perform standard pulmonary function testing,[23] had a [PCO.sub.2] [is greater than] 50 mm Hg,[23] scored [is greater than] 5 on the CAS,[24] failed to improve within 6 h,[23,27] or required PICU admission.[22,24-26]
Yung and South[38] conducted a large, randomized, controlled trial of combination therapy in children with severe, acute asthma that, for the first time, was inclusive of patients who were poorly responsive to [Beta]-agonists, in impending respiratory failure, or admitted to the PICU. They noted the addition of aminophylline to frequently inhaled [Beta]-agonists, ipratropium, and IV steroids significantly improved the spirometry of patients and reduced their requirements for IV [Beta]-agonists and oxygen. Asthma severity scores at 6 h into the study were also improved by aminophylline. Although the majority of patients in this study did not require intensive care or continuously inhaled [Beta]-agonists, there was a measurable benefit from methylxanthine therapy not seen in earlier studies of healthier children.
The possibility that combined therapy with theophylline has an impact on critically ill asthmatics proportionate to their severity of illness is intriguing. Adult studies of acute asthma have shown that spirometric improvements through the addition of a methylxanthine are related to the degree of airway narrowing.[39,40] Combined therapy with theophylline might therefore serve to reduce the incidence of respiratory failure and mechanical ventilation in children with severe status asthmaticus and impending respiratory failure. No patient in our study or that conducted by Yung and South[38] was intubated after receiving theophylline. This compares with intubation rates among control subjects of 13% in this study and 7% in the study by Yung and South.[38] Although the faster recovery time and shorter duration of PICU stay for patients receiving mechanical ventilation and theophylline in our study is based on small numbers, a similar trend in duration of intubation, was seen by Yung and South.[38] The same authors also noted a favorable trend toward lower airway pressures among subjects receiving mechanical ventilation and theophylline. The growing number of adverse outcomes in children with asthma warrants studying these patients more closely and confirming our results in a larger study.
Although the addition of theophylline enhanced the recovery of our critically ill asthmatic children, a difference in PICU or hospital length of stay could not be demonstrated for all subjects or the majority of nonintubated patients. Less-aggressive downward titration in medications at night, delaying major treatment decisions until morning attending rounds, and preferences for daytime transfers and discharges may all limit the impact of therapeutic advances, particularly during short hospitalizations. Yung and South[38] examined the total hospital stay of their patients and were also unable to detect a significant effect from the use of theophylline.[38] Their study size was sufficient to exclude a reduction in hospital stay of [is greater than] 23% or an increase of [is greater than] 14% of the control mean (2.87 days).
Despite extensive clinical experience with the methylxanthines, their mode of action and interaction with other drugs, particularly the [Beta]-agonists, remains poorly defined. Parenteral drugs in general may circumvent the diminished delivery of aerosolized [Beta]-agonists in acute asthma[41] and young children,[42] thus augmenting submaximal bronchial smooth-muscle relaxation. Molecular mechanisms specific to theophylline that may be responsible for its beneficial effect include phosphodiesterase enzyme inhibition, adenosine receptor antagonism, enhanced catecholamine secretion, and modulation of transmembrane calcium fluxes in muscle cells.[43] The influence on calcium may be responsible for an increase in respiratory muscle contractility and resistance to diaphragmatic fatigue particularly advantageous in asthmatics with early respiratory failure. Methylxanthines may also assume greater importance during [Beta]-receptor desensitization where the response to [Beta]-agonist drugs is attenuated but a response to aminophylline persists.[44] Clinical trials involving submaximal bronchodilation have shown that the benefit from combinations of methylxanthines and [Beta]-agonists are more likely additive and not synergistic.[45]
Adverse effects of therapy were common in our study, but the total frequency of these laboratory abnormalities and symptoms did not differ between groups. Furthermore, despite theoretical concerns to the contrary, we saw no evidence for an additive cardiotoxic effect of combination therapy. The high rate of adverse effects in all patients, particularly hyperglycemia, may be related to the stress response associated with severe status asthmaticus and additive effects from [Beta]-agonist and steroid therapies. The increased incidence of nausea and vomiting with methylxanthines is well known and has been reported by others[24,26,38] studying status asthmaticus. However, the decreased incidence of tremor among theophylline patients was an unexpected finding and was contrary to previous controlled studies.[14,16-18,21-23,38] Theophylline administered long-term has been used to treat pathologic tremor disorders and may influence the incidence of tremor through modulation of adenosine activity in the brain.[46] Whether this mechanism or some other methylxanthine-related interaction was involved in attenuating tremor in our study is speculative.
Our study design had limitations that could have influenced the results. Stratifying the patients by age or excluding younger children might have improved our diagnostic accuracy and eliminated some subjects with asthma difficult to objectively document. However, we believed their inclusion was warranted by the number of these young patients in the PICU and their potential to derive the greatest benefit from small improvements in airway caliber and function. We also recognize that not blinding the PICU medical team to the study assignment of enrolled subjects could have influenced important pharmaceutical, interventional (including intubation), and discharge decisions. Our intent was to maximize the safety of studying this controversial drug at a time and in an environment where other effective therapies were available. This decision was balanced by the use of a blinded observer to assess the CAS and any adverse effects.
Contrary to published guidelines,[30] our study suggests that critically ill children with severe status asthmaticus will benefit from the addition of theophylline infusion to [Beta]-agonist, anticholinergic, and corticosteroid therapies. However, IV theophylline should only be used by clinicians experienced in dosing and adjusting infusions of this medication. Physicians must weigh the benefits of therapy in an individual patient against the increased likelihood of emesis and other potential complications. Future studies might examine the administration of theophylline to select patients in the ED unresponsive to conventional therapy, or in those patients known to be at highest risk for respiratory failure. Earlier intervention may increase the impact of methylxanthine therapy on length of stay and incidence of respiratory failure requiring mechanical ventilation. Finally, we concur with the recent efforts of the US Food and Drug Administration to encourage greater drug testing in diverse populations, such as in children and the critically ill, whose pathophysiology may be distinct enough as to derive benefit from a therapy generally considered ineffective in subjects with milder disease.
ACKNOWLEDGMENT: The authors express appreciation to the ED attending, pediatric housestaff, PICU nurses, and respiratory therapists for their assistance. We are grateful to Doris Rubio, PhD, for her statistical consultation. A special thanks to Drs. James Kemp and Blakeslee Noyes for their review of the article.
REFERENCES
[1] Herrmann G, Aynesworth MB. Successful treatment of persistent extreme dyspnea "status asthmaticus": use of theophylline ethylene diamine (aminophylline, U.S.P.) intravenously. J Lab Clin Med 1937; 23:135-148
[2] Gluckman TJ, Corbridge T. Management of respiratory failure in patients with asthma. Curr Opin Pulm Med 2000; 6:79-85
[3] Pierson WE, Bierman CW, Stamm SJ, et al. Double-blind trial of aminophylline in status asthmaticus. Pediatrics 1971; 48:642-646
[4] Vozeh S, Kewitz G, Perruchoud A, et al. Theophylline serum concentration and therapeutic effect in severe acute bronchial obstruction: the optimal use of intravenously administered aminophylline. Am Rev Respir Dis 1982; 125:181-184
[5] Murciano D, Aubier M, Lecocquic Y, et al. Effects of theophylline on diaphragmatic strength and fatigue in patients with chronic obstructive pulmonary disease. N Engl J Med 1984; 311:349-353
[6] Easton PA, Anthonisen NR. Ventilatory response to sustained hypoxia after pretreatment with aminophylline. J Appl Physiol 1988; 64:1445-1450
[7] Cotromanes E, Gerrity TR, Garrard CS, et al. Aerosol penetration and mucociliary transport in the healthy human lung: effect of low serum theophylline levels. Chest 1985; 88:194-200
[8] Iikura Y, Odajima Y, Akazawa A, et al. Antidiuretic hormone in acute asthma in children: effects of medication on serum levels and clinical course. Allergy Proc 1989; 10:197-201
[9] Sullivan P, Bekir S, Jaffar Z, et al. Anti-inflammatory effects of low-dose oral theophylline in atopic asthma. Lancet 1994; 343:1006-1008
[10] Hendeles L, Weinberger M, Szefler S, et al. Safety and efficacy of theophylline in children with asthma. J Pediatr 1992; 120:177-183
[11] Rossing TH, Fanta CH, Goldstein DH, et al. Emergency therapy of asthma: comparison of the acute effects of parenteral and inhaled sympathomimetics and infused aminophylline. Am Rev Respir Dis 1980; 122:365-371
[12] Katz RW, Kelly W, Crowley MR, et al. Safety of continuous nebulized albuterol for bronchospasm in infants and children. Pediatrics 1993; 92:666-669
[13] Stephanopoulos DE, Monge R, Schell KH, et al. Continuous intravenous terbutaline for pediatric status asthmaticus. Crit Care Med 1998; 26:1744-1748
[14] Huang D, O'Brien RG, Harmon E, et al. Does aminophylline benefit adults admitted to the hospital for an acute exacerbation of asthma? Ann Intern Med 1993; 119:1155-1160
[15] Montserrat JM, Barbera JA, Viegas C, et al. Gas exchange response to intravenous aminophylline in patients with a severe exacerbation of asthma. Eur Respir J 1995; 8:28-33
[16] Wrenn K, Slovis CM, Murphy F, et al. Aminophylline therapy for acute bronchospastic disease in the emergency room. Ann Intern Med 1991; 115:241-247
[17] Siegel D, Sheppard D, Gelb A, et al. Aminophylline increases the toxicity but not the efficacy of an inhaled [Beta]-adrenergic agonist in the treatment of acute exacerbations of asthma. Am Rev Respir Dis 1985; 132:283-286
[18] Self TH, Abou-Shala N, Burns R, et al. Inhaled albuterol and oral prednisone therapy in hospitalized adult asthmatics: does aminophylline add any benefit? Chest 1990; 98:1317-1321
[19] Murphy DG, McDermott MF, Rydman RJ, et al. Aminophylline in the treatment of acute asthma when [[Beta].sub.2]-adrenergics and steroids are provided. Arch Intern Med 1993; 153:1784-1788
[20] Zainudin BMZ, Ismail O, Yusoff K. Effect, of adding aminophylline infusion to nebulised salbutamol in severe acute asthma. Thorax 1994; 49:267-269
[21] Rodrigo C, Rodrigo G. Treatment of acute asthma: lack of therapeutic benefit and increase of the toxicity from aminophylline given in addition to high doses of salbutamol by metered-dose inhaler with a spacer. Chest 1994; 106:1071-1076
[22] Digiulio GA, Kercsmar CM, Krug SE, et al. Hospital treatment of asthma: lack of benefit from theophylline given in addition to nebulized albuterol and intravenously administered corticosteroid. J Pediatr 1993; 122:464-469
[23] Carter E, Cruz M, Chesrown S, et al. Efficacy of intravenously theophylline in children hospitalized with severe asthma. J Pediatr 1993; 122:470-476
[24] Strauss RE, Wertheim DL, Bonagura VR, et al. Aminophylline therapy does improve outcome and increases adverse effects in children hospitalized with acute asthmatic exacerbations. Pediatrics 1994; 93:205-210
[25] Needleman JP, Kaifer MC, Nold JT, et al. Theophylline does not shorten hospital stay for children admitted for asthma. Arch Pediatr Adolesc Med 1995; 149:206-209
[26] Bien JP, Bloom MD, Evans RL, et al. Intravenous theophylline in pediatric status asthmaticus: a prospective, randomized, double-blind, placebo-controlled trial. Clin Pediatr 1995; 34:475-481
[27] Nuhoglu Y, Dai A, Barlan I, et al. Efficacy of aminophylline in the treatment of acute asthma exacerbation in children. Ann Allergy Asthma Immunol 1998; 80:395-398
[28] Joseph X, Whitehurst VE, Bloom S, et al. Enhancement of cardiotoxic effects of [Beta]-adrenergic bronchodilators by aminophylline in experimental animals. Fundam Appl Toxicol 1981; 1:443-447
[29] Nicklas RA, Balazs T. Adverse effects of theophylline-[Beta] agonist interactions. J Allergy Clin Immunol 1986; 78:806-811
[30] National Asthma Education and Prevention Program. Expert panel report 2: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Institutes of Health, 1997; Publication No. 051; 115-117
[31] Newacheck PW, Halfon N. Prevalence, impact, and trends in childhood disability because of asthma. Arch Pediatr Adolesc Med 2000; 154:287-293
[32] Centers for Disease Control and Prevention. Asthma mortality and hospitalization among children and young adults--United States, 1980-1993. MMWR Morb Mortal Wkly Rep 1996; 45:350-353
[33] Calmes D, Leake BD, Carlisle DM. Adverse asthma outcomes among children hospitalized with asthma in California. Pediatrics 1998; 101:845-850
[34] Wood DW, Downes JJ, Lecks HI. A clinical scoring system for the diagnosis of respiratory failure. Am J Dis Child 1972; 123:227-228
[35] Papo MC, Frank J, Thompson AE. A prospective, randomized study of continuous versus intermittent nebulized albuterol for severe status asthmaticus in children. Crit Care Med 1993; 21:1479-1486
[36] Van Der Windt DA, Nagelkerke AF, Bouter LM, et al. Clinical scores for acute asthma in pre-school children: a review of the literature. J Clin Epidemiol 1994; 47:635-646
[37] Pollack MM, Ruttimann UE, Getson PR. Pediatric risk of mortality (PRISM) score. Crit Care Med 1988; 16:1110-1116
[38] Yung M, South M. Randomised controlled trial of aminophylline for severe acute asthma. Arch Dis Child 1998; 79:405-410
[39] Rossing TH, Fanta CH, MacFadden ER. A controlled trial of the use of single versus combined drug therapy in the treatment of acute episodes of asthma. Am Rev Respir Dis 1981; 123:190-194
[40] Fanta CH, Rossing TH, McFadden ER. Treatment of acute asthma: is combination therapy with sympathomimetics and methylxanthines indicated? Am J Med 1986; 80:5-10
[41] Lipworth BJ, Clark DJ. Effects of airway calibre on lung delivery of nebulized salbutamol. Thorax 1997; 52:1036-1039
[42] Penna AC, Dawson KP, Manglick P, et al. Systemic absorption of salbutamol after nebulizer delivery in acute asthma. Acta Paediatr 1993; 82:963-966
[43] Vassallo R, Lipsky JJ. Theophylline: recent advances in the understanding of its mode of action and uses in clinical practice. Mayo Clin Proc 1998; 73:346-354
[44] Avner BP, Noland B. In vivo desensitization to [Beta] receptor mediated bronchodilator drugs in the rat: decreased [Beta] receptor affinity. J Pharmacol Exp Ther 1978; 207:23-33
[45] Handslip PDJ, Dart AM, Davies BH. Intravenous salbutamol and aminophylline in asthma: a search for synergy. Thorax 1981; 36:741-744
[46] Mally J, Stone T. Potential role of adenosine antagonist therapy in pathological tremor disorders. Pharmacol Ther 1996; 72:243-250
(*) From the Divisions of Critical Care (Drs. Ream, Loftis, Lynch, and Mink), Pulmonology (Dr. Albers), and Allergy and Immunology (Dr. Becker), Department of Pediatrics, Saint Louis University and the Cardinal Glennon Pediatric Research Institute, St. Louis, MO.
Supported by Cardinal Glennon Children's Hospital.
This study was presented, in part, at the 27th Educational and Scientific Symposium of the Society of Critical Care Medicine, San Antonio, TX, February 4-8, 1998.
Manuscript received April 17, 2000; revision accepted September 6, 2000.
Correspondence to: Robert S. Ream, MD, Department of Pediatrics, Saint Louis University, Cardinal Glennon Children's Hospital, 1465 South Grand Blvd, St. Louis, MO 63104; e-mail: reamrs@slu.edu
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group