Background: [[Beta].sub.2]-Agonists and corticosteroids or theophylline can interact to produce beneficial effects on airway function in asthma, but this has not been established in COPD.
Methods: Eighty patients with well-controlled COPD were randomized to receive 3 months of treatment in one of four treatment groups: (1) salmeterol, 50 [micro]g bid; (2) salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid; (3) salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid; and(4) salmeterol, 50 [micro]g, plus titrated theophylline bid. At each visit, a dose-response curve to inhaled salbutamol was constructed using a total cumulative dose of 800 [micro]g.
Results: A gradual increase in FEV1 was observed with each of the four treatments. Maximum significant increases in [FEV.sub.1] over baseline values that were observed after 3 months of treatment were as follows: salmeterol, 50 [micro]g bid, 0.163 L (95% confidence interval [CI], 0.080 to 0.245 L); salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid, 0.188 L (95% CI, 0.089 to 0.287 L); salmeterol, 50 [micro]g, plus fiuticasone propionate, 500 [micro]g bid, 0.239 L (95% CI, 0.183 to 0.296 L); and salmeterol, 50 [micro]g, plus titrated theophylline bid, 0.157 L (95% CI, 0.027 to 0.288 L). Salbutamol always caused a significant dose-dependent increase in FEV1 (p [is less than] 0.001), although the 800-[micro]g dose never induced further significant benefit when compared with the 400- [micro]g dose. The mean differences between the highest salbutamol FEV1 after salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid, and that after salmeterol, 50 [micro]g, plus titrated theophylline bid or salmeterol, 50 [micro]g bid, were statistically significant (p [is less than] 0.05).
Conclusion: These data show that both long-acting [[Beta].sub.2] - agonists and inhaled corticosteroids have a role in COPD. The data also show that fluticasone propionate and salmeterol given together are more effective than salmeterol alone. Moreover, it suggests that the addition of fluticasone propionate to salmeterol allows a greater improvement in lung function after salbutamol, although regular salmeterol is able to improve lung function in COPD patients without development of a true subsensitivity to its bronchodilator effect. In any case, patients must be treated for at least 3 months before a real improvement in lung function is achieved.
(CHEST 2000; 118:1576-1581)
Key words: COPD; fluticasone propionate; salbutamol; salmeterol; theophylline; tolerance
Abbreviations: CI = confidence interval; MDI = metered-dose inhaler
Although originally designed for the treatment of bronchial asthma, use of long-acting [[Beta].sub.2]-agonist bronchodilators is about to become a leading therapeutic approach in COPD. [1,2] In fact, several clinical studies have documented that the protracted treatment of COPD with these agents can induce an improvement in respiratory function.[3,4]
Unfortunately, there is evidence for downregulation of [[Beta].sub.2]-adrenoceptor protein and messenger RNA after selective long-acting [[Beta].sub.2]-adrenoceptor agonist treatment in human lung,[5] and this may limit their therapeutic efficacy in obstructive airways disease.
The changes induced in [[Beta].sub.2] - receptors by exposure to [[Beta].sub.2] - agonists may be attenuated or reversed by the addition of corticosteroids. [6] In effect, [[Beta].sub.2]-agonists can interact with corticosteroids to produce beneficial effects on airway function in asthma,[6] but this has not been established in COPD. In particular, the efficacy of inhaled corticosteroids in the treatment of COPD remains controversial.[7] Obviously, also the impact of long-acting [[Beta].sub.2]-agonists on combinations with corticosteroids is still unclear.
The present study aimed to investigate the potential additive effect of two different doses of inhaled fluticasone propionate in patients with stable COPD who received inhaled salmeterol, 50 [micro]g bid, administered with a metered-dose inhaler (MDI). Moreover, we examined the effectiveness of fluticasone for preventing the development of subsensitivity to bronchodilator effects of salbutamol after regular inhaled salmeterol. We also asked the question whether the addition of theophylline to treatment with long-acting [[Beta].sub.2]-agonists could be justified. In fact, theophylline, which has anti-inflammatory properties, could also provide adequate bronchodilation when used in combination with [[Beta].sub.2]-agonists and prevent the development of tolerance to the bronchoprotective effect of salmeterol.[8] It has yet to be tested whether the association of a long-acting [[Beta].sub.2]-agonist with theophylline induces an increase in the bronchodilator effect caused by either of the two drugs.
MATERIALS AND METHODS
Eighty patients with well-controlled COPD (our definition of COPD was consistent with the criteria proposed by the American Thoracic Society),[9] who had previously been individually dose titrated with slow-release theophylline to a serum theophylline level of 10 to 20 [micro]g/mL, were recruited. Inclusion criteria were as follows: [is greater than] 50 years old with at least a 20-year smoking history; a change in [FEV.sub.1] [is less than or equal to]12% as a percent of the predicted normal value following salbutamol, 400 [micro]g; postbronchodilator [FEV.sub.1] [is less than] 85%; and good MDI technique. Exclusion criteria were as follows: current evidence of asthma as primary diagnosis; unstable respiratory disease requiring oral/parenteral corticosteroids within 4 weeks prior to beginning the study; upper or lower respiratory tract infection within 4 weeks of the screening visit; unstable angina or unstable arrhythmias; concurrent use of medications that affected COPD or interacted with methylxanthine products, such as macrolides or fluroquinolones; and evidence of alcohol abuse. Table 1 outlines some characteristics and the smoking history of the population studied.
Table 1--Anthropometric Data and Smoking History(*)
(*) Data are presented as mean (95% CI) unless otherwise indicated. M = male; F = female.
Patients entered a 2-week run-in period during which their regular treatment for COPD was stopped and they received salbutamol as required. They were then randomized to receive 3 months of treatment in one of four treatment groups: (1) salmeterol, 50 [micro]g bid; (2) salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid; (3) salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid; and (4) salmeterol, 50 [micro]g, plus titrated theophylline bid, after giving their informed consent. Salmeterol and fluticasone were administered from an MDI and holding chamber (AeroChamber; Trudell Medical International; London, Ontario, Canada) with mouthpiece.
At each visit, three [FEV.sub.1] and FVC measurements were taken, and the highest of each was recorded. Spirometric testing was performed according to the procedures described in the American Thoracic Society 1987 update.[10] These measurements were performed on the morning of each visit, before any drug had been taken. Soon after, a dose-response curve to inhaled salbutamol was constructed using doses of 100, 100, 200, and 400 [micro]g from an MDI with spacer and mouthpiece, for a total cumulative dose of 800 [micro]g salbutamol. Doses were given at 20-min intervals, and the measurements were made 15 min after each dose.
Serum theophylline levels in patients receiving salmeterol, 50 [micro]g, plus titrated theophylline bid were measured monthly during the 3-month treatment period. Adverse events were collected through nonspecific questioning or direct observation by investigators at each clinic visit and through spontaneous reports by patients.
In order to qualify for efficacy analysis, the patient had to complete the 3-month treatment period. The predose-response curve to the salbutamol [FEV.sub.1] value was chosen as the primary outcome variable. Analysis of spirometric data for each treatment was performed using the Student's t test for paired variables. Mean responses were also compared by multifactorial analysis of variance to establish any significant overall effect among all four treatments. In the presence of a significant overall analysis of variance, Duncan's multiple range testing with 95% confidence limits was used to identify where differences were significant. A probability level of p [is less than] 0.05 was considered as being of significance for all tests.
RESULTS
All patients who enter the run-in period were randomized to treatment in blocks of four according to a list of randomized codes; of these, 69 patients completed the 3-month treatment period: 18 patients receiving salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid; 18 patients receiving salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid; 16 patients receiving salmeterol, 50 [micro]g, plus titrated theophylline bid; and 17 patients receiving salmeterol, 50 [micro]g bid. Patients were withdrawn for various reasons, the most common of which were poor compliance with the protocol, exacerbation, and tachycardia.
There were no significant differences among the baseline spirometric values of the four treatment groups ([FEV.sub.1], p [is greater than] 0.05).
A gradual increase in [FEV.sub.1] was observed with each of the four treatments (Fig 1). Maximum significant (p [is less than] 0.05) increases in [FEV.sub.1] over baseline values that were observed after 3 months of treatment were as follows: salmeterol, 50 [micro]g bid, 0.163 L (95% confidence interval [CI], 0.080 to 0.245 L); salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid, 0.188 L (95% CI, 0.089 to 0.287 L); salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid, 0.239 L (95% CI, 0.183 to 0.296 L); and salmeterol, 50 [micro]g, plus titrated theophylline bid, 0.157 L (95% CI, 0.027 to 0.288). However, the mean differences between the highest [FEV.sub.1] after salmeterol, 50 [micro]g bid, treatment and that after salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid (- 0.011 L; 95% CI, - 0.327 to 0.306 L), salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid (- 0.031 L; 95% CI, - 0.320 to 0.257 L), or salmeterol, 50 [micro]g, plus titrated theophylline bid (- 0.071 L; 95% CI, - 0321 to 0.208 L) were not statistically significant (p [is greater than] 0.05).
[Figure 1 ILLUSTRATION OMITTED]
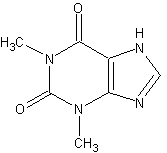
Salbutamol always caused a significant dose-dependent increase in [FEV.sub.1] (p [is less than] 0.001), although the 800-[micro]g dose never induced further significant benefit (p [is greater than] 0.05) when compared with 400-[micro]g dose (Fig 2). After 3 months, the mean maximum increase in [FEV.sub.1] over presalbutamol values induced by salbutamol, 800 [micro]g, was 0.100 L (95% CI, 0.0048 to 0.152 L) in the group receiving salmeterol, 50 [micro]g bid; 0.188 L (95% CI, 0.089 to 0.287 L) in the group receiving salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid; 0.232 L (95% CI, 0.163 to 0.30 L) in the group receiving salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid; and 0.138 L (95% CI, 0.034 to 0.233 L) in the group receiving salmeterol, 50 [micro]g, plus titrated theophylline bid. However, only the dose-response curve for salbutamol in the group receiving salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid, was significantly different (p [is less than] 0.05) when data after 3 months of treatment were compared with those obtained after 2 months of treatment.
[Figure 2 ILLUSTRATION OMITTED]
Mean [FEV.sub.1] values after inhalation of salbutamol, 800 [micro]g, in all the four treatments were statistically different (p [is less than] 0.05) from their corresponding pretreatment levels after 3 months of treatment. After 3 months, salbutamol, 800 [micro]g, induced the highest [FEV.sub.1] improvement (0.283 L; 95% CI, 0.106 to 0.459 L) in the patients receiving salmeterol, 50 [micro]g, plus fluticasone propionate, 250 [micro]g bid, and the lowest [FEV.sub.1] improvement (0.152 L; 95% CI, 0.065 to 0.238 L) in those receiving salmeterol, 50 [micro]g bid.
Patients receiving salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid, showed the highest mean improvement in [FEV.sub.1] (0.472 L; 95% CI, 0.386 to 0.557 L) over the presalbutamol baseline (pretreatment) value; patients receiving salmeterol, 50 [micro]g bid, showed the lowest mean improvement in [FEV.sub.1] (0.263 L; 95% CI, 0.195 to 0.331 L). The mean differences between the highest salbutamol [FEV.sub.1] after salmeterol, 50 [micro]g, plus fluticasone propionate, 500 [micro]g bid, and that after salmeterol, 50 [micro]g, plus titrated theophylline bid or salmeterol, 50 [micro]g bid, were statistically significant (p [is less than] 0.05). Two patients receiving salmeterol, 50 [micro]g bid, and one patient treated with salmeterol 50 [micro]g, plus titrated theophylline bid experienced exacerbations.
DISCUSSION
The present data show that patients with COPD must be treated for at least 3 months before a real improvement in lung function is achieved. In this study, the bronchodilator effect elicited by regular treatment with salmeterol was progressive. This finding is in agreement with the results of several reports that have shown that treatment with long-acting [[Beta].sub.2]-agonists may result in an improvement in functional status, even in patients suffering from apparently nonreversible obstructive pulmonary disease.[3,4,11]
Unfortunately, there are concerns about the effectiveness of prolonged therapy with long-acting [[Beta].sub.2]-adrenoceptor agonists. In fact, in mild to moderate asthma, salmeterol appears to rapidly lose its ability to control both specific and aspecific bronchial hyperresponsiveness, while it is effective in maintaining a well-sustained bronchodilation despite a small degree of tachyphylaxis.[12,13]
The present study demonstrates that the regular treatment with salmeterol leads to significant bronchodilation and, moreover, does not interfere with the effects of standard doses of short-acting [[Beta].sub.2]-agonist in patients suffering from partially reversible COPD. This is, in our opinion, an important finding, considering that when the airway obstruction becomes more severe, the therapeutic option is to add a short-acting inhaled [[Beta].sub.2]-agonist, such as salbutamol, as rescue medication to cause rapid relief of bronchospasm.
However, the long-term treatment with formoterol and salmeterol could reduce the airways responses to repeated doses of a short-acting inhaled [[Beta].sub.2]-agonist because they are partial [[Beta].sub.2]-receptor agonists and in the presence of a full [Beta]-agonist they may act as a [[Beta].sub.2]-antagonist.[14] In fact, it has been demonstrated that asthmatic patients treated with salmeterol had reduced bronchodilator responses to salbutamol in terms of [FEV.sub.1] and peak expiratory flow rate than those treated with placebo.[15] The reduction in response equated with a 2.5-fold and a fourfold greater dose of salbutamol being required to produce a given [FEV.sub.1] and peak expiratory flow rate, respectively.
Our study confirms and extends our previous documentation that salbutamol causes additional bronchodilation when salmeterol has already caused its bronchodilatory effect in patients suffering from partially reversible COPD.[16] This is consistent with the results of Langley et al,[17] who showed that regular salmeterol usage did not lead to reduced efficacy of usual or higher-than-usual doses of salbutamol in adult patients with stable asthma. However, all patients in that study were receiving inhaled corticosteroids, while in the present study, the same effect has been observed also in COPD patients who were treated with only regular salmeterol. In any ease, Nelson et ails have documented that, irrespective of concurrent corticosteroid treatment, long-term therapy with salmeterol does not result in tolerance to the bronchodilator effects of salbutamol.
Although salmeterol was beneficial to our patients with COPD, the combination of salmeterol with fluticasone did not induce a greater bronchodilation than salmeterol alone. This finding contrasts with the documentation that asthmatic patients treated with salmeterol combined with fluticasone propionate have improvements over baseline in [FEV.sub.1] at endpoint that were at least twice as great as improvements in patients treated with salmeterol or fluticasone propionate alone.[19] Moreover, the addition of salmeterol therapy to patients who remain symptomatic while using a low dose of fluticasone propionate is clinically and statistically superior to increasing the dose of fluticasone propionate.[20] Inhaled corticosteroids and salmeterol target different aspects of the underlying disease process, and, consequently, combined therapy is frequently more effective than monotherapy.[20]
Because of the very little evidence to date on the effect of inhaled corticosteroids in COPD,[21,22] there is disagreement over corticosteroid treatment in this disease. Even the improvement in airflow limitation conferred by beclomethasone dipropionate, 3 [micro]g, when used in combination with high doses of bronchodilators was small on average.[23]
However, Paggiaro et al[24] have recently demonstrated that fluticasone propionate may be of clinical benefit in patients with COPD over at least 6 months. Moreover, Calverley et al[25] have shown that fluticasone induces higher [FEV.sub.1] compared with placebo throughout a 3-year treatment period, although it has no effect on rate of decline in [FEV.sub.1].
Thus, the type of inhaled corticosteroid may apparently have an important role in the long-term treatment of COPD. In effect, there are significant differences in the pharmacokinetics and pharmacodynamics of inhaled corticosteroids.[26] For example, long pulmonary residence time has been calculated for fluticasone propionate, but budesonide appears to disappear rapidly.[26] Moreover, budesonide and beclomethasone dipropionate show comparable antiasthma effects at equal doses, where fluticasone propionate is approximately twice as potent as either steroid.[26] These differences might be of importance in patients with COPD.
It is important to highlight that corticosteroids can prevent homologous downregulation of [[Beta].sub.2]-adrenoceptor number and induce an increase in the rate of synthesis of receptors through a process of increased [[Beta].sub.2]-adrenoceptor gene transcription.[27] Such effects may have clinical implications, not only for preventing the development of tolerance to [[Beta].sub.2]-agonists in patients treated with [Beta]-agonist bronchodilators, but, likely, also for increasing the bronchodilator response to [[Beta].sub.2]-agonists. In fact, in this study, the combination of salmeterol with fluticasone allowed a greater improvement in lung function after salbutamol than salmeterol alone.
Theophylline improves airflow, reduces pulmonary artery pressure, increases arterial oxygen tension, improves diaphragmatic strength and endurance, increases right ventricular function, and may produce anti-inflammatory effects. However, the magnitude of these changes is small, the therapeutic index is narrow, and side effects are common, even when serum theophylline levels are within the therapeutic range.[8] For these reasons, the recent British Thoracic Society guidelines for the management of COPD state that the addition of oral theophylline should be considered only if inhaled treatments have failed to provide enough benefit.[7]
Nevertheless, as the drug has been shown to have anti-inflammatory and immunomodulatory effects in patients with asthma,[8,28] it is possible that theophylline might also attenuate the airflow limitation caused by airway inflammation in COPD.[29] In any case, we must stress that regular theophylline treatment neither prevents nor worsens the development of tolerance to the bronchoprotective effect of salmeterol in vivo.[30]
A number of clinical studies support the combined use of theophylline and a [Beta]-agonist in patients with COPD.[31] In fact, Giessel et alas have recently demonstrated that the combination of salmeterol plus theophylline was significantly better in improving [FEV.sub.1] area under curve than theophylline or salmeterol alone in patients with COPD. However, our study demonstrates that the addition of theophylline to a treatment with salmeterol is not justified because there is not a true advantage on a treatment with salmeterol alone. In any case, the addition of salmeterol to fluticasone propionate seems to be better.
In conclusion, this study confirms that both long-acting [[Beta].sub.2]-agonists and inhaled corticosteroids have a role in COPD. The data also show that fluticasone propionate and salmeterol given together are more effective than salmeterol alone after a treatment period of 3 months. Moreover, it suggests that the addition of fluticasone propionate to salmeterol allows a greater improvement in lung function after salbutamol, although regular salmeterol use is able to improve lung function in COPD patients without development of a true subsensitivity to its bronchodilator effect. Therefore, the results of the present study seem to support the use of combined therapy. However, the true impact of long-acting [[Beta].sub.2]-agonists on combinations is still unclear. Regular assessment of the patient's physiologic status will determine the clinical usefulness of these drugs. Therefore, carefully designed studies with larger population are required to define their role and, possibly, to develop a new treatment algorithm for COPD.
REFERENCES
[1] Cazzola M, Spina D, Matera MG. The use of bronchodilators in stable chronic obstructive pulmonary disease. Pulm Pharmacol Ther 1997; 10:129-144
[2] Cazzola M, Matera MG. Should long-acting [[Beta].sub.2]-agonists be considered an alternative first choice option for the treatment of stable COPD? Respir Med 1999; 93:227-229
[3] Boyd G, Morice AH, Pounsford JC, et al. All evaluation of salmeterol in the treatment of chronic obstructive pulmonary disease (COPD). Eur Respir J 1997; 10:815-821
[4] Mahler DA, Donohue JF, Barbee RA, et al,. Efficacy of salmeterol xinafoate in the treatment of COPD. Chest 1999; 115:957-965
[5] Nishikawa M, Mak JC, Barnes PJ. Effect of short- and long-acting [[Beta].sub.2]-adrenoceptor agonists on pulmonary [[Beta].sub.2]-adrenoceptor expression in human lung. Eur J Pharmacol 1996; 31.8:123-129
[6] Mak JC, Nishikawa M, Shirasaki H, et al. Protective effects of a glucocorticoid on downregulation of pulmonary [[Beta].sub.2]-adrenergic receptors in vivo J Clin Invest 1995; 96:99-106
[7] BTS guidelines for the management of chronic obstructive pulmonary disease. The COPD Guidelines Group of the Standards of Care Committee of the BTS. Thorax 1997; 52(suppl 5):S1-S28
[8] Cazzola M, Donner CF, Matera MG. Long-acting [[Beta].sub.2]-agonists and theophylline in stable chronic obstructive pulmonary disease. Thorax 1999; 54:730-736
[9] American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1995; 152(suppl):S72-S120
[10] American Thoracic Society. Standardization of spirometry, 1987 update. Am Rev Respir Dis 1987; 136:1285-1298
[11] Ulrik CS. Efficacy of inhaled salmeterol in the management of smokers with chronic obstructive pulmonary disease: a single center randomised, double blind, placebo controlled, crossover study. Thorax 1995; 50:750-754
[12] Cheung D, Timmers MC, Zwinderman AH, et al. Long-term effects of a long-acting [[Beta].sub.2]-adrenoceptor agonist, salmeterol, on airway hyperresponsiveness in patients with mild asthma. N Engl J Med 1992; 327:1198-1203
[13] Dottorini ML, Tantucci C, Peccini F, et al. Diurnal change of bronchial caliber and airway responsiveness in asthmatics during long-term treatment with long-acting [[Beta].sub.2]-agonist salmeterol. Int J Clin Pharmacol Ther 1996; 34:438-443
[14] Lipworth BJ, Grove A. Evaluation of partial beta-adrenoceptor agonist activity. Br J Clin Pharmacol 1997; 43:9-14
[15] Grove A, Lipworth BJ. Bronchodilator subsensitivity to salbutamol after twice daily salmeterol in asthmatic patients. Lancet 1995; 346:201-206
[16] Cazzola M, Di Perna F, Noschese P, et al. Effects of formoterol, salmeterol or oxitropium bromide on airway responses to salbutamol in COPD. Eur Respir J 1998; 11:1337-1341
[17] Langley SJ, Masterson CM, Batty EP, et 'al. Bronchodilator response to salbutamol after chronic dosing with salmeterol or placebo. Eur Respir J 1998; 11:1081-1085
[18] Nelson HS, Berkowitz RB, Tinkelman DA, et al. Lack of subsensitivity to albuterol after treatment with salmeterol in patients with asthma. Am J Respir Crit Care Med 1999; 159:1556-1561
[19] Pearlman DS, Stricker W, Weinstein S, et al. Inhaled salmeterol and fluticasone: a study comparing monotherapy and combination therapy in asthma. Ann Allergy Asthma Immunol 1999; 82:257-265
[20] Condemi JJ, Goldstein S, Kalberg C, et al. The addition of salmeterol to fluticasone propionate versus increasing the dose of fluticasone propionate in patients with persistent asthma: Salmeterol Study Group. Ann Allergy Asthma Immunol 1999; 82:383-389
[21] Dompeling E, van Schayck CP, Molema J, et al. Inhaled beclomethasone improves the course of asthma and COPD. Eur Respir J 1992; 5:945-952
[22] Renkema TE, Schouten JP, Koeter GH, et al. Effects of long-term treatment with corticosteroids in COPD. Chest 1996; 109:1156-11.62
[23] Nishimura K, Koyama H, Ikeda A, et al. The effect of high-dose inhaled beclomethasone dipropionate in patients with stable COPD. Chest 1999; 115:31-37
[24] Paggiaro PL, Dahle R, Bakran I, et al. Multicentre randomised placebo-controlled trial (if inhaled fluticasone propionate in patients with chronic obstructive pulmonary disease: International COPD Study Group. Lancet 1998; 351:773-780
[25] Calverley PMA, Burge PS, Jones PW, et al. Effects of 3 years treatment with fluticasone propionate in patients with moderately severe COPD [abstract]. Am J Respir Crit Care Med 1999; 159:A524
[26] Derendorf H, Hochhaus G, Meibohm B, et al. Pharmacokinetics and pharmacodynamics of inhaled corticosteroids. J Allergy Clin Immunol 1998; 101(suppl):S440-S446
[27] Barnes PJ. Efficacy of inhaled corticosteroids in asthma. J Allergy Clin Immunol 1998; 102:531-538
[28] Banner KH, Page CP. Theophylline and selective phosphodiesterase inhibitors as anti-inflammatory drugs in the treatment of bronchial asthma. Eur Respir J 1995; 8:996-1000
[29] Ikeda A, Nishimura K, Izumi T. Pharmacological treatment in acute exacerbations of chronic obstructive pulmonary disease. Drugs Aging 1998; 12:129-137
[30] Cheung D, Wever AM, de Goeij JA, et al. Effects of theophylline on tolerance to the bronchoprotective actions of salmeterol in asthmatics in vivo. Am J Respir Crit Care Med 1998; 158:792-796
[31] Rennard SI. Combination bronchodilator therapy in COPD. Chest 1995; 107(suppl):171S-175S
[32] Giessel G, ZuWallack R, Cook C, et al. A comparison of Serevent and theophylline on pulmonary function in COPD patients [abstract]. Am J Respir Crit Care Med 1999; 159:A523
(*) From A. Cardarelli Hospital (Drs. Cazzola, Di Perna, and Calderaro), Division of Pneumology and Allergology and Respiratory Clinical Pharmacology Unit, Naples; University of Palermo, Institute of Internal Medicine and Geriatrics (Dr. Di Lorenzo), Palermo; GlaxoWellcome Italy (Dr. Testi), Medical Department, Verona; and University of Milan (Dr. Centanni), San Paolo Hospital, Respiratory Unit, Milan, Italy.
Dr. Cazzola has received financial support for research and attending meetings and has received roes for streaking and consulting by GlaxoWellcome Italy. Dr. Di Lorenzonas received financial support for research andhas spoken at some meetings financially supported by GlaxoWellcome Italy. Dr. Testi is employed by GlaxoWellcome Italy. Fluticasone propionate and salmeterol are manufactured by GlaxoWellcome.
Manuscript received June 17, 1999; revision accepted June 20, 2000.
Correspondence to: Marlo Cazzola, Divisione di Pneurmologia e Allergologia e Unita di Farmacologia Clinica Respiratoria, Ospedale A. Cardarelli, Via del Parco Margherita 24, 80121 Napoli, Italy; e-mail: mcazzola@qubisoft.it
COPYRIGHT 2000 American College of Chest Physicians
COPYRIGHT 2001 Gale Group