Patients with brain damage, in contrast to normal subjects, exhibit a significant ventilatory undershoot when brief hypocapnic hypoxia is terminated abruptly by hyperoxia. This has been attributed to an impairment of activation of short-term potentiation, a brain stem mechanism promoting breathing stability. We hypothesized that in these patients theophylline, a drug that stabilizes breathing, may affect short-term potentiation. Eight stable patients with brain damage and 10 normal adults were studied. Activation of short-term potentiation was examined by brief exposure to hypoxia followed by hyperoxia after pretreatment with placebo or theophylline. Both in patients and normal subjects at the end of hypoxia ventilation increased to a similar magnitude with and without theophylline. In normal subjects independent of pretreatment, when hypoxia was terminated abruptly by hyperoxia, ventilation declined slowly to baseline without an undershoot, indicating activation of short-term potentiation. In patients with placebo, ventilation upon switching to hyperoxia exhibited a significant undershoot. This undershoot was significantly attenuated by theophylline, although compared with normal subjects, a slight hypoventilation was observed. We conclude that in patients with brain damage, theophylline largely prevents the hyperoxic drop of ventilation, presumably by affecting the activation of short-term potentiation. This may underlie the beneficial effect of theophylline on breathing stability.
Keywords: periodic breathing; ventilation; hypoxia; hyperoxia
After abrupt cessation of a respiratory stimulus, respiratory output depends on the balance of excitatory and inhibitory influences, developed during the preceding hyperventilatory phase (1-3). Both inhibitory influences, mediated through mechanoreceptors and blood gasses changes, and excitatory influences mediated mainly through activation of short-term potentiation (STP) have been repeatedly demonstrated in animals and humans (1-7). The relative strength of these influences determines ventilation after withdrawal of a stimulus. In awake humans at rest or during exercise, termination of a brief period of hypocapnic hypoxia by hyperoxia resulted in poststimulus potentiation of ventilation, indicating that activation of STP during the preceding hypoxic hyperventilation overrode the inhibitory influences (4, 7). Similar findings have been reported in sleeping normal humans under normocapnic conditions, but hypoventilation was observed when Pa^sub CO2^ was allowed to fall (1). Nevertheless, apnea was observed infrequently, suggesting that STP activation minimized the hypocapnic inhibition. This is supported by the fact that apnea consistently occurred after passive hypocapnic hyperventilation, which is not associated with STP activation (8).
STP is a neural mechanism that is located in the brain stem and is activated by a variety of stimuli (5, 8). STP once activated is able to drive ventilation for some time independent of peripheral and central afferents. It has been proposed that STP is an important factor promoting ventilatory stability (9). According to this hypothesis, the activation of STP during hyperventilation would preclude an appreciable ventilatory undershoot later, aborting thus the ventilatory oscillation. Conversely, periodic breathing would be promoted if STP was absent or reduced. This hypothesis is supported by studies in animals and humans (10-12). In mice that genetically were not able to exhibit STP (13), unstable breathing was triggered when brief hypocapnic hypoxia was terminated abruptly (12). Patients with periodic breathing such as those with sleep apnea syndrome (10) or brain damage (11) do not exhibit poststimulus potentiation of ventilation after brief hypoxia, indicating a reduced STP activation. It is of interest to note that in patients with brain damage, a relationship was observed between the ventilatory response pattern after hypoxia and breathing stability during room air breathing. Indeed, the tendency to exhibit periodic breathing was associated with greater posthypoxic ventilatory inhibition (11).
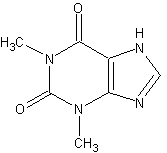
It has been shown in patients with periodic breathing that administration of theophylline (an adenosine antagonist at therapeutic doses) alleviated Cheyne-Stokes respiration and central apneas (14-17). This beneficial effect of theophylline has been observed in premature infants (15) and in adult patients with ischemic stroke (14) or congestive heart failure (17). However, the mechanism underlying the effect of theophylline on breathing stability is not known. It is possible that theophylline may influence STP and promote ventilatory stability through this mechanism. The aim of this study was to investigate the effect of theophylline on STP in patients with brain damage by examining ventilatory responses to acute hyperoxia after brief exposure (45 seconds) to hypocapnic hypoxia with and without pretreatment with theophylline. We hypothesized that pretreatment with theophylline may restore STP activation, thus preventing the posthypoxic hyperoxic ventilatory depression observed in this group of patients (11). In addition the effect of theophylline on posthypoxic hyperoxic ventilation was further studied in a group of normal adults. Some of the results of this study have been previously reported in the form of an abstract (18).
METHODS
Eight stable patients with brain damage were studied (see Table E1 in the online supplement). The study was approved by the hospital ethics committee, and informed consent was obtained from patients' family. The apparatus used for the hypoxic-hyperoxic ventilatory responses has been fully described in previous reports (4, 19).
Each patient was studied on two occasions on nonconsecutive days. In the morning of each study day, normal saline (placebo) or theophylline was administered in a randomized double-blind manner. A blood sample was drawn at the end of the experiment to determine blood theophylline levels.
After 2 hours of continuous infusion of placebo or theophylline, the patients breathed room air until end-tidal P^sub CO2^ and ventilation stabilized. During this period, arterial blood gasses were measured. Then the inspirate was changed to nitrogen for three breaths during which end-tidal O2 decreased rapidly to less than 60 mm Hg. The inspirate was then switched to 8.5% O2, which maintained end-tidal P^sub O2^ at approximately 45 mm Hg for a total of 40 seconds. During the last 5 seconds of hypoxia arterial blood was drawn for Pa^sub O2^ and Pa^sub CO2^ determination. Hypoxia was terminated abruptly by switching to O2, whereas hyperoxia was sustained for 2 minutes. On each study day, four hypoxic-hyperoxic trials were performed in each patient. Furthermore, in each patient on both study days, the effect of switching the inspirate from room air to O2 was tested. On each study day, two normoxic-hyperoxic trials were performed in each patient. In all of these experiments, no attempt to control end-tidal P^sub CO2^ was made.
The control group consisted of 10 normal adults (eight males and two females, mean age of 31). Similar to patients, the normal adults were studied with and without pretreatment with theophylline in an identical manner. Arterial blood gasses were not measured in this group. In these experiments, a supplemental source of CO2 was attached to the inspiratory limb of the breathing circuit to allow titration of inspired CO2 concentration. On each study day, three hypocapnic and three isocapnic hypoxic-hyperoxic runs were performed in each subject using the same method as described previously here.
Tidal volume, inspiratory and expiratory time, end-tidal P^sub CO2^ and P^sub O2^ were measured breath by breath for 1 minute before hypoxia baseline, during hypoxia, and for 2 minutes after switching to O2. All breaths during hypoxia and hyperoxia were expressed as a percentage of mean baseline values. Breaths during the first 7 seconds of all hyperoxic exposures were assumed to be influenced by hypoxic or normoxic blood perfusing the peripheral chemoreceptors due to a 6- to 8-second circulation delay between the lung and carotid bodies (20, 21). These breaths were averaged to give a single value. Thereafter, ventilation was averaged breath by breath (first hyperoxic breath after 7 seconds of hyperoxia, second hyperoxic breath after 7 seconds of hyperoxia, etc.) and plotted as a function of time. The posthypoxic hyperoxic ventilatory decline was analyzed, up to the point that ventilation started to increase steadily, as an exponential of the form Vt = V^sub L^ + Ae^sup (-t/[tau])^, where Vt was ventilation at time t of hyperoxia (after the first 7 seconds of hyperoxia). V^sub L^ was ventilation at the lower asymptote. A was a constant, and [tau] was the time constant of the decay (see Figure E1 in the online supplement).
To compare ventilatory parameters in a given time of hyperoxia with and without theophylline, the results for all trials in a given patient or subject were averaged at 5-second intervals, the individual values being obtained by linear interpolation between the adjoining breaths (10, 11).
Data were analyzed by paired t-test, multifactorial analysis of variance, and nonparametric Mann-Whitney U test, when appropriate. A value of p
RESULTS
At the end of the theophylline protocol, the mean serum theophylline for the group of patients was 12.3 + or - 1.3 mg/L. In six patients, blood levels of theophylline were between 10 to 17 mg/L, whereas in two, they ranged between 7 and 8 mg/L. In normal subjects, the corresponding blood levels of theophylline was 16.8+ or -2.2 mg/L. With placebo in both groups, theophylline blood levels were undetectable. There were no side effects from the drug infusion. Breath by breath changes in Sa^sub O2^ is not reported because of the slow response of the oximeter. In both patients and normal subjects, the lowest value of Sa^sub O2^ was observed several seconds (more than 15-20 seconds) after switching the inspirate to hyperoxia.
Patients with Brain damage
The patients were studied 101 + or - 9 days after injury. In all patients, the findings of the computed tomography scan were compatible with moderate to severe brain damage.
In each study day (theophylline or placebo), two hypoxic-hyperoxic and two normoxic-hyperoxic runs were analyzed in a given patient (for the group a total of 32 hypoxic-hyperoxic and 16 normoxic-hyperoxic runs were analyzed). Mean room air (baseline) and end-hypoxic values of ventilation, breathing patterns, and Pa^sub CO2^ with and without theophylline are shown in Table 1. With theophylline, baseline ventilation was slightly higher than that with placebo, mainly due to higher breathing frequency. As a result, Pa^sub CO2^ was lower with theophylline. These changes, however, were not significant. Independent of pretreatment when hypcroxia followed room air breathing, ventilation did not exhibit any appreciable immediate undershoot and remained close to normoxic baseline throughout the hyperoxic exposure. On both study days at the end of hypoxia, ventilation and tidal volume increased, and total breath duration decreased significantly (Table 1). The hypoxic ventilatory response, expressed as a percentage of baseline, did not differ between placebo and theophylline days. At the end of hypoxia, Pa^sub O2^ did not differ between study days, whereas Pa^sub CO2^ was significantly lower with theophylline than that with placebo (Table 1).
During the various study periods (baseline, end of hypoxia) end-tidal P^sub CO2^ was approximately 2 to 3 mm Hg lower than the corresponding Pa^sub CO2^ Breaths with low tidal volume were associated with very low level of end-tidal P^sub CO2^, presumably because of the inability of the expired gas to displace the dead space fully, making use of end-tidal P^sub CO2^ to infer changes in blood Pa^sub CO2^, unreliable (22). This usually occurred when hyperoxia followed hypoxia. For this reason and for clarity of presentation, breath by breath end-tidal P^sub CO2^ values are not reported. Pa^sub CO2^ at the end of hypoxia was served as an index of the magnitude of hypocapnia at the beginning of hyperoxia.
With and without pretreatment with theophylline, the ventilalory hypoxic increase was maintained on average for the first 7 seconds of hyperoxia, ventilation during this time averaging with and without theophylline 1.40.2 + or - 11% and 147.6 + or - 5% of baseline, respectively (Figure 1). Thereafter, ventilation declined with a pattern that was clearly different between placebo and theophylline days (Figures 1 and 2). In all patients, the posthypoxic hyperoxic ventilatory decay followed an exponential course with an rvalue ranging between 0.92-0.99. Individual parameters of ventilatory decay as derived from Equation 1 are shown in Table 2. Although with theophylline ventilation decreased to values that were significantly higher than those with placebo, the lime constant of ventilatory decay was 38% longer than placebo. Figure 1 shows at 5-second intervals the mean hyperoxic ventilation, tidal volume, and expiratory time when hyperoxia followed hypoxia. With placebo, ventilation, after correction for circulatory delay, dropped immediately to 70% of baseline, reaching a nadir value of 62% during the fourth 5-second interval. With theophylline, ventilation, after correction for circulatory delay, remained at 125% of baseline reaching a nadir value of 94% during the fourth 5-second interval. This effect of theophylline on posthypoxic hyperoxic ventilatory inhibition was due to a combined action on expiratory time and tidal volume. With placebo in 19 out of 32 hypoxic-hyperoxic trials (59%) breaths with expiratory time greater than 200% (defined as apneas) of baseline were observed. With theophylline, only 7 out of 32 hypoxic-hyperoxic trials (22%) were associated with such breaths (p
Normal Subjects
In each study day, 30 hypocapnic (three in each subject) and 30 isocapnic (three in each subject) hypoxic-hyperoxic runs were analyzed. With theophylline baseline ventilation was significantly higher than that with placebo (10.1 + or - 0.6 vs. 8.9 + or - 0.4 L/min). As a result, baseline end-tidal P^sub CO2^ was slightly but significantly lower with theophylline than that with placebo (34.1 + or - 1.1 vs. 36.3 + or - 1.0 mm Hg). With placebo, at the end of hypoxia, ventilation increased by 55 + or - 5% and 72 + or - 8%, respectively, in hypocpnic and isocapnic runs, whereas with theophylline the corresponding values were 60 + or - 8% and 75 + or - 9%. The magnitude of hypoxic ventilatory increase did not differ between theophylline and placebo. At the end of hypocapnic hypoxia, end-tidal P^sub CO2^ dropped by 7.9 + or - 2.5% and 8.4 + or - 2.6% of baseline, respectively, with placebo and theophylline. Abrupt termination of hypocapnic or isocapnic hypoxia by hyperoxia was associated with a slow ventilatory decay to baseline without a significant undershoot (Figure 3). No apneas were observed. In all subjects, the hyperoxic ventilatory decline followed an exponential pattern (r > 0.90). For a given hypoxic condition (hypocapnic or isocapnic), the pattern of ventilatory decay did not differ significantly between theophylline and placebo (Table 3). Compared with hyperoxia after hypocapnic hypoxia, the ventilatory decay followed a significantly slower pattern when hyperoxia followed isocapnic hypoxia (Table 3). In normal subjects, V^sub L^ was significantly higher, and T [tau] was significantly longer than the corresponding values in patients with brain damage (Mann-Whitney nonparametric U test).
DISCUSSION
A group of patients with moderate to severe brain damage were studied as indicated by their low Glasgow coma scores and computed tomography findings. On both study days with room air, all patients breathed at a faster rate than normal (more than 17 breaths per minute). We carefully excluded patients with hypoxemia or any evidence of pulmonary or cardiovascular disease, and thus, the breathing pattern that we observed most likely was due to the loss of cortical influences on ventilatory centers (23). All, patients and normal subjects, achieved blood theophylline levels that have been shown to promote breathing stability (17).
Our apparatus was designed to achieve rapid changes in alveolar P^sub O2^. In all conditions, end-tidal P^sub O2^ at the end of the first hyperoxic breath was at or above the normoxic baseline, and that of the second was above 120 mm Hg. Given a normal lung-carotid circulation time of 6-8 seconds (20, 21), it is reasonable to assume that the hypoxic stimulus, at least with placebo, was withdrawn about 7 seconds after switching to hyperoxia. It is possible that theophylline decreased the circulation delay by increasing both the ejection fraction of the left ventricle and the heart rate. Nevertheless, this effect in patients with normal cardiovascular system is minimal (24) and if any, all the other being equal, should result in hypoventilation earlier in hyperoxia. This was not the case, and a significant hyperventilation was observed both in normal subjects and patients during the first 7 seconds of hyperoxia with and without theophylline. Thus, although the real time required in each patient or subject for complete withdrawal of any residual hypoxic drive was not known, we believe that the assumption of a similar circulation delay between study days is valid and supported by the breathing pattern immediately upon transition from hypoxia to hyperoxia.
In the patients, when theophylline was infused, Pa^sub CO2^ during baseline and at the end of hypoxia was slightly lower than it was with placebo because of higher minute ventilation. The lower Pa^sub CO2^ with theophylline made comparisons between placebo and theophylline days difficult. For example, the hypoxic ventilatory response may have been affected by differing baseline Pa^sub CO2^ levels. On the other hand, the lower Pa^sub CO2^ during the theophylline infusion did not weaken analyses of changes in ventilation when hyperoxia followed hypoxia. Indeed, the lower Pa^sub CO2^ with theophylline at the end of hypoxia may have increased the effectiveness of the functional chemodenervation achieved with hyperoxia (25), making the effect of inhibitory influences of hypocapnia on ventilation more prominent. Similar arguments apply also in normal subjects in whom end-tidal P^sub CO2^ was served as an index of CO2 stimulus.
Theoretically, for a given Pa^sub CO2^, medullary P^sub CO2^ should be higher with theophylline than that with placebo because of theophylline-induced cerebral vasoconstriction (26, 27). However, the effect of cerebral vasoconstriction on medullary P^sub CO2^ is greatly minimized by the concomitant decrease in brain P^sub O2^ permitting the blood to carry more CO2 for a given P^sub CO2^ (Haldane effect). Indeed, it has been shown in normal adults that theophylline infusion was associated with a significant decrease in jugular P^sub O2^, whereas the jugular P^sub CO2^, an index of medullary P^sub CO2^, remained constant (27). Nevertheless, in our study, ventilatory parameters were expressed as the percentage of baseline value of a given study day, thus taking into account any difference in baseline medullary P^sub CO2^. On the other hand, theophylline at therapeutic doses does not affect the hypoxic increase in cerebral blood flow; hypoxia with and without theophyllinc lowers jugular P^sub CO2^ to a similar magnitude (26, 27). Although cerebral blood flow was not measured, the patients were studied several months after the primary event when they were stable with normal intracranial and cerebral perfusion pressure, indicating that cerebral blood vessels most likely responded with the usual pattern to hypoxia (vasodilation) and hyperoxia (vasoconstriction) (28). It has been shown that patients with brain damage have impaired autoregulation of cerebral vessels in the first 2 days after injury, but they regain the normal cerebral vasoreactivity 1 week latter if they will survive (28). It follows that compared with baseline, with and without theophylline, medullary P^sub CO2^ should decrease during hypoxia. Thus, independent of the study day when peripheral chemoreccplors were turned off by hyperoxia, the CO2 stimulus at the central level (medullary P^sub CO2^) should be lower than that with room air.
Our results in brain-damage patients showed that with placebo abrupt cessation of hypoxic stimulus resulted in a considerable drop of ventilation below the normoxic baseline. The mean group hyperoxic ventilation decreased to 70% of baseline 7 seconds after hypoxia and reached a nadir value (62%) at about 25 seconds of hyperoxia. The ventilatory inhibition was due to prolongation of expiratory time and, to a lesser extent, to a tidal volume decrease. This response pattern was presumably due to hypocapnic inhibition. The relatively greater change and the response pattern of expiratory time indicate that at least in some patients Pa^sub CO2^ dropped below the apneic threshold (29,30). These results are similar to those reported by Georgopoulos and colleagues (11) also in patients with brain damage. Furthermore, this study showed that this posthypoxic hyperoxic breathing pattern was significantly altered by pretreatment with theophylline, which largely prevented the posthypoxic hyperoxic depression of ventilation. With theophylline, ventilation expressed as percentage of normoxic baseline was significantly higher than that with placebo for 25 seconds after the estimated circulatory delay. This effect of theophylline was due both to expiratory time and tidal volume changes.
In normal subjects with placebo when hyperoxia followed isocapnic hypoxia, ventilation declined gradually to levels that were slightly higher than the baseline. A similar pattern was observed when hyperoxia followed hypocapnic hypoxia, although the ventilatory decay followed a more rapid course. These findings are similar to those reported previously in normal young and older adults (4, 19, 31). We have interpreted this gradual decline in ventilation as indicative of STP or afterdischarge. Theophylline did not change this response pattern. This suggests that either the lower CO2 stimulus at the end of hypoxia when theophylline was infused or a saturation of STP mechanism activated by a certain degree of hypoxia might be responsible for the failure of theophylline to significantly influence the posthypoxic hyperoxic ventilation in normal subjects. Although theoretically raising the baseline end-tidal P^sub CO2^ by increasing the inspired CO2 when theophylline was infused could resolve this issue, the achievement of steady state with increasing inspired CO2 may take several hours, and this may considerably influence the ventilatory changes (32).
An effect of theophylline on the apnea threshold could also explain the results of our study (33). If theophylline shifted the apneic threshold to lower value then when hypoxia was terminated by hyperoxia, the undershoot of ventilation should be lower. The effect of theophylline on apneic threshold is not known. However, studies indicate that this should be small, if any. Indeed, it has been demonstrated that theophylline did not affect either the intercept of the extrapolation of hypercapnic ventilatory response to zero ventilation (an index of apneic threshold) or the slope of the hypercapnic ventilatory response (34). Notwithstanding the uncertainty of extrapolation the ventilatory response to CO2 to below eupnea and that normal subjects were studied (34), these findings indicate that theophylline does not alter the CO2-mediated ventilatory control, rendering the likelihood of a selective action of theophylline on apneic threshold rather unlikely. However, the possibility remains that the posthypoxic hyperoxic ventilatory depression observed with placebo was due to relatively high apnea threshold (close to PCO2 during normoxia), and theophylline decreased to some extent this threshold. Under this circumstance, the activation of STP was unmasked by theophylline, resulting in a posthypoxic ventilatory response pattern that resembled that observed in normal subjects. The design of our study does not permit further clarification of this issue.
In a previous study, we reasoned that in patients with brain damage, an impairment of STP activation is the most plausible explanation for the considerable ventilatory depression observed when hyperoxia followed hypoxia (11). Because ventilation after withdrawal of hypoxia is determined by the relative strength of inhibitory and excitatory influences, the prevention of ventilatory depression with theophylline in patients with brain damage indicates that either the inhibitory influences are decreased or STP activation is increased (or unmasked). Potential inhibitory influences operating at the beginning of hyperoxia after hypoxia are hypocapnia at the peripheral and central levels (1), a memory of vagally mediated mechanoreceptor feedback due to tidal volume increase during hypoxia (3) and central hypoxic depression secondary to accumulation of neurolransmitter (i.e., adenosine) (35). On both study days, central hypoxic depression is unlikely to play a significant role because of the brief duration of hypoxia (4). In addition, central hypoxic depression is associated with reduced ventilatory response (4), and hypoxic responses in this group of patients were within the normal range (10). At the end of hypoxia, the fall in PaCO2 was greater with theophylline than that with placebo, whereas the increase in tidal volume was comparable between study days. Thus, with theophylline, the inhibitory influences were greater or at least comparable to these with placebo. It follows that the observed changes in hyperoxic ventilation with theophylline should be due either to an increase in activation of STP during the brief hypoxic exposure or to a decrease in the relatively high apneic threshold that unmasked the STP activation. Although the exact mechanism through which the theophylline influences STP is difficult to be elucidated, the adenosine-blocker mode of action of the drug might be involved, as it is the case with the stimulating effect of the drug on resting ventilation (36). However, an effect of theophylline on higher cortical centers, which have been shown to influence posthypoxic hyperoxic ventilation and therefore the STP expression (1, 37), could also explain the results of our study. This, however, is unlikely to occur because the Glasgow Coma Scale did not differ between study days and there was no any clinical indication of a cortical function change throughout the experiments. Finally, theophylline may exert its effect on posthypoxic hyperoxic ventilation by modifying the S-nitrosothiols biochemistry of the nucleus tractus solitarii (38, 39). Recent data have shown that the changes in ventilation during and after hypoxia are signaled at the level of nucleus tractus solitarii by deoxyhemoglobin-derived S-nitrosothiols (38, 39). Further studies are needed to clarify the pathway through which theophylline could influence STP.
Both in normal subjects and patients with theophylline, resting ventilation was slightly higher, indicating a higher level of baseline central nervous system ventilatory activity, and this may affect the posthypoxic ventilatory changes. In normal subjects, however, posthypoxic hyperoxic ventilation did not differ with and without theophylline, In addition, we have shown that almitrine, a drug that is associated with a comparable increase in resting ventilation did not affect the posthypoxic hyperoxic ventilation (19). These data indicate that changes in resting ventilation, at least in the range observed in our study, may not be an important determinant of ventilatory poststimulus potentiation.
Previous studies have shown that patients with periodic breathing such as those with sleep apnea syndrome or brain damage exhibit an immediate ventilatory depression after brief hypoxia indicating a reduced STP activation (10, 11). In patients with brain damage, a relationship between spontaneous periodic ventilation and STP activation was demonstrated (11). Similar results have been recently published in mice that have genetically a defect in STP activation (12, 13). Collectively, the results of these studies are in accordance with the hypothesis suggesting that STP is an important factor promoting ventilatory stability (9). This study clearly demonstrated that pretreatment with theophylline almost abolished the posthypoxic hyperoxic hypoventilation, most probably by restoring STP activation. These results are qualitatively similar to those reported by Georgopoulos and colleagues (35) in normal adults when sustained (20 minutes) isocapnic hypoxia (a condition that is likely associated with impairment of STP activation) (1, 4, 40) was followed by hyperoxia. However, this study was not designed to examine STP, whereas hyperoxia was introduced in a rather slow manner (35). Notwithstanding these limitations, these results (35) combined with those of this study suggest that theophylline may restore STP activation independent of the cause of its impairment.
In patients, we did not attempt to maintain isocapnic conditions during hypoxia because we believe that end-tidal PCO2 was not a reliable index of CO2 stimulus at presence of high breathing frequency and low tidal volume (22). Under this circumstance, maintaining constant end-tidal PCO2 breath by breath may overestimate or underestimate the actual PaCO2 making the interpretation of changes in ventilation difficult. This however, should affect neither the interpretation nor the conclusion of our study. When hyperoxia followed hypocapnic hypoxia, CO2 stimulus was considerably lower with theophylline than that with placebo, resulting in a relative underestimation of the STP activation.
Although theophylline significantly attenuated the posthypoxic hyperoxic drop of ventilation in patients with brain damage, the ventilatory decline followed a different pattern than that observed in normal subjects after hypocapnic hypoxia. Indeed, the ventilatory decline followed a more rapid course to levels that were considerably lower. This could be due to the loss of cortical influence in patients with brain damage. This situation may resemble that during non-rapid eye movement (NREM) sleep in which the influence of hypocapnia may cause a modest ventilatory inhibition in normal subjects when brief hypocapnic hypoxia is terminated abruptly by hyperoxia (1). However, a partial restoration of STP activation by theophylline might also play a role.
The effect of theophylline on posthypoxic hyperoxic ventilation may elucidate the mechanism through which the drug exerts its beneficial effect on periodic breathing, observed in susceptible neonates as well as in adults (14-17). By preventing a drop in ventilation brought by the hyperventilation-induced hypocapnia, the swings in PCO2 would be minimized leading to a decrease tendency to periodic breathing. It is possible that theophylline may decrease the periodic breathing through other than STP mechanisms. For example, in patients with congestive heart failure, theophylline therapy may alleviate Cheyne-Stokes breathing by decreasing the circulatory delay. Nevertheless, the effect of theophylline on cardiac function is not well established (24, 41). On the other hand Javaheri and colleagues (17) have shown in patients with stable heart failure that theophylline therapy reduced the number of episodes of apnea and hypopnea during sleep without affecting the right and left ventricular ejection fractions, suggesting that the observed decrease in periodic breathing was not related to cardiac function changes. Similarly, in patients with normal cardiovascular system and periodic breathing, the effect of theophylline on breathing stability is unlikely to be mediated by changes in cardiac output. Indeed, in these patients, the circulation delay is relatively short, and thus, it is not considered to be a strong destabilizing factor (9).
Our study does not intend to recommend theophylline as a standard treatment for patient with brain damage. Although theophylline could prevent life-threatening periodic breathing in patients with ischemic stroke (14), this therapy may be associated with lessening the threshold for seizures, a side effect with considerable morbidity and mortality (42). In addition the theophylline-induced cerebral vasoconstriction and the associated decrease in the oxygen delivery (26, 27) should not be ignored in some clinical settings. Further studies are needed to address the potential clinical implication of long-term theophylline therapy in patients with brain damage.
References
1. Badr MS, Skatrud JB, Dempsey JA. Determinants of poststimulus potentiation in humans during NREM sleep. J Appl Physiol 1992;73:1958-1971.
2. Xi L, Smith CA, Saupe KW, Dempsey JA. Effects of memory from vagal feedback on short-term potentiation of ventilation in conscious dogs. J Physiol 1993;462:547-561.
3. Leevers AM, Simon PM, Xi L, Dempsey JA. Apnoea following normocapnic mechanical ventilation in awake mammals: a demonstration of control system inertia. J Physiol 1993:472:749-768.
4. Georgopoulos D, Bshouty Z, Younes M, Anthonisen NR. Hypoxic exposure and activation of the afterdischarge mechanism in conscious humans. J Appl Physiol 1990;69:1159-1164.
5. Eldridge FE, Gill-Kumar P. Central neural respiratory drive and afterdischarge. Respir Physiol 1980;40:49-63.
6. Engwall MJ, Daristotle E, Niu WZ, Dempsey JA, Bisgard GE. Ventilatory afterdischarge in the awake goat. J Appl Physiol 1991;71:1511-1517.
7. Fregosi RF. Short-term potentiation of breathing in humans. J Appl Physiol 1991;71:892-899.
8. Eldridge FE. Posthyperventilation breathing: different effects of active and passive hyperventilation. J Appl Physiol 1973:34:422-430.
9. Younes M. The physiological basis of central apnea and periodic breathing. Curr Pulmonol 1989;10:265-326.
10. Georgopoulus D, Giannouli E, Tsara V, Argiropoulou P, Patakas D, Anthonisen NR. Respiratory short-term poststimulus potentiation (after-discharge) in patients with obstructive sleep apnea. Am Rev Respir Dis 1992;146:1250-1255.
11. Georgopoulos D, Mitrouska I, Koletsos K, Markopoulou K, Riggos D, Patakas D, Anthonisen NR. Ventilatory post-stimulus potentiation in patients with brain damage. Am J Respir Crit Care Med 1995;152:1627-1632.
12. Han F, Subramanian S, Price ER, Nadeau J, Strohl KP. Periodic breathing in the mouse. J Appl Physiol 2002;92:1133-1140.
13. Han F, Subramanian S, Dick TE, Dreshaj IA, Strohl KP. Ventilatory behavior after hypoxia in C57BL/6J and A/J mice. J Appl Physiol 2001;91:1962-1970.
14. Nachtmann A, Siebler M, Rose G, Sitzer M, Steinmetz H. Cheyne-Stokes respiration in ischemic stroke. Neurology 1995;45:820-821.
15. Paky F, Donath P, Huebmer E, Stogmann W. Theophylline for infants with abnormal pneumographic results: a randomized double blind, placebo-controlled trial. Klin Padiatr 1997;209:66-70.
16. Pesek CA, Cooley R, Narkiewicz K, Dyken M, Weintraub NE, Somers VK. Theophylline therapy for near-fatal Cheyne-Stokes respiration: a case report. Ann Intern Med 1999;130:427-430.
17. Javaheri S, Parker TJ, Wexler L, Liming JD, Lindower P, Roselle GA. Effect of theophylline on sleep-disordered breathing in heart failure. N Engl J Med 1996;335:562-567.
18. Mitrouska I, Kondili E, Prinianakis G, Michelaki E, Siafakas N, Georgopoulos D. Effects of aminophlline on ventilatory post-stimulus potentiation in patients with brain damage [abstract]. Am J Respir Crit Care Med 2002;165:A668.
19. Georgopoulos D, Mitrouska I, Argyropoulou P, Patakas D, Anthonisen NR. Effect of hypoxic sensitivity on decay of respiratory short-term potentiation. Chest 1995;107:150-155.
20. Khoo MC, Kronauer RE, Strohl KP, Slutsky AS. Factors inducing periodic breathing in humans: a general model. J Appl Physiol 1982;53:644-659.
21. Lange RL, Horgan JD, Botticelli JT, Tsagaris T, Carlisle RP, Kuida H. Pulmonary to arterial circulatory transfer function: importance in respiratory control. J Appl Physiol 1966;21:1281-1291.
22. Clark JS, Votteri B, Ariagno RL, Cheung P, Eichhorn JH, Fallat RJ, Lee SE, Newth CJ, Rotman H, Sue DY. Noninvasive assessment of blood gases. Am Rev Respir Dis 1992;145:220-232.
23. Plum FL, Leight RJ. Abnormalities of central mechanism. In: Hornbein TF, editor. Lung biology in health and disease: regulation of breathing, vol. 17. New York: Marcel Dekker; 1981. p. 981-1067.
24. Conradson TB. Bronchodilating plasma concentrations of enprofylline and theophylline have minor cardiovascular effects in man. Acta Pharmacol Toxicol (Copenh) 1986;58:204-208.
25. Lambertsen CJ. Chemical control of respiration at rest. In: Mountcastle VB, editor. Medical physiology, 14 ed, vol 2. St. Louis: Mosby; 1980. p. 1775-1829.
26. Bowton DL, Haddon WS, Prough DS, Adair N, Alford PT, Stump DA. Theophylline effect on the cerebral blood flow response to hypoxemia. Chest 1988;94:371-375.
27. Nishimura M, Yoshioka A, Yamamoto M, Akiyama Y, Miyamoto K, Kawakami Y. Effect of theophylline on brain tissue oxygenation during normoxia and hypoxia in humans. J Appl Physiol 1993;74:2724-2728.
28. Czosnyka M, Smielewski P, Kirkpatrick P, Menon DK, Pickard JD. Monitoring of cerebral autoregulation in head-injured patients. Stroke 1996;27:1829-1834.
29. Skatrud JB, Dempsey JA. Interaction of sleep state and chemical stimuli in sustaining rhythmic ventilation. J Appl Physiol 1983;55:813-822.
30. Xie A, Skatrud JB, Puleo DS, Rahko PS, Dempsey JA. Apnea-hypopnea threshold for CO2 in patients with congestive heart failure. Am J Respir Crit Care Med 2002;165:1245-1250.
31. Ahmed M, Giesbrecht GG, Serrette C, Georgopoulos D, Anthonisen NR. Respiratory short-term potentiation (after-discharge) in elderly humans. Respir Physiol 1993;93:165-173.
32. Reynolds WJ, Milhorn HT Jr, Holloman GH Jr. Transient ventilatory response to graded hypercapnia in man. J Appl Physiol 1972;33:47-54.
33. Nakayama H, Smith CA, Rodman JR, Skatrud JB, Dempsey JA. Effect of ventilatory drive on carbon dioxide sensitivity below eupnea during sleep. Am J Respir Crit Care Med 2002;165:1251-1260.
34. Griffiths TL, Christie JM, Parsons ST, Holgate ST. The effect of dipyridamole and theophylline on hypercapnic ventilatory responses: the role of adenosine. Eur Respir J 1997;10:156-160.
35. Georgopoulos D, Holtby SG, Berezanski D, Anthonisen NR. Aminophylline effects on ventilatory response to hypoxia and hyperoxia in normal adults. J Appl Physiol 1989;67:1150-1156.
36. Eldridge FL, Millhorn DE, Waldrop TG, Kiley JP. Mechanism of respiratory effects of methylxanthines. Respir Physiol 1983;53:239-261.
37. Chin K, Ohi M, Fukui M, Kita H, Tsuboi T, Noguchi T, Otsuka N, Hirata H, Mishima M, Kuno K. Inhibitory effect of an intellectual task on breathing after voluntary hyperventilation. J Appl Physiol 1996;81:1379-1387.
38. Lipton SA. Physiology: nitric oxide and respiration. Nature 2001;413:118-119, 121.
39. Lipton AJ, Johnson MA, Macdonald T, Lieberman MW, Gozal D, Gaston B. S-nitrosothiols signal the ventilatory response to hypoxia. Nature 2001;413:171-174.
40. Jubran A, Tobin MJ. Effect of isocapnic hypoxia on variational activity of breathing. Am J Respir Crit Care Med 2000;162:1202-1209.
41. Esquivel M, Burns RJ, Ogilvie RI. Cardiovascular effects of enprofylline and theophylline. Clin Pharmacol Ther 1986;39:395-402.
42. Turski WA, Cavalheiro EA, Ikonomidou C, Mello LE, Bortolotto ZA, Turski L. Effects of aminophylline and 2-chloroadenosine on seizures produced by pilocarpine in rats: morphological and electroencephalographic correlates. Brain Res 1985;361:309-323.
Ioanna Mitrouska, Eumorfia Kondili, George Prinianakis, Nickolaos Siafakas and Dimitris Georgopoulos
Department of Intensive Care Medicine and Department of Thoracic Medicine, University Hospital of Heraklion, University of Crete, Heraklion, Crete, Greece
(Received in original form June 73, 2002; accepted in final form January 10, 2003)
Correspondence and requests for reprints should be addressed to Dimitris Georgopoulos, M.D., University Hospital of Heraklion, University of Crete, Heraklion, 711 10, Crete, Greece. E-mail: georgop@med.uoc.gr
This article has an online supplement, which is accessible from the issue's table of contents online at www.atsjournals.org
Am J Respir Crit Care Med Vol 167. pp 1124-1130, 2003 Originally Published in Pressas DOI: 10.1164/rccm.200206-552OC on January 16, 2003 Internet address: www.atsjournals.org
Copyright American Thoracic Society Apr 15, 2003
Provided by ProQuest Information and Learning Company. All rights Reserved